Abstract
Aims: The present study aimed to evaluate the safety and feasibility of a low frame rate protocol for chronic total occlusion (CTO)-percutaneous coronary intervention (PCI).
Methods and results: A total of 192 consecutive patients who underwent CTO-PCI following the low frame rate protocol were analysed. The low frame rate protocol adopted reduced frame rates and the addition of copper and aluminium filters. Procedural outcomes, radiation dose and in-hospital outcomes were ascertained. Meanwhile, a phantom experiment was designed to measure the radiation dose reduction. Overall technical and procedural success rates were 91.1% (175) and 90.6% (174), respectively. The retrograde approach was attempted in 56 (29.2%) lesions. The mean air kerma (AK) radiation exposure, fluoroscopy time and contrast volume were 2.6±2.0 Gy, 50.3±34.3 min and 294.1±131.8 ml, respectively. In-hospital major adverse events occurred in one patient (0.5%) and procedural complications occurred in six patients (3.1%). In the phantom experiment, a remarkable radiation dose reduction could be achieved for AK, dose area product (DAP), simulated first and second operator radiation exposure (reduction of 72.5%, 69.8%, 60.9% and 59.6%, respectively) in cineangiography from this protocol.
Conclusions: Our results provide the primary evidence that it appears to be safe and feasible to carry out the low frame rate protocol for CTO-PCI.
Abbreviations
AK: air kerma
ALARA: as low as reasonably achievable
CABG: coronary artery bypass grafting
CART: controlled antegrade and retrograde tracking
CTO: chronic total occlusions
DAP: dose area product
FPS: frames per second
LAD: left anterior descending artery
LVEF: left ventricular ejection fraction
MI: myocardial infarction
NSTEMI: non-ST-segment elevation myocardial infarction
PCI: percutaneous coronary intervention
PMI: periprocedural myocardial injury
PMMA: polymethyl methacrylate
ST: stent thrombosis
TIMI: Thrombolysis In Myocardial Infarction
Introduction
In recent decades, percutaneous interventional therapy has become one of the cardinal treatment strategies for numerous cardiovascular diseases. Meanwhile, as various reports focusing on radiation risk have been published in journals, safety concerns have gradually been raised1-3. The idiom “a double-edged sword” has been used to describe ionising radiation in the field of medicine.
More than 20% of the patients affected by coronary artery disease have at least one chronic total occlusion (CTO)4,5. As the “last frontier” of percutaneous coronary intervention (PCI)6, CTO-PCI carries a significantly high radiation dose7,8 and more complications9-11 than PCI in non-CTO lesions. Undoubtedly, daily radiation exposure will inevitably impair the health of medical professionals. Therefore, it is very important to reduce radiation exposure in CTO-PCI by adopting the appropriate protocol. Up until now, in accordance with the principle of “as low as reasonably achievable” (ALARA)12, many attempts have been made to reduce radiation exposure13-16 for diagnostic coronary angiography and non-CTO-PCI procedures. So far, however, radiation protocol optimisation for CTO-PCI has rarely been reported.
To achieve a good balance of imaging quality and radiation dose reduction, we adopted a low frame rate protocol for CTO-PCI using the Philips X-ray system. This new protocol involved reduced default frame rates (15 to 7.5 frames per second [FPS]) and the addition of copper (Cu) and aluminium (Al) filters. Procedural outcomes, radiation dose parameters, and in-hospital outcomes were retrospectively evaluated.
Meanwhile, in view of the lack of operators’ radiation exposure in the present study and confounding factors in the real world (patient characteristics and X-ray system manipulation), a phantom experiment was designed to determine the radiation dose reduction from this protocol under standardised radiology conditions. Therefore, this study sought to evaluate the safety and feasibility of a low frame rate protocol for CTO-PCI and how much radiation dose reduction could be achieved from this protocol under standard conditions.
Methods
STUDY POPULATION
Between June 2015 and February 2017, 192 consecutive patients who underwent CTO-PCI adopting the low frame rate protocol were retrospectively screened and analysed from the database of the Chronic Total Occlusion Club, China. All the CTO cases from authorised CTO club experts were consecutively recorded in the dedicated database. Each CTO-PCI was performed according to the current guidelines and algorithms. A total of six first operators participated in the completion of all of the above procedures. The study protocol was approved by the hospital’s medical ethics committee. All patients provided written informed consent before participating in the procedure.
IMAGING PROTOCOL
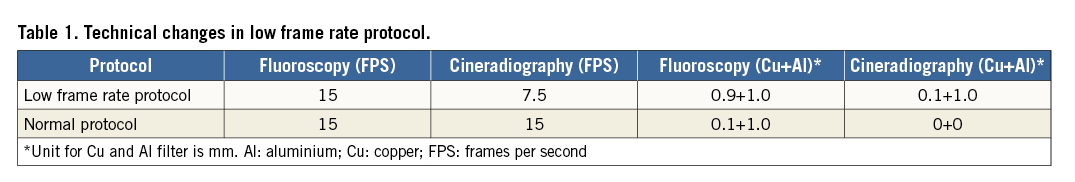
All procedures under the low frame rate protocol were carried out in two identical cardiac catheterisation laboratories (Philips Allura Xper; Royal Philips Electronics, Amsterdam, the Netherlands) in our intervention centre. The radiation parameters set for the two systems were consistent and synchronised. The technical changes in the low frame rate protocol (Table 1) included: 1) an extra 0.9 mm Cu filter for fluoroscopy mode; and 2) reduced FPS (15 to 7.5) and an extra 0.1 mm/1.0 mm Cu/Al filter for cineangiography mode. The air kerma (AK) radiation exposure was registered as indicated by the X-ray system.
DEFINITIONS AND STUDY ENDPOINTS
CTO was defined as Thrombolysis In Myocardial Infarction (TIMI) grade 0 flow and duration of coronary occlusion ≥3 months6. The angiographic indices examined were the locations of the CTO, stump morphology, calcification at the site of the occlusion (radiopacity present before contrast injection), vessel tortuosity (the presence of at least one bend of >45° proximal to the occlusion)17 and grades of collaterals18. The J-CTO score was calculated according to the previous study reported by Yoshihiro17. All of the films were reviewed by at least two qualified interventional doctors. If there was any ambiguity in the reports or films, the films were reviewed independently by a third well-qualified interventional doctor.
Technical success was defined as a restoration of TIMI flow grade 3 in the target vessel and a residual stenosis <30% by visual estimation. Procedural success was defined as achievement of technical success without in-hospital major adverse cardiac events (MACE).
In-hospital outcome evaluation included in-hospital MACE, periprocedural myocardial injury (PMI) and procedural complications. In-hospital MACE included any of the following adverse events before hospital discharge: death from all causes; stent thrombosis (ST)/Q-wave myocardial infarction (MI); ischaemia-driven revascularisation; emergency cardiac surgery. The Academic Research Consortium definition19 was used to define ST. PMI was defined according to the third universal definition of MI20. Donor vessel dissection, vessel perforation and cardiac tamponade were assessed as procedural complications. Coronary perforation was defined as any contrast pool or evidence of contrast leak into cardiac chambers or pericardial space21. Perforations were divided into two categories according to the location of perforation: 1) target vessel perforation; and 2) collateral perforation.
PHANTOM EXPERIMENT
A 20 cm polymethyl methacrylate (PMMA) phantom was adopted to simulate the adult human body layer thickness in the standardised radiology experiment (Figure 1). The centre of the PMMA phantom was placed at a height of 110 cm. Real-time radiation dosimeters were placed at the simulated positions of the first and second operators. To simulate the operator’s position in the radial access, the real-time radiation dosimeter was taped to a drip stand at a height of 140 cm22 (approximately at the level of the left chest) and was positioned at a lateral distance of 45 cm from the centre of the phantom. The distance between the operator and the exposed centre of the phantom was 95 cm in the posterior-anterior projection for radial access. The second operator was located 60 cm from the first operator. The system-attached conventional lead curtains were placed beside the first operator.
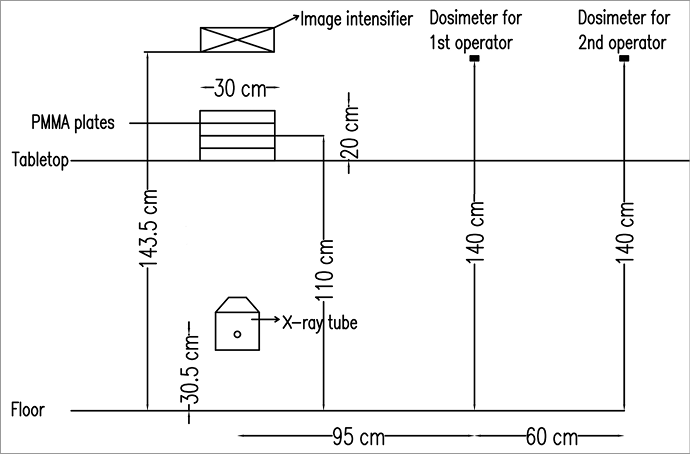
Figure 1. Experimental arrangements to measure radiation dose using a polymethyl methacrylate (PMMA) phantom. The position arrangements were set to simulate the operator’s position in radial access. The centre of the PMMA phantom was placed at a height of 110 cm. The real-time radiation dosimeter was taped to a drip stand at a height of 140 cm and a lateral distance of 45 cm from the centre of the phantom. The distance between the operator and the exposed centre of the phantom was 95 cm in the posterior-anterior projection. The second operator was located 60 cm from the first operator.
Exposures were carried out ten times in each of nine routine projections, including right anterior oblique (RAO) 30°, RAO 30°+cranial (CRA) 30°, RAO 30°+caudal (CAU) 30°, left anterior oblique (LAO) 45°+CAU 30°, LAO 45°+CRA 30°, CRA 30°, CAU 30°, LAO 45° and LAO 20°+CRA 20°. Each exposure time was controlled at between three to six seconds in the cineangiography mode. Then, AK and dose area product (DAP) values were registered as indicated by the X-ray system. The real-time radiation dose for simulated operators was measured using the RaySafe X2 dosimeter (Unfors RaySafe, Billdal, Sweden). The series data were compared between the two protocols in the cineangiography mode (Table 1).
STATISTICAL ANALYSIS
Data were expressed as the mean±SD for continuous variables, and as frequencies for categorical variables. Comparison of continuous variables was performed using the independent Student’s t-test or the Mann-Whitney U test as appropriate. Statistical analysis of the categorical variables was performed using the Pearson chi-square or Fisher’s exact test as appropriate. P-values were two-tailed, and p<0.05 was considered statistically significant. The data were analysed with SPSS, Version 20.0 (IBM Corp., Armonk, NY, USA).
Results
BASELINE CHARACTERISTICS
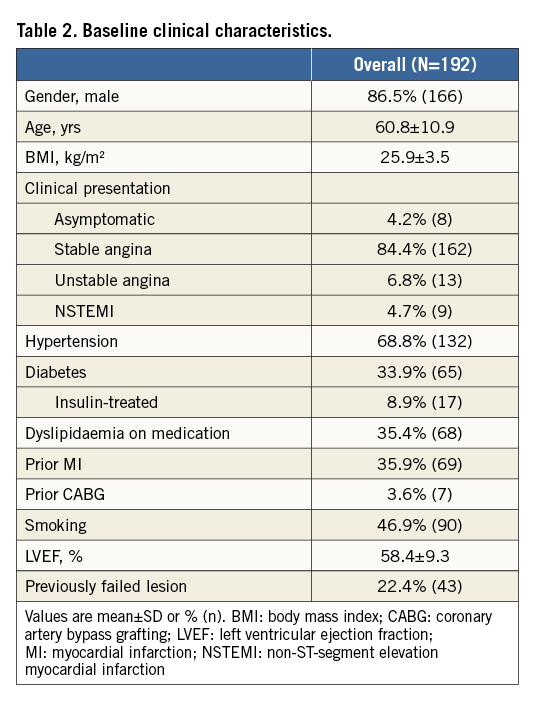
The baseline clinical characteristics of the patients are presented in Table 2. As is common in CTO-PCI series, males (86.5%) were the dominant group in the overall patient population. The prevalence of hypertension, diabetes, dyslipidaemia on medication, prior MI, prior coronary artery bypass grafting (CABG) and smoking was 68.8%, 33.9%, 35.4%, 35.9%, 3.6% and 46.9%, respectively. Previously failed lesions accounted for 22.4% of all lesions.
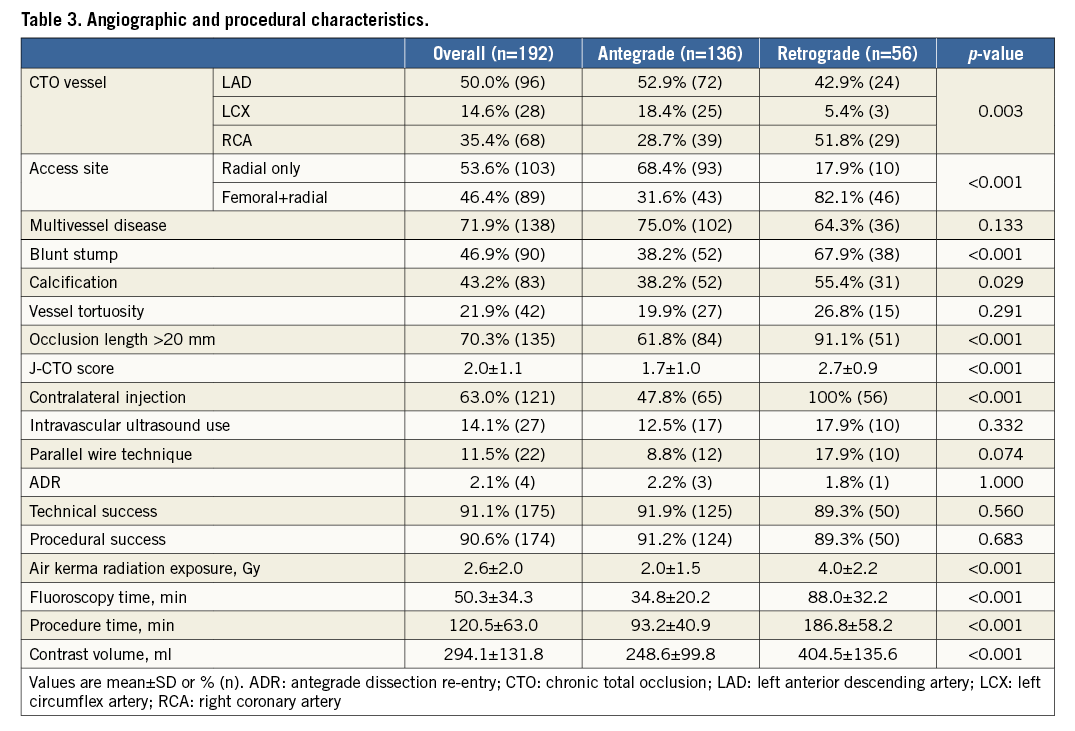
ANGIOGRAPHIC AND PROCEDURAL CHARACTERISTICS
Table 3 summarises the angiographic and procedural characteristics of all procedures. The overall average J-CTO score was 2.0±1.1. The overall technical and procedural success rates were 91.1% (n=175) and 90.6% (n=174), respectively. The average AK radiation exposure, fluoroscopy time and contrast volume was 2.6±2.0 Gy, 50.3±34.3 min, and 294.1±131.8 ml, respectively.
The retrograde approach was attempted in 56 (29.2%) lesions. Most CTO angiographic characteristics, which were acknowledged to be associated with procedural difficulties, showed significant differences between the antegrade and retrograde approach groups. Moreover, there were significant differences of AK radiation exposure, fluoroscopy time and contrast volume (p<0.001) among the radiation dose parameters between the two groups.
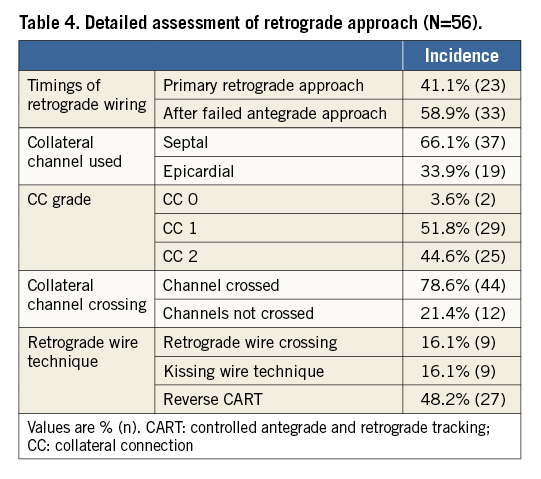
ASSESSMENT OF RETROGRADE APPROACH
Details of the retrograde approach are shown in Table 4. A primary retrograde approach was employed in 41.1% of retrograde cases with a retrograde method after failed antegrade approach in the remaining. Retrograde wire crossing of collateral channels was achieved in 78.6% of retrograde cases. Among the cases with retrograde approach, there were 16.1%, 16.1% and 48.2% cases where we used the retrograde wire crossing technique, kissing wire technique and the reverse controlled antegrade and retrograde tracking (CART) technique, respectively.
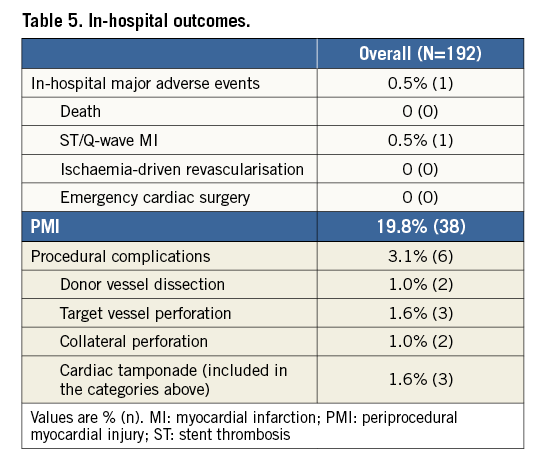
IN-HOSPITAL OUTCOMES
Detailed in-hospital outcomes are presented in Table 5. A major adverse event occurred in one patient (0.5%) with instances of Q-wave MI. This Q-wave MI was associated with the occlusion of the 2nd diagonal branch in a left anterior descending artery (LAD)-CTO antegrade approach and was treated conservatively. PMI was observed in 38 (19.8%) cases. The incidence of donor vessel dissection, target vessel perforation, collateral perforation and cardiac tamponade was 1.0%, 1.6%, 1.0% and 1.6%, respectively. Donor vessel dissection occurred in two cases, with one type E and one type F dissection. Both dissections were treated by stent implantation. Four cases experienced vessel perforation, of which two were target vessel perforation (one Ellis type I and one Ellis type III), one was epicardial collateral perforation (Ellis type III) and one case experienced both (Ellis type III for target vessel perforation and Ellis type II for epicardial collateral perforation). By treatment with a membrane-covered stent or coil, all the patients mentioned above were discharged after an uneventful course.
PHANTOM EXPERIMENT
With adoption of the low frame rate protocol, a remarkable radiation dose reduction could be achieved for pooled AK, DAP and simulated operator radiation exposure in the cineangiography mode (Figure 2). The new protocol achieved a 72.5% reduction of AK value (4.6±1.3 vs. 16.7±3.5 mGy/s, p<0.001) and a 69.8% reduction of DAP value (292.9±71.3 vs. 970.6±188.1 mGy·cm2/s, p<0.001). The reduction for simulated operators was 60.9% for the first operator (314.9±162.9 vs. 805.5±419.8 nSv/s, p<0.001) and 59.6% for the second operator (151.8±72.5 vs. 376.1±182.4 nSv/s, p<0.001). The reduction was very significant for every projection position.
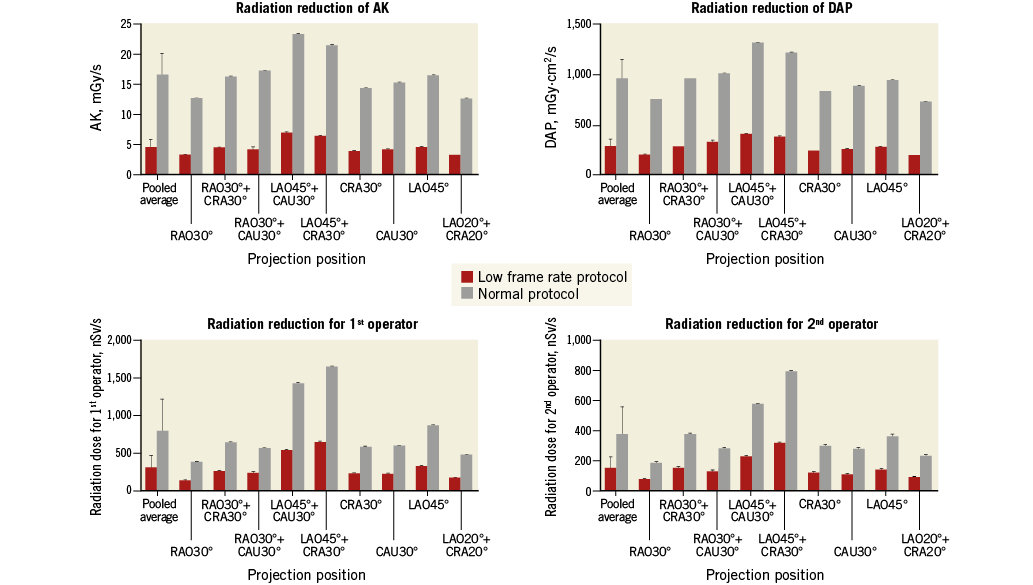
Figure 2. Radiation dose comparisons between the low frame rate protocol and normal protocol in the cineangiography mode of the phantom experiment. Reduction was very significant for air kerma (AK), dose area product (DAP), simulated first and second operator radiation exposure in cineangiography using the low frame rate protocol.
Discussion
CTO-PCI inevitably involves the problems of a daily accumulation of high radiation exposure. Therefore, it is very important to reduce radiation dose in CTO-PCI by adopting an appropriate protocol. However, deterioration of the image quality, as a reasonable consequence of radiation reduction, could have a potential impact on the quality of the procedure. Therefore, the key question is how to strike a good balance between a reduction of radiation dose and the quality of the procedure.
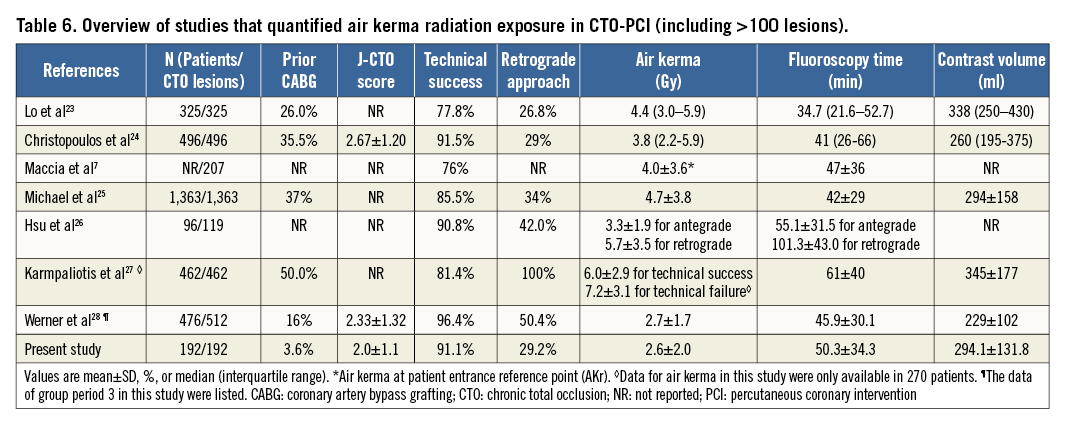
From our results, no death, no ischaemia-driven revascularisation and no emergency cardiac surgery was observed. Q-wave MI occurred in only one case because of the occlusion of the 2nd diagonal branch in a LAD-CTO antegrade approach. Compared with the normal frame protocol, the image obtained using the low frame rate protocol in this study was compromised a little. To overcome this limitation, the operators always performed tip injection to select the most promising interventional collateral channels for retrograde approach. With tip injection, most of the tiny collateral channels could be visualised clearly. In terms of procedure-related complications, vessel perforation contributed most to the total complications. After proper monitoring and treatment, there were no subsequent adverse events. However, the complications under the new radiation protocol should be carefully evaluated in larger studies. From the perspective of effectiveness, we scrutinised larger studies7,23-28 that quantified AK value in CTO-PCI (Table 6). Among these studies, the present study showed an excellent combination of high technical success rate and low radiation exposure from the low frame rate protocol. The levels of fluoroscopy time and contrast volume were also comparable. Nevertheless, we should also be aware of the different baseline characteristics among these studies, such as prior CABG. In this study, prior CABG was found in 3.6% of the patients, less than in western countries24. Obviously, a higher proportion of prior CABG was related to more calcification24, higher J-CTO score and lower success rates, hence the increased radiation exposure. Additionally, it should be pointed out that higher radiation dose was related to higher body mass index (BMI).
In order to make up for the lack of operators’ radiation dose, we designed a standardised phantom experiment to simulate the operators’ locations and assessed how much radiation dose reduction could be achieved from this protocol. Naturally, differences exist between the standard radiology experiment and real-world manipulation, but it can provide the basic test data for further attempts and studies. Also, in the real world, radiation dose is affected by many factors, such as the heterogeneity of patient characteristics (age, BMI, gender, etc.) and X-ray system manipulation (distance from radiation source to patient, height of intensifier, etc.). In these respects, a standardised test has its own advantages. The results showed a remarkable reduction (about 60%) using this new protocol. This could represent a very significant improvement for the world’s busy intervention centres, especially the high-volume CTO intervention centres.
Limitations
This study had several limitations. First, this study had a retrospective design and included a relatively small number of patients. However, it was innovative and one of the leading studies in this field. During the period of this study, only two X-ray systems were adjusted for the low frame rate protocol in our centre. We should acknowledge that selection bias due to the nature of the study design was present. Second, due to the lack of documentation of radiation dose, historical comparison with similar patients treated in the era before the dose reduction protocol could not be performed. Third, the single institution and single group design of this study mandates further multicentre validation of the results.
Conclusions
Our results provide the first evidence that it appears to be safe and feasible to carry out a low frame rate protocol for CTO-PCI.
| Impact on daily practice By striking a good balance between imaging quality and reduction of radiation dose in the low frame rate protocol, there would be a great degree of radiation dose reduction for CTO-PCI staff and experts. |
Funding
This work was supported by Shanghai Sailing Program (No. 16YF1401600).
Conflict of interest statement
The authors have no conflicts of interest to declare.