Abstract
The autonomic nervous system (ANS) has a pivotal role in the pathogenesis and maintenance of atrial and ventricular arrhythmias. Catheter-based renal denervation (RDN) is associated with a reduction of central sympathetic activity, muscle sympathetic nerve activity, and blood pressure in resistant hypertension. As renal afferent nerves are regulators of central sympathetic tone, RDN opens the possibility to modulate sympathetic activity, but without affecting peripheral chemoreceptors and mechanoreceptors in the heart and other organs. RDN was shown to reduce heart rate in humans and to reduce inducibility of atrial fibrillation (AF) as well as ventricular rate during AF in experimental studies. First evidence indicates that pulmonary vein isolation in combination with RDN increases the rate of AF freedom in patients with resistant hypertension. Furthermore, RDN may have a beneficial impact on ventricular arrhythmia, in particular in patients with coronary artery disease or heart failure.
Introduction
The autonomic nervous system (ANS) is a physiological modulator of cardiac electrophysiology, as it influences physiological cardiac properties such as chronotropy, inotropy, and dromotropy. However, it plays a detrimental role in the development and maintenance of atrial and ventricular arrhythmias1,2. The cardiac ANS consists of a complex network of sympathetic and parasympathetic nerve fibres, which synapse in the extrinsic and intrinsic cardiac ganglia and finally innervate cardiac myocytes3.
Various new treatment approaches modulating autonomic tone are emerging. Renal sympathetic afferent and efferent nerves are important mediators of central sympathetic activity4. Percutaneous catheter-based renal sympathetic denervation (RDN) reduces blood pressure5,6 and improves glucose metabolism in resistant hypertension7 and has been associated with a reduction of renal and whole-body sympathetic activity8. This review addresses the link between the autonomic regulation of the heart and the kidneys and highlights the possible implications of RDN as a new treatment option for atrial and ventricular arrhythmias.
Autonomic innervation of the heart
The nervous system of the heart consists of extrinsic and intrinsic ganglia3. Mechanical stress receptors, baroreceptors, and chemoreceptors located in the heart and great vessels modulate autonomic tone3. The extrinsic cardiac nervous system is divided into a sympathetic component, originating in the cervical spinal cord, and a parasympathetic component from the vagus nerve3. Sympathetic nerves in the heart are either preganglionic (originating from the spinal cord) or postganglionic (coming from the stellate ganglion)9. On the whole, sympathetic stimulation of the heart activates postganglionic fibres in the sinus node, atrioventricular node and in the contractile tissue. The intrinsic nervous system consists of cardiac ganglia, where the preganglionic sympathetic nerves and all parasympathetic nerves synapse. Groups of ganglia form a complex neural network composed of ganglionated plexi, which are located in the atria in multiple locations and in the ventricle primarily associated with the origins of the great cardiac blood vessels3. Ganglionated plexi modulate the interactions between the extrinsic and intrinsic nervous system and mediate the efferent signalling to the atrial and ventricular myocardium10.
Role of the kidneys for central sympathetic activity
The kidney communicates with the systemic sympathetic nervous system via the renal sympathetic afferent nerves4. Triggered by renal ischaemia or other intra-renal pathology, renal afferent nerve activity directly influences systemic sympathetic drive by modulating posterior hypothalamic activity11. Interruption of the connection between the brain and kidney has been seen in preclinical trials to have salutary effects on blood pressure, and the systemic consequences of sympathetic overactivity11. Clinical evidence on the interaction between renal and central sympathetic activity came from patients with end-stage renal disease after nephrectomy, where elevated muscle sympathetic nerve activity is reduced close to the activity in normal individuals12. The ability to denervate the renal efferent and afferent sympathetic nerves by RDN influences not only renal but also central sympathetic activity8 and thereby affects blood pressure5, glucose metabolism7 and heart rate (Figure 1)13. It has been shown that RDN can reduce whole-body norepinephrine spillover by 42% and efferent muscle sympathetic nerve activity by 66%8,14. As a source of central sympathetic tone the kidneys open the possibility to eliminate the renal sympathetic afferent fibres selectively without affecting peripheral chemoreceptors and mechanoreceptors in the heart or other organs. The preserved response to cardiopulmonary exercise after RDN without affecting the physiological rise of blood pressure and heart rate may be regarded as sign of intact cardiac autonomous function following RDN15.
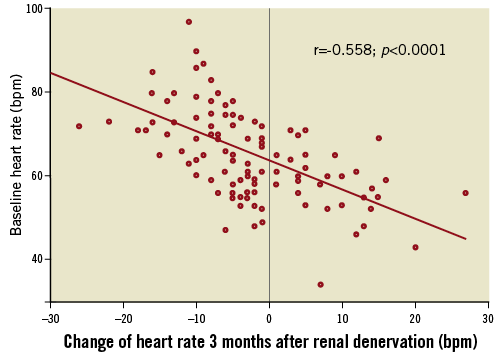
Figure 1. Correlation between heart rate at baseline and change of heart rate three months after renal denervation in patients with resistant hypertension. Higher baseline heart rate was associated with a greater reduction after RDN, whereas heart rates ≤60 beats per minute at baseline resulted in no change13.
Renal denervation as treatment for supraventricular arrhythmias
In the atrium, the ANS affects important electrophysiological properties such as chronotropy and dromotropy1. It is well known that sympathetic activity increases heart rate (HR) and facilitates atrioventricular conduction whereas parasympathetic activity counterbalances these effects16. In heart failure, sinus tachycardia could be recognised as a sign of elevated cardiac sympathetic tone17. Recent studies demonstrated that HR reduction without additional systemic effects results in an improvement of cardiovascular mortality in patients with heart failure18,19. A reduction of sympathetic activity mediated by RDN may therefore have beneficial electrophysiological effects. We recently reported HR reduction of 2.6±0.8 beats per minute (bpm) at three months and of 2.1±1.1 bpm after six months in 136 patients with resistant hypertension undergoing RDN13. Heart rate at baseline correlated with change of HR after RDN (Figure 2). In patients with heart rate >71 bpm, heart rate reduction was 8.5±1.4 bpm. Interestingly, blood pressure reduction was not associated with HR changes. Additionally, the atrioventricular conduction was affected by the reduction of sympathetic activity after RDN. The PR interval was prolonged by 11.3±2.5 and 10.3±2.5 ms at three and six months after RDN, respectively. Patients with a more pronounced PR prolongation had a greater HR reduction showing the relation between these changes. Twenty-one patients (17%) fulfilled the criteria for a newly diagnosed first-degree atrioventricular block (AVB) during follow-up. Spontaneous first-degree AVB as marker of structural cardiac abnormalities, such as atrial fibrosis and calcification, is associated with a higher risk of future atrial fibrillation and pacemaker implantation20. In contrast, short-term PR changes due to RDN are regarded as benign signs of reduced sympathetic activity21.
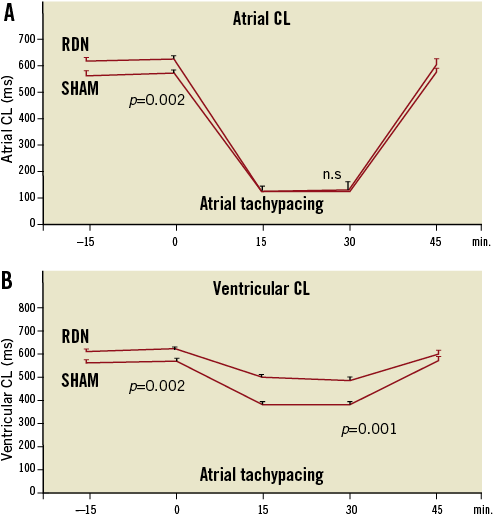
Figure 2. Effect of RDN on atrial cycle length (CL) (A) and ventricular CL (B) after renal denervation or sham procedures. Rapid pacing induced AF without changing the atrial CL (A), but significantly prolonged the ventricular CL (B). This provides evidence for improved ventricular rate control during AF35.
Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia encountered in clinical practice and is a frequent complication in patients with hypertension22,23. There are data indicating that the ANS potentially plays a detrimental role in the initiation and maintenance of AF, although electrical remodelling of the atria may not be influenced by autonomic tone24-26. Importantly, not only one arm of the ANS but also –and even more importantly– the interaction between both can induce AF and also seems to be one factor stabilising AF27. An increased parasympathetic tone results in a shortening of the atrial effective refractory period (AERP) thereby creating a substrate for re-entries, whereas sympathetic tone enhances spontaneous triggered activity28. The predominant autonomic cause –sympathetic or vagal– depends on the presence of comorbidities3. A parasympathetic predominance is common in the absence of organic heart diseases25. In these patients, AF typically occurs during sleep, when parasympathetic tone is predominant25. On the other hand, in patients with comorbidities such as hypertension, coronary artery disease, and heart failure, AF is associated with elevated sympathetic tone3. Patients with obstructive sleep apnoea (OSA) characteristically have a profound sympathovagal dysbalance29. Bradycardia and atrioventricular conduction disturbances in combination with postapnoeic blood pressure rises during awakening illustrates the interplay between parasympathetic and sympathetic activation in these patients29,30. As a consequence, OSA is associated not only with a high prevalence of AF but also with hypertension31,32. In the light of these considerations, modulation of the autonomic activity could be beneficial in these patients. In a small population of patients with resistant hypertension and OSA, RDN was able to reduce blood pressure and severity of OSA measured by the apnoea-hypopnoea index33. We presented experimental data supporting this approach34. In a pig model for OSA, negative tracheal pressure (NTP) induced AERP shortening and increased AF inducibility. Combined surgical and chemical denervation of the kidneys resulted in a reduced BP rise after NTP and attenuated the AERP shortening induced by NTP. This was associated with a markedly reduced AF inducibility in RDN treated pigs compared to atenolol treatment and to a sham group. In another model for paroxysmal AF by repetitive atrial stimulation, RDN has been shown not only to reduce the duration of induced AF episodes, but also, in particular, to lead to an improvement of ventricular rate control (Figure 3)35. Similar results on the inducibility of AF were observed by another group in a dog model of AF36.
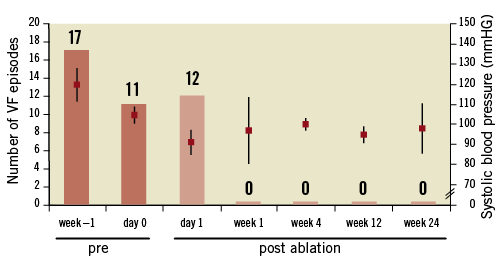
Figure 3. Number of ventricular tachycardia and fibrillation episodes before and after RDN in a patient with electric storm and dilated cardiomyopathy. After 24 hours after RDN VF episodes did not reoccur in the next six months. Blood pressure during procedure and follow-up remained stable with a mean systolic blood pressure of 101 mmHg. VF: ventricular fibrillation or polymorphic ventricular tachycardia58.
In clinical practice pulmonary vein isolation (PVI) is an effective and established treatment for symptomatic AF23. However, one main drawback is the rate of recurrence of atrial tachyarrhythmias after PVI, which depends on the type of AF and prevalence of comorbidities, including uncontrolled hypertension37 The mechanism of recurrent atrial arrhythmias after PVI is most commonly pulmonary vein reconnection. However, some data indicate a post-ablation modulation of sympathetic cardiac innervation and electroanatomical remodelling of the atria37. Consequently, RDN as treatment for patients with AF is currently under investigation38-40. Besides a possible change of autonomic tone, RDN has further beneficial effects in patients with hypertension, which may indirectly reduce AF recurrence after PVI: hypertension and increased atrial size were identified as predictors of poor outcome following PVI37. Reduction and control of BP5, 6 reduction of left ventricular hypertrophy, and improvement of diastolic function41, all possibly affecting atrial size, have been described in treatment-resistant hypertensives after RDN. All these beneficial changes may lead to reduced electrical, structural, and mechanical remodelling of the left atrium, which has a positive impact on the AF recurrence rate after PVI. The first clinical evidence came from Pokushalov et al38 investigating the additive effect of RDN in patients with symptomatic AF and resistant hypertension undergoing PVI. In this study, 27 patients were enrolled and randomised to either PVI alone or PVI in combination with RDN. Besides a significant reduction of SBP (from 181 to 156 mmHg, p<0.001) the rate of AF freedom at 12 months was also significantly higher in the PVI+RDN group (69% vs. 29%; p=0.033) compared to PVI alone38.
These first results led to the initiation of a multicentre trial (H-FIB) investigating the adjunctive effect of RDN at the time of AF ablation40. In this trial, 300 patients with AF and hypertension (defined as SBP ≥160 mmHg and/or DBP ≥100 mmHg) receiving at least one medication will be enrolled. In contrast to the study by Pokushalov et al38 patients in this study will have uncontrolled hypertension, but do not necessarily need to fulfil criteria of treatment resistance. After standard PVI, patients will be randomised to additional RDN in the same session or sham procedure. The primary endpoint will be freedom from AF recurrence (without antiarrhythmic drugs) for 12 months. The secondary endpoints will include freedom from AF for 24 months, echocardiographic measurements of left ventricular hypertrophy and left atrial size, BP changes and antihypertensive medication, as well as major adverse cardiac events.
Although H-FIB is a pivotal trial advancing our knowledge on AF as well as on RDN, one drawback in the study design should be noticed: the RDN procedure will be performed with the same irrigated-tip radiofrequency catheter which was used for PVI. Although first data on the use of this catheter for RDN were recently published, no safety and efficacy data over a longer period of time exist unlike the standard RDN devices42. Development and progression of renal artery stenosis has been reported in two case reports with approved RDN devices43,44. It is currently unknown whether non-purpose-designed cardiac ablation systems for RDN have a higher or lower procedural and long-term risk45. Additionally, in the event that H-FIB becomes a negative trial, it will remain unknown to what extent this negative outcome will be attributable to an incomplete ablation of renal sympathetic nerve fibres using a cardiac ablation catheter.
Sympathomodulatory treatments for ventricular arrhythmias
The ANS plays a relevant role in the onset, maintenance and interruption of ventricular arrhythmias46. In particular in patients with comorbidities such as hypertension, diabetes, coronary artery disease, and myocardial infarction, an autonomic dysbalance leads to a higher risk of ventricular arrhythmias47. In general, sympathetic activity facilitates ventricular arrhythmias, whereas vagal tone normally suppresses them46. The shortening of effective ventricular refractory period and thereby allowing re-entry circuits, increased ventricular automaticity, and reduction of the threshold for ventricular arrhythmias are regarded as potential mechanisms of arrhythmogenesis by elevated sympathetic tone48
Myocardial infarction for instance, may cause an area of sympathetic denervation by interruption of nerve fibres traveling through the lesion. This was demonstrated by iodine-123 metaiodobenzylguanidine nuclear studies which showed a decreased distribution and activity of sympathetic nerves in areas of infarction compared to healthy tissue49. Additionally, nerve injury may trigger excessive regeneration via nerve sprouting in this area50. This may be related to inhomogeneous and hypersensitive sympathetic innervation in particular in the border zones of scars which may be the source of premature ventricular contractions thereby initiating ventricular arrhythmias46. Ventricular arrhythmias are associated with regional cardiac hyperinnervation and may also indicate a hypersensitivity to central sympathetic tone51.
Therapies aiming at reducing sympathetic activity may potentially protect against ventricular arrhythmias. Surgical excision of the left ganglion stellatum (left cardiac sympathetic denervation) is considered in high-risk patients with the long QT syndrome and may be considered in the rare event of repetitive catecholamine-sensitive ventricular tachycardias despite the use of ß-blockers52,53. Bilateral cardiac sympathetic denervation may be performed in cases where left cardiac sympathetic denervation was not effective in suppressing ventricular arrhythmias54. With increasing use of implantable cardioverter defibrillators (ICD) the number of patients experiencing ventricular arrhythmias is rising55. Recurrent ventricular arrhythmias are associated with an impairment of quality of life and poor prognosis56,57. We recently reported treatment of electrical storm by RDN in two patients as first-in-man experience58. Both patients had symptomatic heart failure (NYHA class III) and suffered from recurrent episodes of ventricular arrhythmias. Cardiac ablation therapies failed or were declined, therefore RDN was performed as an experimental attempt to reduce ventricular arrhythmia burden. In both cases, RDN did not result in any apparent acute or chronic haemodynamic complications in these normotensive patients. Ventricular arrhythmias were markedly reduced in both patients following the procedure (Figure 3). As sympathetic activity was not measured directly, the efficacy of RDN was indirectly observed via an improvement of the glycaemic status of one patient with diabetes7. Further studies investigating RDN for treatment of ventricular arrhythmias and electric storm are necessary and ongoing.
Notably, the majority of patients experiencing ventricular arrhythmias have underlying structural heart disease and suffer from heart failure. Pathophysiologically, heart failure is characterised by neurohumoral activation, including chronic activation of the central sympathetic nervous system59. A first-in-man experience investigating RDN in heart failure was recently published suggesting the safety of the procedure60. A large randomised multicentre trial (RE-ADAPT-CHF) is ongoing and is also investigating the effects of RDN on arrhythmia burden as well as cardiac and renal function as the main safety and efficacy endpoints.
Conclusion and perspective
The autonomic nervous system is substantially involved in the genesis and maintenance of atrial and ventricular arrhythmias. Physicians are challenged by unresolved issues such as the recurrence rates of AF after PVI and the rising prevalence of ventricular arrhythmia burden in heart failure. Modulation of central sympathetic activity by RDN raises new hopes. However, the contribution of kidney-mediated sympathetic activity to the initiation and maintenance of arrhythmias remains unclear. If arrhythmias occur in the context of significant comorbidities such as AF in hypertension or OSA, or ventricular arrhythmias in heart failure, a relevant contribution of the kidneys to central sympathetic drive is conceivable. In these disease states, renal sympathetic innervation is a therapeutic target that deserves further clinical investigation. However, data demonstrating an elevated renal sympathetic activity in arrhythmias are lacking. Besides safety and efficacy, the mechanism of the antiarrhythmic effects of RDN needs to be illuminated. Is reduction of sympathetic activity or maybe just improved BP control the key mechanism for success in hypertensive patients undergoing AF ablation? With RDN a new and probably antiarrhythmic tool has become available that definitely deserves to be investigated.
Funding
C. Ukena, F. Mahfoud, M. Böhm and H.R. Neuberger are supported by the Ministry of Science and Economy of the Saarland. M. Böhm is supported by the Deutsche Forschungsgemeinschaft (KFO 196). F. Mahfoud is supported by Deutsche Hochdruckliga und Deutsche Gesellschaft für Kardiologie.
Conflict of interest statement
C. Ukena, F. Mahfoud, M. Böhm and H.R. Neuberger have received speakers’ honoraria from Medtronic. D. Linz has no conflicts of interest to declare.