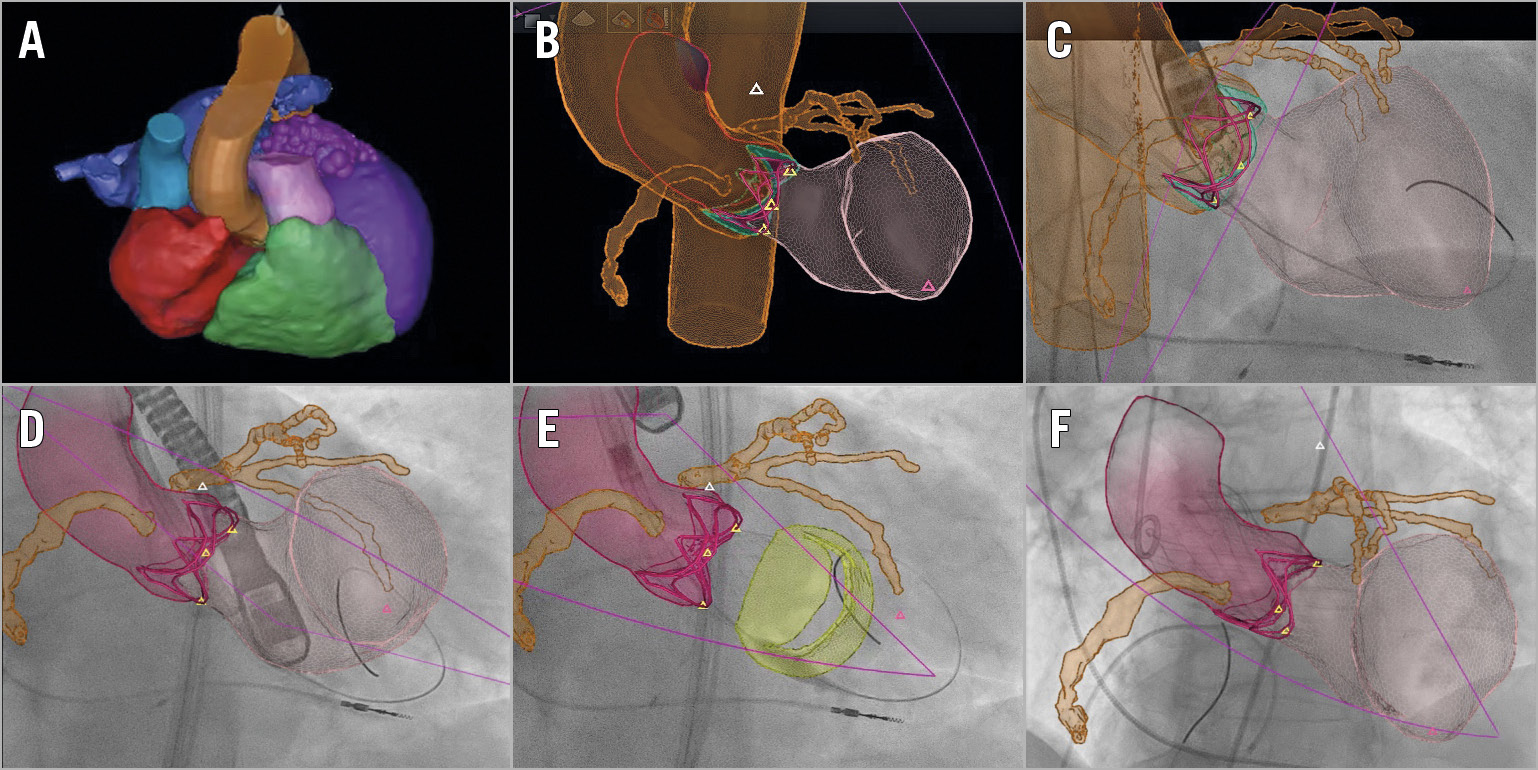
Figure 1. Fusion model during the procedure. A) Model after segmentation of preprocedural MSCT. B) Matched 3D-TEE and MSCT segmentation. Orange: coronary arteries and aorta. Pink: left ventricle. C) Pre-implantation verification with small contrast injection. D) Optimal implantation depth localisation. E) Checking possible interference of the prosthetic valve with the mitral valve (yellow). F) Post-implantation verification with small contrast injection.
Several tools have been developed in order to optimise transcatheter aortic valve implantation (TAVI) procedures and decrease the risk of procedural complications such as acute kidney injury. Real-time fusion of 3D multislice computed tomography (3D-MSCT) images with X-ray fluoroscopy may help physicians during the procedure1. However, these still MSCT images cannot be matched with X-ray fluoroscopy without the use of contrast injection1. We describe the first use of a new, fully automatic, 3D transoesophageal echocardiography (TEE)-based fusion technique of 3D-MSCT on live fluoroscopy during TAVI.
An 85-year-old woman, with severe symptomatic aortic valve stenosis and renal impairment (estimated glomerular filtration rate [eGFR] 44 ml/min/1.73 m2) underwent TAVI with a self-expanding valve.
Preprocedurally, the HeartNavigator (Philips Healthcare, Best, the Netherlands) was used for automatic localisation and segmentation of all anatomical structures of the heart on MSCT (Figure 1A).
Procedural 3D-TEE was automatically processed over the entire cardiac cycle, resulting in a 4D segmentation model of the heart. The EchoNavigator (Philips Healthcare) was used to overlay this TEE-based heart segmentation on top of live fluoroscopic images. As the MSCT segmentation and 3D-TEE segmentation of the heart originate from a similar model-based segmentation algorithm and are performed on the same patient, an automatic point-based 3D-3D rigid registration algorithm can be used to register the MSCT segmentation to live fluoroscopy via the registered 3D-TEE segmentation. For each segmented 3D-TEE frame in the heartbeat, the best matching MSCT registration was selected as the most optimal registration (Figure 1B).
We verified the fusion model’s anatomical precision of the aortic annulus with contrast injection before (Figure 1C, Moving image 1, Moving image 2) and after valve deployment (20 ml contrast in total), which was accurate (Figure 1C, Figure 1F, Moving image 3). The valve was correctly implanted, without paravalvular leakage (Figure 1D-Figure 1F).
This new fusion technique provides ultimate flexibility in live image fusion and has several advantages: 1) overlay of MSCT data without the use of contrast medium, which makes zero contrast procedures possible; 2) MSCT data add complementary information to the ultrasound overlay; and 3) MSCT data have a larger view than echo. Further testing of this technology in terms of accuracy and efficacy is necessary, especially in more complex procedures.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Verification of the fusion model with contrast injection pre implantation.
Moving image 2. Verification of the fusion model with contrast injection during valve implantation.
Moving image 3. Verification of the fusion model with contrast injection post implantation.