Transcatheter interventions for valvular heart disease have become a feasible alternative to surgical valve repair and replacement in patients at increased risk or with contraindications for surgery. More than 200,000 patients with severe aortic stenosis have been treated worldwide with transcatheter aortic valve implantation (TAVI), and more than 30,000 patients with severe mitral regurgitation have undergone transcatheter edge-to-edge mitral valve repair1,2. Meanwhile, first-in-man experiences with percutaneous treatment of severe tricuspid valve regurgitation have been published3, and percutaneous techniques for pulmonary valve implantation and treatment of degenerated bioprostheses or failing mitral or tricuspid ring annuloplasty are now routine treatment options for specific patient subgroups4. Advances in three-dimensional (3D) imaging techniques have underpinned these interventional developments.
As a consequence, imaging cardiologists and interventionists have learnt to speak a common language to understand mutually the underlying mechanisms of valve dysfunction, select the patients who may benefit from transcatheter therapies, and guide the procedures. Interventionists are familiar with fluoroscopic cardiac anatomy and use an attitudinal terminology to locate and manipulate catheters in relation to the valve of interest5. In contrast, imaging cardiologists are familiar with echocardiographic anatomy which references the position of the heart within the thorax and its adjacency to surrounding structures6. Multi-detector row computed tomography has allowed the development of a common terminology since it permits unparalleled views of the heart valves and allows their orientation according to both fluoroscopic and echocardiographic views (Figure 1). This imaging technique has therefore become pivotal in the evaluation of TAVI candidates and is fundamental in the planning of newer techniques for transcatheter mitral valve implantation. In patients with aortic stenosis, it provides accurate anatomic characterisation (i.e., bicuspid versus tricuspid anatomy, burden of valve calcification), measurements where the transcatheter valve is to be deployed, and precise evaluation of the spatial relationships of the valve apparatus with surrounding structures7. It also permits accurate device sizing, selection of the appropriate access route and reconstruction of the optimal fluoroscopic projections. Furthermore, 3D transoesophageal echocardiography permits volume rendering and multiplanar reconstruction of the heart valves similar to multi-detector row computed tomography, allowing the use of common terminology between interventionists and imaging cardiologists (Figure 1). Development of software that permits integration (or fusion) of 3D transoesophageal echocardiography and computed tomography data with fluoroscopy has further facilitated this communication, since transcatheter valve procedure can be monitored with excellent soft-tissue resolution of cardiac structures using fluoroscopic orientation (Figure 1)8. These therapeutic and technological advances will demand specialised training in multimodality imaging and interventions for fellows who are interested in forming part of teams dedicated to structural heart disease.
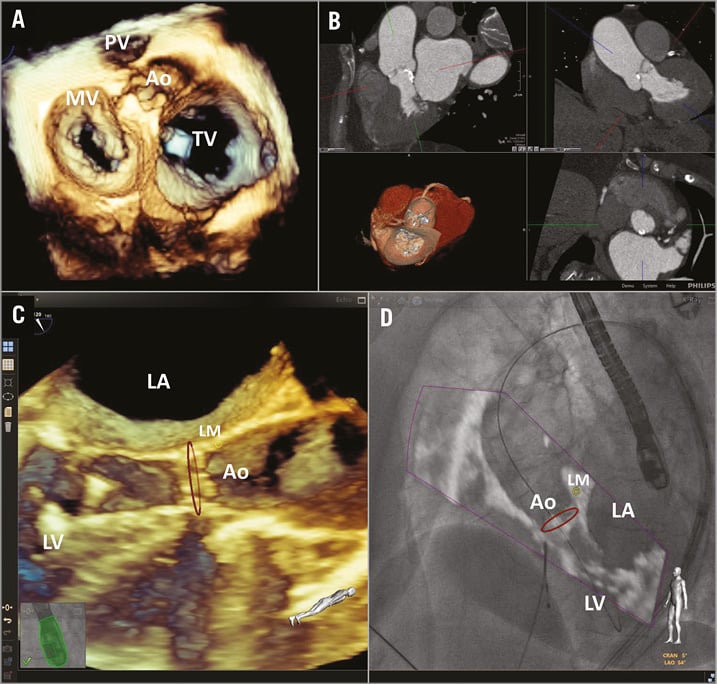
Figure 1. Multimodality imaging in transcatheter interventions for valvular heart disease. Panel A shows the en face view of the four cardiac valves on 3D transoesophageal volume rendering. Panel B shows multi-detector row computed tomography data of the heart with multiplanar reconstructions across the aortic annulus to measure its dimensions and 3D volume rendering with an en face view of the aortic and the mitral valve. Panel C shows a live 3D transoesophageal echocardiographic view of the aortic valve during TAVI which can be overlaid on the fluoroscopic view to guide the procedure (D). Note the red circle indicating the position of the aortic annulus and the yellow circle demarcating the position of the left coronary ostium (courtesy of Dr José Luis Zamorano, University Hospital Ramon y Cajal, Madrid, Spain). Ao: aortic valve; LA: left atrium; LV: left ventricle; MV: mitral valve; PV: pulmonary valve; TV: tricuspid valve
This section of the EuroIntervention PCR London Valves supplement summarises the current role of imaging in transcatheter valve interventions and underscores the use of multimodality imaging and integration of different modalities to optimise the results of intervention and improve clinical outcomes.
Funding
The Department of Cardiology of Leiden University Medical Center has received research grants from Edwards Lifesciences, Biotronik, Boston Scientific and Medtronic.
Conflict of interest statement
V. Delgado has received speaker fees from Abbott Vascular. J. Bax has no conflicts of interest to declare.

