Abstract
In the majority of hypertensive patients, no particular cause for abnormal blood pressure is evident (primary or essential hypertension). In contrast, in the minority of patients with secondary hypertension a specific underlying cause is responsible for the elevated blood pressure. The prevalence of secondary hypertension is higher in patients with resistant hypertension than in the general hypertensive population and increases with age. The list of secondary forms of hypertension is long and prevalence of the individual causes of secondary hypertension varies. Hence, this review divides them into two categories: common causes and rare causes. If appropriately diagnosed and treated, patients with a secondary form of hypertension might be cured, or at least show an improvement in their blood pressure control. Consequently, screening for secondary causes of hypertension plays an essential part in the care of patients with arterial hypertension. If the basal work-up raises the suspicion of a secondary cause of hypertension, specific diagnostic procedures become necessary, some of which can be performed by primary care physicians, while others require specialist input.
Common causes
RENAL VASCULAR DISEASE
Atherosclerosis and fibromuscular dysplasia (FMD) are the two main causes of renal artery stenosis. The gold standard for diagnosing renal vascular disease is renal angiography. Due to the invasive nature of renal angiography, other alternative non-invasive methods for initial screening/evaluation are preferable, namely renal artery Doppler ultrasonography, computed tomography scan, or magnetic resonance angiography of the renal arteries1-3.
Haemodynamically relevant atherosclerotic renal artery stenosis (ARAS) (>70% diameter narrowing) is found in nearly 10% of patients with resistant hypertension over 65 years of age4. The presence of relevant ARAS should be considered particularly in patients with rapidly deteriorating renal function, those with a reduction in their estimated glomerular filtration rate of >25% after administration of a renin-angiotensin system-inhibitor or angiotensin receptor blocker, onset of hypertension after 50 years of age, and those with a history of “flash pulmonary oedema”. In autopsy studies, ARAS prevalence ranges from 4%-50%1,2,5, indicating that a significant number were apparently both not suspected and associated with hypertension during life. Moreover, in the ASTRAL (Angiopathy and Stenting in Renal Artery Lesions) trial, stenting of obstructed renal arteries did not overall result in a meaningful clinical benefit in terms of blood pressure (BP) control6. However, methodology problems with this study have been raised, among which the most significant is selection bias. Patients were enrolled if they had ARAS that was considered potentially suitable for stenting, and if the physicians were uncertain that the patient would definitely have a worthwhile clinical benefit from intervention. About 40% of the enrolled patients had <70% diameter narrowing7-9. Perhaps the recently completed Cardiovascular Outcomes in Renal Atherosclerotic Lesions (CORAL) study will help to clarify the doubts and the potential benefits of percutaneous transluminal renal angioplasty with stenting in subjects with ARAS.
FMD is a much less frequent cause (10%) and is more frequently encountered in younger females10,11, but should also be considered in older subjects and in male patients12. In contrast to ARAS, the interventional therapy (i.e., percutaneous dilation) in FMD is much more often successful. In a retrospective analysis, about half of the patients with FMD who underwent intervention were completely cured from their hypertension, with others having at least some beneficial effect on BP, serum creatinine and the number of antihypertensive drugs required for BP control13.
RENAL PARENCHYMAL DISEASE
Chronic kidney disease (CKD) is frequently associated with hypertension, but in this case the kidney can be both “the victim and the culprit”, meaning that CKD not only causes hypertension but can also be a complication of hypertension. The prevalence of hypertension is related to the severity of renal function impairment14. All recent guidelines recommend lower BP goals in patients with CKD, especially in those subjects with albuminuria15,16. However, fewer than 15% of patients with CKD achieve the BP target value of <130/80 mmHg despite taking a combination of three or more medications4,17,18. In patients with CKD the degree of albuminuria predicts both the prognosis in respect of kidney function and also cardiovascular morbidity and mortality19-22. Results from a long-term follow-up study revealed that the probability of normalisation of urinary albumin excretion during antihypertensive treatment is clearly reduced when glomerular filtration rate (GFR) is below 60 ml/min/1.73 m2.23
Initial evaluation of suspected renal parenchymal disease includes blood tests (serum creatinine (or cystatin C) for estimation of GFR), urine tests (including presence of protein, erythrocytes and leukocytes) and renal ultrasonography24.
PRIMARY ALDOSTERONISM
The prevalence of primary aldosteronism (PA) is greater than previously thought. In contrast to the still widely held belief, absence of hypokalaemia or absence of an adrenal mass cannot rule out the presence of hyperaldosteronism25,26. It is thought that hypokalaemia is only present in severe and/or late manifestations of PA. Among untreated patients, the prevalence of PA increases in parallel with the increasing severity of the hypertension, from 2% in patients with stage 1 hypertension to 8% in those with stage 2 hypertension and 13% in those with stage 3 hypertension25,27-31. Moreover, in resistant hypertensives, the prevalence of PA ranges between 15 and 23%28,32.
Previous investigations revealed that hyperplasia of the glands is more frequent than adrenal adenomas10,33. If an adenoma exists, comprised of cortical glomerulosa cells, it is usually unilateral. PA is rarely caused by adrenal carcinoma.
The aldosterone-renin ratio (ARR) is the most reliable test for screening purposes. However, like all biochemical tests, false-positive and false-negative results may occur. Ideally, hypokalaemia should be corrected if present (because hypokalaemia inhibits aldosterone release, which can lead to a false-negative screening test). Moreover, it was often postulated that interfering medication should be removed; however, for safety reasons this cannot always be done in every patient with severe hypertension. The impact of concomitant medication is small when using α-blockers and ACE-inhibitors34. Amlodipine gave a very small percentage of false-negative diagnoses for PA35. Beta-blockers can be responsible for an increased rate of false-positive ARR as they potently suppress renin release34. However, treatment with an aldosterone antagonist (e.g., spirolactone) and/or a direct renin inhibitor (aliskiren) has to be stopped in any case.
It has been suggested that ARR is most sensitive when collected in the morning (at least two hours after the patient gets up) at rest in a seated position. There are important and confounding differences across laboratories regarding the methods and units used to report values of renin and aldosterone. Therefore, the reported threshold ranges from 20-100, with the most commonly adopted threshold of 30 (for aldosterone in ng/dl over plasma renin activity in ng/ml/h)36.
If the ARR is positive, biochemical evidence of PA has to be confirmed, e.g., with the oral sodium loading36. If biochemical evidence for hyperaldosteronism can be confirmed, then the next step is imaging of the adrenal glands, i.e., by computed tomography. Finally, lateralisation of the source of excessive aldosterone secretion, demonstrated by adrenal vein sampling (AVS), is critical to guide the management of PA, i.e., to aid in making the decision whether surgery or medical treatment should be pursued36-38. However, selective bilateral catheterisation is technically challenging. Retrospective data from the German Conn’s Registry revealed a bilateral success rate of AVS of only about 30% by using a selectivity index (cortisol adrenal vein/cortisol inferior vena cava) of ≥2.0. After implementation of standard operating procedures, mean success rate increased to 61%, with individual success rates of >70% in selected centres which additionally performed a rapid cortisol assay39.
OBSTRUCTIVE SLEEP APNOEA
Even in the general population, and particularly in men, obstructive sleep apnoea (OSA) is a common finding40. In addition, it has been shown that OSA in normotensive subjects predicts future development of hypertension10. Approximately 30% of adults with hypertension have OSA41-43. OSA is a strong and independent risk factor for the presence of hypertension and cardiovascular diseases41-43. OSA is often associated with isolated diastolic hypertension44-46. Moreover, masked hypertension must also be considered in patients with OSA and hence 24-hour ambulatory blood pressure monitoring (ABPM) should be done47.
OSA is characterised by repetitive episodes of complete or partial upper airway obstruction and respiratory effort-related arousal events during sleep. The daytime symptoms of OSA can comprise severe hypersomnia and lack of energy.
Specific questionnaires48,49 may be helpful in the routine assessment of the clinical features of OSA, but their diagnostic sensitivity and specificity are low50. Standard methods for examination of OSA are polygraphy and polysomnography; the latter simultaneously also includes recording of sleep. Both diagnosis of OSA based on the International Classification of Sleep Disorders (ICSD) criteria and management of patients with OSA and hypertension are reviewed in detail in the joint recommendations by the European Society of Hypertension, by the European Respiratory Society and by members of European COST ACTION B26 on OSA51. Meta-analyses of clinical trials on the effect of continuous positive airway pressure (nCPAP) on BP are available. Bazzano et al included 16 randomised clinical trials published between 1980 and 2006 in their meta-analysis. A total of more than 800 participants were included and the study compared CPAP to control. The reported BP mean net change in SBP for those treated with CPAP when compared with control was nearly –2.5 mmHg; the mean net change in DBP was nearly –2 mmHg during the intervention52. Nevertheless, although the BP reduction may be modest in some patients, screening and diagnosing of OSA should be taken into account, since it was also shown that “the higher the BP and/or more severe OSA, the larger the reduction”52,53. Furthermore, presence of OSA is an independent and additional risk factor of cardiovascular diseases51.
DRUG-INDUCED HYPERTENSION
Drug-induced hypertension is one of the most common causes of secondary hypertension and is often found in clinical practice. Many prescriptions and over-the-counter medicines can exacerbate arterial hypertension. The elimination of the responsible agent is not always possible in some cases, but a dose reduction or an alternative treatment option should be considered54.
The use of non-steroidal anti-inflammatory drugs (NSAIDs) for example is often the cause of drug-induced hypertension54,55. In 265 patients with drug-related hypertension, NSAIDs as a contributing factor to poor BP control could be identified in 88% of cases10. Data on the precise effects of NSAIDs on BP levels are not available, and hence two important aspects should be taken into account. First are the potential differences of the effect on BP among the various NSAIDs. For example, a meta-analysis has shown that naproxen and indomethacin were associated with the largest BP elevations, while piroxicam, sulindac, ibuprofen, and aspirin exhibited little, if any, effect on BP56. Second are the potential differences of NSAIDs on BP according to concomitant antihypertensive medication used57,58.
As another group, mineralocorticoids and oral glucocorticoids are able to increase SBP as much as 15 mmHg within 24 hours59. Another important group of medications are oral contraceptives. They represent a class of drugs that are widely used and are capable of inducing hypertension60. Oral contraceptives result in a mild elevation of BP in most women and lead to hypertension in about 5%. The Nurses’ Health Study comprising more than 60,000 normotensive women found that women using oral contraceptives had an 80% higher risk of developing hypertension compared to women who were not using such drugs61. Of note, combined oral contraceptives (progestin and oestradiol) are more frequently associated with BP elevations than progestin-only oral contraceptives10,62,63. Oestradiol treatment effects on SBP in healthy postmenopausal women64 differ significantly depending on age, suggesting an increase in SBP in younger postmenopausal women, while having the opposite effect in older postmenopausal women.
Another class of agents which has a profound influence on the development of hypertension are antineoplastic drugs, such as VEGF-inhibitors. Development of hypertension was found in 20-30% of patients treated with bevacizumab, and 15-60% of patients treated with VEGF kinase inhibitors65.
Other important groups of drugs that can cause an increase in BP are, for example, the sympathomimetics (diet pills, amphetamines), the antidepressants and erythropoietin agents4.
Rare causes
There are a number of rare causes of secondary hypertension, which cannot be discussed in detail in this article. Hence, from a clinical point of view specific underlying diseases, which should be ruled out in patients with treatment-resistant hypertension, are reported.
PHEOCHROMOCYTOMA
Although the prevalence of pheochromocytoma in the general hypertensive population is very low, diagnosis and treatment are extremely important in view of the possibility of precipitating hypertensive crisis if the tumour is stimulated66-68. However, only 50% of the patients have recurrent episodes of hypertensive crisis. The clinical presentation of pheochromocytoma can be variable, but a triad of headache, palpitations, and sweating would be typical findings69. Hence, all patients with suggestive clinical symptoms, with incidentalomas or a genetic predisposition (e.g., von Hippel Lindau disease) should be screened70. Once the suspicion is raised, the diagnosis of pheochromocytoma is straightforward. As a screening test to rule out phechromocytoma, 24-hour urinary collection of fractioned metanephrines is recommended. The most sensitive test, but with a higher number of false-positive findings, is to measure plasma levels of free metanephrines, which have a diagnostic sensitivity of 97-99% and a specificity of about 89%69,71. After biochemical evidence for the presence of pheochromocytoma has been ascertained, pre-surgical localisation of the tumour mass includes CT and MRI methods, as well as 123I-labelled metaiodobenzylguanidine (MIBG) scintigraphy72.
CUSHING’S SYNDROME
Due to the prescription of glucocorticoids in a number of clinical conditions, Cushing’s syndrome is in most cases iatrogenic. However, less than half of these patients have hypertension73. In contrast, hypertension is one of the most distinguishing features of endogenous Cushing’s syndrome, and can be found in about 80% of adult patients. The classic physical findings of Cushing´s syndrome are referred to in Table 1. Unfortunately, manifestation varies and many other presented symptoms are non-specific (e.g., menstrual irregularities and glucose intolerance). Hence, Cushing’s syndrome should also be considered in patients with treatment-resistant hypertension and in patients with adrenal incidentaloma. Adrenal adenoma and carcinoma are thought to cause an equal number of Cushings’s syndrome (together about 2-5 cases per million subjects per year). However, there are also reports of an increased number of Cushing’s syndrome due to adrenal adenoma in some regions of the world74,75.
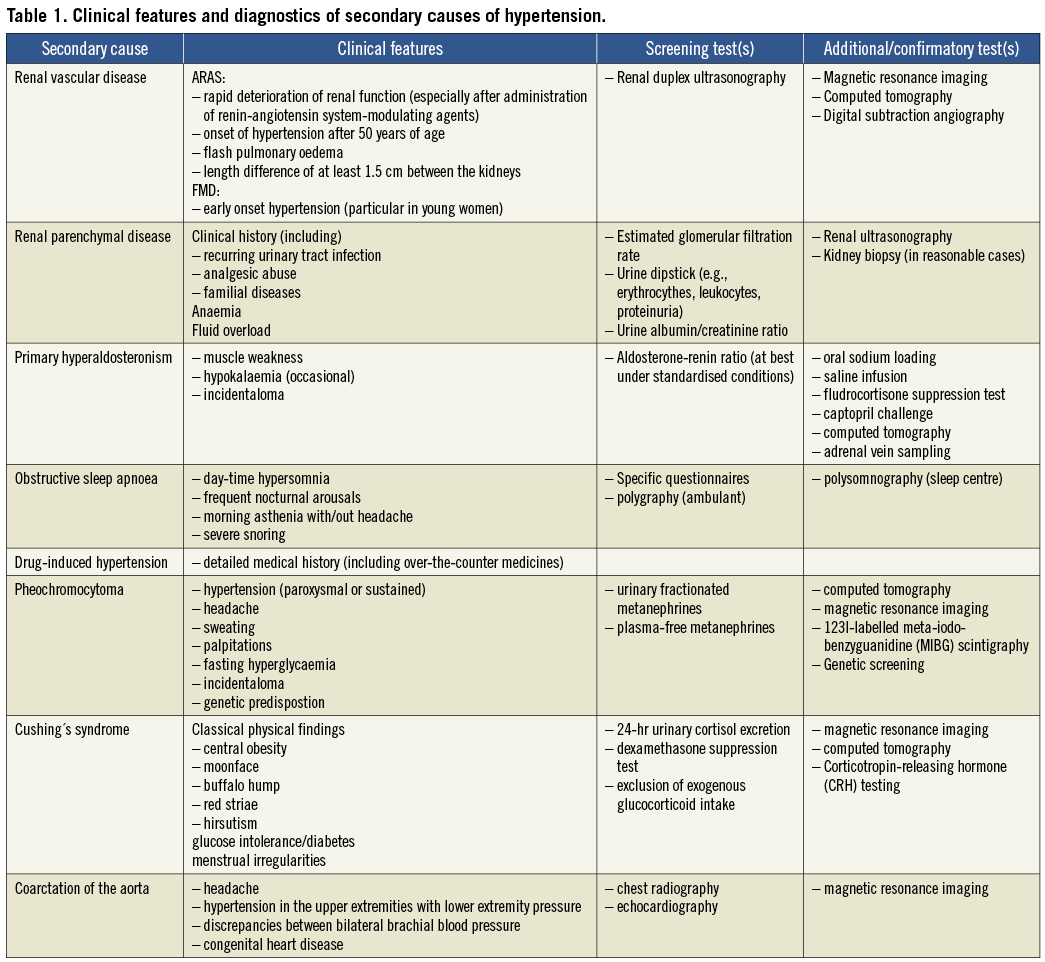
COARCTATION OF THE AORTA
Although coarctation of the aorta is a common cause of secondary hypertension in children, milder cases may first be detected as a rare cause of arterial hypertension in adults. Moreover, it was reported that, despite successful repair of coarctation, elevation in the average systolic 24-hour ABPM and exercise-induced hypertension could persist76. According to American guidelines (JNC VII and ACC/AHA 2008) hypertensive adults with congenital heart disease should be screened for possible coarctation of the aorta16,77. This includes measurement of bilateral brachial (upper extremities) BP, based on the finding that the origin of the left subclavian artery may be distal to the coarctation, and femoral (lower extremities) BP to search for discrepancies. Chest radiography in adults may show the classic “three” sign or rib notching. However, magnetic resonance imaging is the preferred imaging method in adults78.
Conflict of interest statement
The authors have no conflicts of interest to declare.