The technical advances in percutaneous coronary intervention (PCI) of chronic total occlusions (CTO) are well documented: in randomised trials the success rate has been reported as 87%1,2, and in expert centres above 90%. One aspect of CTO PCI is often neglected in daily practice as it does not carry immediately obvious risks for the patient, namely the radiation exposure during often lengthy procedures. In a meta-analysis of complications related to CTO PCI, radiation risk is mentioned but the incidence was almost zero3. This is too low, because none of the studies reviewed looked for actual damage. Radiation damage to the skin typically appears a few days after discharge on the back of the patient. Even then, it is seldom realised without specific instructions for follow-up examinations. There are a few studies which have explicitly looked for skin injury, revealing a higher incidence when re-examining the patient carefully after the procedure4. Damage to the skin may occur with a skin entry dose as low as 2 Gy and invariably after 5 Gy, leading to different degrees of skin alteration5 (Figure 1).
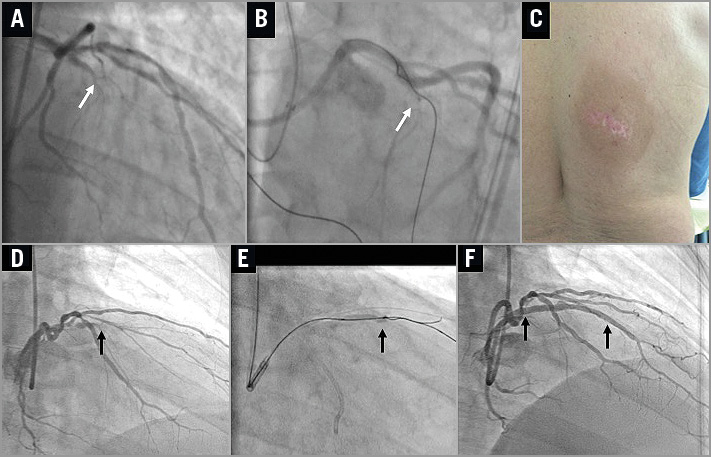
Figure 1. Example of excessive radiation exposure and skin damage, and minimised radiation exposure in the same patient. A 53-year-old patient underwent PCI for a proximal left anterior descending artery (LAD) CTO (panel A, arrow). In this procedure the operator attempted a retrograde recanalisation via a conus branch from the right coronary artery, which ultimately failed as he could not pass the retrograde wire through the lesion (panel B, arrow). The procedure was documented on 125 cine runs at a rate of 25 cineframes/s in predominantly anteroposterior cranial projection. The estimated radiation dose must have exceeded 15 Gy. C) The patient’s back three months later showed a rectangular patch of discoloured skin with a central ulcerated part. D) A reattempt of the lesion (arrow) was performed in the author’s institution, avoiding the damaged skin area in RAO cranial and plain RAO projections. E) It was a complex retrograde reverse CART procedure (arrow) using an epicardial collateral from the first diagonal to the LAD. F) The procedure was successful with placement of two drug-eluting stents (arrows). The fluoroscopy time was 85 min, with only 2.215 Gy using a low-dose radiation protocol9.
Raising awareness of radiation damage together with a discipline of radiation-saving protocols in the cath lab is important and overdue. Not only has the recanalisation technique evolved, but also X-ray equipment has been further refined with a specific focus on radiation safety. However, minimising radiation requires the active interaction of the operator with the machine. The paper by Ge et al in this issue of EuroIntervention6 contributes to the still scarce literature on radiation exposure and active radiation reduction in CTO PCI.
This is for the benefit of the patient, and also for the sake of the operator and the cath lab staff7. The authors report on a modified low-dose protocol based on modified filters and a reduced frame rate for cineangiography. They observed no loss of procedural success or safety during their procedures. They do not compare this to a previous time period but put it into perspective with recently published data from other CTO registries. They also present an experimental model in which they showed the positive impact of this protocol on radiation dose. They varied projection angles and recorded operator exposure and compared this to a standard protocol without filters and higher cine frame rates.
The observed reduction in radiation dose could have been even higher, if the operators had modified the fluoroscopy rate as well. It should be noted that of course radiation during cineangiography is the main contributor to the total radiation exposure but, given the trend to use fluoroscopy storage wherever feasible and reduce cineangiography to a minimum, the contribution of fluoroscopy frame rates becomes more relevant. A randomised study on the radiation saving effect of a fluoroscopy rate of 7.5 versus standard rates of 15/s showed a significant radiation reduction. Again that study did not use the whole potential of radiation reduction as they used cineangiographic frame rates of 15/s8. The human eye can hardly discriminate between a 15 or 7.5/s frame rate and, if the equipment allows the modification, we can even work comfortably with 6 pulses/s for fluoroscopy, with no negative impact on the success rate9. We may increase the cineangiographic rate to 15/s for detailed assessment of the collateral circulation, but then should actively reduce it again and prefer fluoro over cine documentation.
Ge et al compare their study results with a few published registry observations, but what is missing as one of the major determinants of radiation exposure is the body weight or body mass index (BMI). This value is required to compare studies in different populations. In the USA, and also in Europe, the weight and BMI are considerably higher. In the present study the BMI was 25.9, in our study it was 28.8 at 88 kg9, and in the recent OPEN-CTO registry from the USA the air kerma (AK) of 2.5 Gy was as low as in Ge’s study, but at a BMI of 30.510.
These comparisons underscore the potential of further optimising the radiation reduction measures in our cath labs beyond that which was demonstrated in the current study. The management of radiation must be an integral part of a CTO procedure and the general ALARA (as low as reasonably achievable) rule of radiography needs to be followed. While in the USA an excess of radiation may even carry legal consequences, this is not the case in most other countries. However, it is the operator’s responsibility to minimise damage to the patient and to do what is possible with the highly developed X-ray systems we have available.
Conflict of interest statement
The author has no conflicts of interest to declare.