Sympathetic hyperactivity contributes significantly to the development of ventricular arrhythmias (VA)1. Catheter-based renal sympathetic denervation (RSD) has been demonstrated to reduce norepinephrine spillover and efferent muscle sympathetic nerve activity2. We report a case of a patient with electrical storm, contraindication of cardiac ablation and multiple renal arteries in whom RSD was carried out as an attempt to reduce episodes of ventricular tachycardia (VT).
A 62-year-old man with dilated cardiomyopathy presented with syncope and multiple VA episodes. Implantable cardioverter-defibrillator records showed 50 episodes of VT (cycle length varying from 345 to 430 ms), resulting in 85 ATPs and eight shocks within 48 hours. No reversible causes were found. Despite the use of amiodarone (900 mg/d), magnesium, lidocaine and beta-blocker, VT persisted. An echocardiogram showed the presence of a left ventricular thrombus contraindicating cardiac ablation. Thus, RSD was offered as an alternative therapy.
The angiogram revealed the presence of two main renal arteries as well as two right and one left accessory renal artery (Figure 1A). Five lesions were applied to each main renal artery and one right accessory artery. The remaining arteries were not ablated due to the small diameter. An open-irrigated tip catheter (Therapy™ Cool-Path™; St. Jude Medical, St. Paul, MN, USA) was used for ablation. Satisfactory impedance drop was observed during each ablation point, meaning appropriate tissue heating. The procedure was approved by the local ethics committee and the patient signed informed consent.
No procedural-related complications occurred. Within the first week after ablation there were 10 VT episodes and no ATP. At one-month, one episode of VT was recorded resulting in three ATPs and one shock. No more arrhythmias were seen during the five months of follow-up (Figure 1B). Blood pressure remained stable during the whole follow-up period.
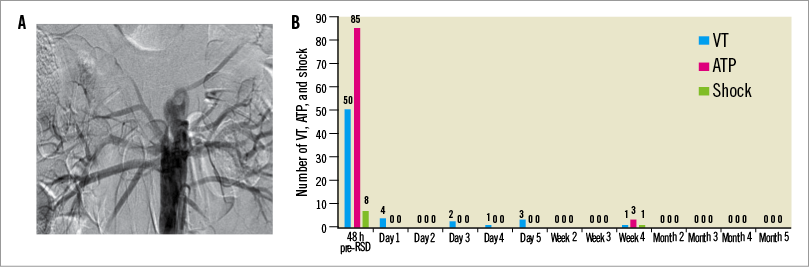
Figure 1. Bilateral renal angiogram and episodes of ventricular arrhythmia on ICD interrogation. A) Angiogram showing multiple renal arteries. B) VT episodes, ATP events and shocks before and after RSD. ATP: anti-tachycardia pacing; RSD: renal denervation; VT: ventricular tachycardia
Although sympathetic activity was not measured directly, the efficacy of RSD was indirectly observed by significant reduction of VA and increased vagal nerve activity measured by spectral analysis of 24 hr Holter monitoring. Bilateral renal nerve ablation increased the indices of vagal nerve activity (high frequency component of heart rate variability [HRV], 77.45 [18.8] and 87.69 [13.02] at baseline and after RDN, respectively, p=0.04) and there was a trend towards reduction in sympathetic nerve activity (low frequency component of HRV, 19.27 [10.93] and 12.3 [13] at baseline and after RDN, respectively, p=0.06).
Despite the fact that no definitive therapeutic recommendations can be made, our findings illustrate the relevance of sympathetic activation in patients with VA and confirm the feasibility and potential efficacy of RSD in patients with electrical storm and multiple accessory renal arteries.
Conflict of interest statement
The authors have no conflicts of interest to declare.

