Abstract
Aims: Our objective was to evaluate the relationship between coronary chronic total occlusion (CTO) treatment strategy and quality of life improvements.
Methods and results: This multicentre prospective cohort study enrolled consecutive CTO patients undergoing a non-urgent coronary angiogram who completed the Seattle Angina Questionnaire (SAQ) and EQ-5D at baseline and at one year. Strategies were: i) medical therapy, ii) PCI to non-CTO, iii) PCI to CTO, and iv) CABG. Multivariable regression models compared quality of life changes over time among strategies, accounting for repeat measures per patient. In our cohort of 387 patients, 154 underwent medical therapy, 83 had PCI to the non-CTO artery, 104 underwent CABG, and 46 underwent PCI to the CTO. Medically treated patients had no improvement on any SAQ domains. Patients with revascularisation of the CTO territory with either PCI or CABG had significant improvements in the physical limitation (PCI to CTO 60.5-76.4; CABG 61.6-80.1; p<0.001), angina frequency (PCI to CTO 79.0-92.7; CABG 82.1-97.9; p<0.001), and disease perception (PCI to CTO 50.5-75.0; CABG 50.2-80.0; p<0.001) domains. In non-CTO PCI patients, improvement was restricted to the angina frequency (82.8-93.3; p<0.001), and disease perception (53.8-71.4; p<0.001) domains.
Conclusions: CTO territory revascularisation was associated with quality of life improvements.
Introduction
Coronary chronic total occlusions (CTOs) are common, with approximately 18-33% of patients with significant coronary disease on coronary angiography having at least one CTO1,2. Despite this, there remains substantial uncertainty as to whether CTO territories should be revascularised and, if so, by which modality.
The therapeutic nihilism surrounding CTO is in part due to the substantial technical difficulties in addressing CTO lesions with percutaneous coronary intervention (PCI), which has traditionally had success rates of only 50%. Furthermore, there is a hesitation to offer coronary artery bypass graft (CABG) surgery to patients who may not have multivessel disease2-6. Over the last decade there has been tremendous progress in the techniques and equipment available for percutaneous management of CTO, such that rates for successful recanalisation with PCI by expert operators are greater than 80%4,5,7,8. Due to this rapid evolution in technology and techniques available for percutaneous management of CTO, there has been limited randomised evaluation in this area; therefore, observational studies remain highly relevant.
Coupled with the historical difficulty of treating CTO, contemporary landmark studies in patients with stable angina suggest that there is no mortality benefit for revascularisation compared to medical therapy9,10. As such, improvements in quality of life outcomes may be the most relevant indication for revascularisation of CTO in non-urgent coronary disease. However, there is a paucity of data on quality of life outcomes in patients with CTO, with only two studies in the published literature, both of which were restricted to CTO patients after an attempt at PCI11,12. There is a pressing need to address this gap in knowledge.
Accordingly, our objective in this prospective cohort study was to evaluate changes in generic and cardiac-specific quality of life over one year in patients with at least one CTO on non-emergent coronary angiography, comparing patients with aggressive revascularisation of the CTO territory (with either CABG or PCI) versus those with conservative management. This study was approved by the institutional research ethics board at each of the participating hospitals.
Methods
DATA SOURCE
Our study cohort consisted of consecutive patients with non-emergent coronary artery disease who underwent coronary angiography at the Schulich Heart Center, Sunnybrook Health Sciences Centre in Toronto, Ontario, Canada, or as part of the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease (APPROACH) registry. The APPROACH registry collects demographic and clinical information on all patients who undergo a diagnostic angiogram at three hospitals in the province of Alberta, Canada13. Patients were accrued from the APPROACH database between April 1st 2008 and July 31st 2009 and at Sunnybrook Health Sciences Centre from December 1st 2008 to August 31st 2009.
Data were abstracted (Toronto cohort) and retrieved (APPROACH registry) on socio-demographic features, comorbidities, baseline medications, coronary anatomy, left ventricular (LV) function, availability of a pre-procedural stress test, and presence of Q-waves on electrocardiogram. In addition, patients completed two quality of life surveys, the Seattle Angina Questionnaire (SAQ) and the EQ-5D at baseline, with follow-up after one year.
MEASURES
SEATTLE ANGINA QUESTIONNAIRE (SAQ)
The SAQ is a 19-item descriptive, self-administered questionnaire that focuses on symptoms and impairments in health unique to coronary disease14. The five dimensions of coronary artery diseases that are measured include physical limitation, anginal stability, anginal frequency, disease perception and treatment satisfaction14. Ordinal scores on the questionnaire are transformed to continuous scale, from a low score of 0 to maximum score of 10014. The scores of each dimension are analysed separately, with a high score indicating better quality of life.
EQ-5D
This scale expresses preference for health status using a single index score and it is the tool recommended by the National Institute for Health and Clinical Excellence (NICE) for calculation of utility weights for economic evaluations15,16. The score has two anchors, with a low score of 0 representing death, and an upper ceiling of 1, representing perfect health16. The EQ-5D covers five dimensions of health: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression16. Each dimension is measured using a three-level ordinal scale, and a unique health state is defined by a combination of scores on each of the five dimensions16. A score for each of the 243 potential health states is calculated by applying a country-specific tariff. In this analysis, we used US tariffs16.
TREATMENT CATEGORY
Patients were assigned to one of four treatment strategies based on actual treatment intention within 30 days of index angiogram: i) medical therapy, ii) PCI to the non-CTO artery, iii) PCI to the CTO, and iv) CABG. Treatment strategies were broadly dichotomised into those involving aggressive treatment of the CTO territory (PCI to CTO, and CABG), or conservative treatment of the CTO territory (PCI to non-CTO, and medical therapy). If a patient received a PCI to the CTO artery after a non-CTO PCI, both within the 30-day period of interest, they were assigned to the PCI to CTO category as this probably represented a planned staged procedure. However, if they received a CABG after a non-CTO PCI or a CTO PCI, the CABG was probably emergent in nature, and therefore these patients were not reclassified. If PCI to the CTO was not successful or if the CTO area was not bypassed by CABG, they remained in the intention to treat category.
ANALYSIS
MISSING DATA
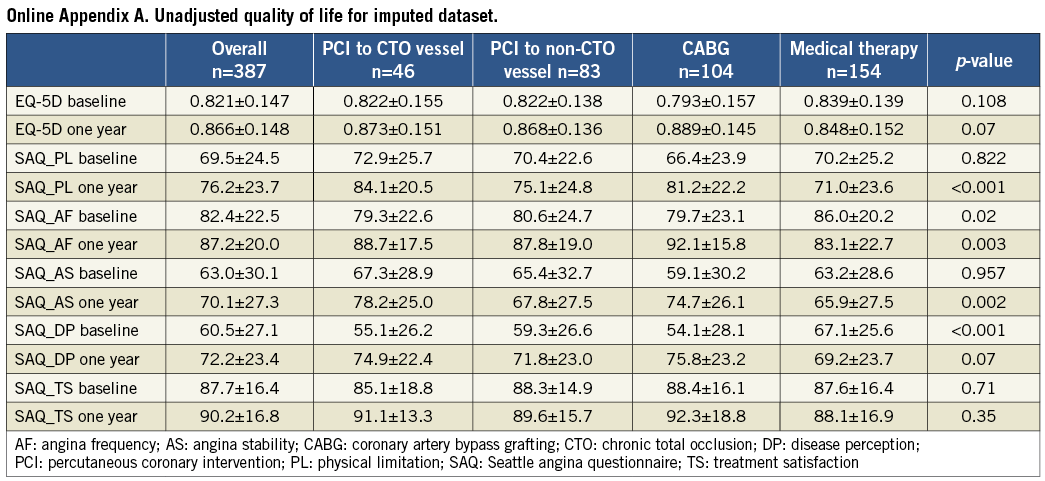
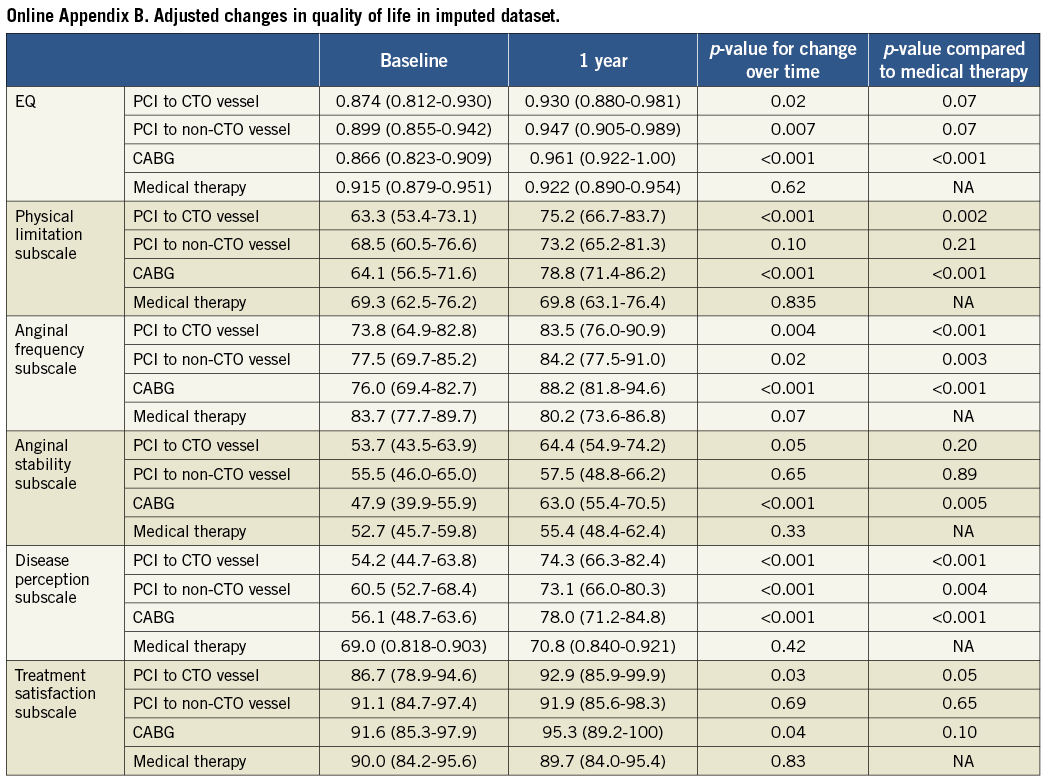
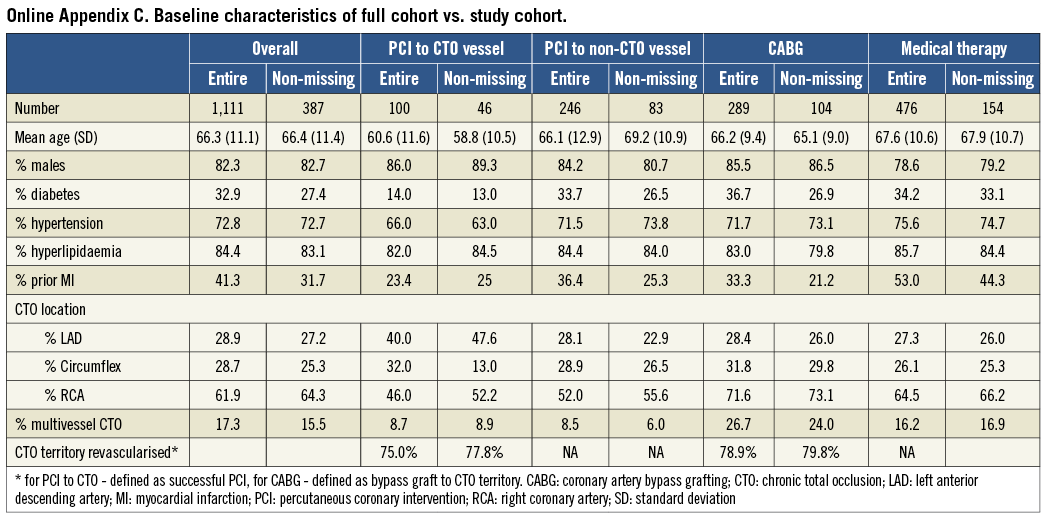
In our primary analysis, we only report on patients who returned the quality of life surveys. Based on previous publications, we anticipated that approximately 75-85% of patients who completed the surveys would have complete data on all questions for both the SAQ and the EQ-5D17,18. We performed a sensitivity analysis to determine if our conclusions were overly biased by incomplete data. In the patients who returned the quality of life surveys, but had missing data in the EQ-5D or in any of the subscales of the SAQ, we created five imputed datasets, using Markov chain Monte Carlo methods to impute missing data, which were assumed to be missing at random. Our subsequent regression modelling (outlined below) was performed on each dataset. These results are provided in Online Appendix A and Online Appendix B, and show no qualitative difference conclusions. In addition, we compared the baseline characteristics of the entire cohort of CTO patients to those of the patients who returned the surveys (Online Appendix C), and found them to be similar.
MODEL DEVELOPMENT
Comparison of baseline characteristics between patients in each treatment group was evaluated using analysis of variance (ANOVA) for normally distributed continuous data, and chi-square or Fisher’s exact tests for categorical data. For unadjusted analysis of quality of life scores, we compared mean baseline and one-year scores among the four treatment groups using ANOVA.
For our adjusted models, we created six multivariable regression models, each with the scores from one of the five domains of the SAQ or the EQ-5D as the response variable. The unit of analysis for all models was the individual patient, and the scores were treated as continuous variables. To account for the repeated/paired measures per patient, we used generalised estimating equation (GEE) methods, with each patient having both a baseline and one-year score. Variables included in the model were time (baseline vs. one year), treatment strategy (medical therapy, PCI to non-CTO, PCI to CTO, surgery) and the interaction between time and treatment strategy. In this manner, we were able to evaluate quality of life changes from baseline to one year for each treatment group, and changes between groups over time. The reference group for all between-group comparisons was the medical therapy group. Finally, a fully adjusted model comparing within and between group changes over time was developed, by forcing in all baseline characteristics (age, gender, diabetic status, hypertension status, hyperlipidaemia, history of previous MI, CTO location, presence of multivessel coronary disease or multivessel CTO, LVEF, and presence of Q-waves in the CTO territory) into the regression.
Statistical analyses were performed using SAS version 9.0 (SAS Corporation, Cary, NC, USA). Results were considered statistically significant with a two-sided p-value of <0.05.
Results
Over the 18 months of patient recruitment, CTOs were identified in 18.2% of all non-urgent coronary angiograms done at the participating institutions. Of these, 387 patients completed the quality of life instruments and constituted our study cohort. Baseline characteristics of the study cohort are found in Table 1. A minority of the study population had revascularisation of the CTO territory, with the majority undergoing medical therapy (n=154), 83 with PCI to the non-CTO artery, 104 undergoing CABG, and 46 undergoing PCI to the CTO. Of the patients undergoing CABG, 79.8% had a bypass graft to the CTO territory, while 77.8% of the patients with PCI to the CTO artery had successful PCI recanalisation. The majority of patients had a CTO in the right coronary artery (RCA) with 15.2% of patients having CTOs in more than one coronary artery. Most patients had preserved LV function (54.1%) and a minority (12.9%) had Q-waves in the CTO territory. Stress testing was done in 61.1% of all patients, in the majority of whom the test was positive for ischaemia (95%).
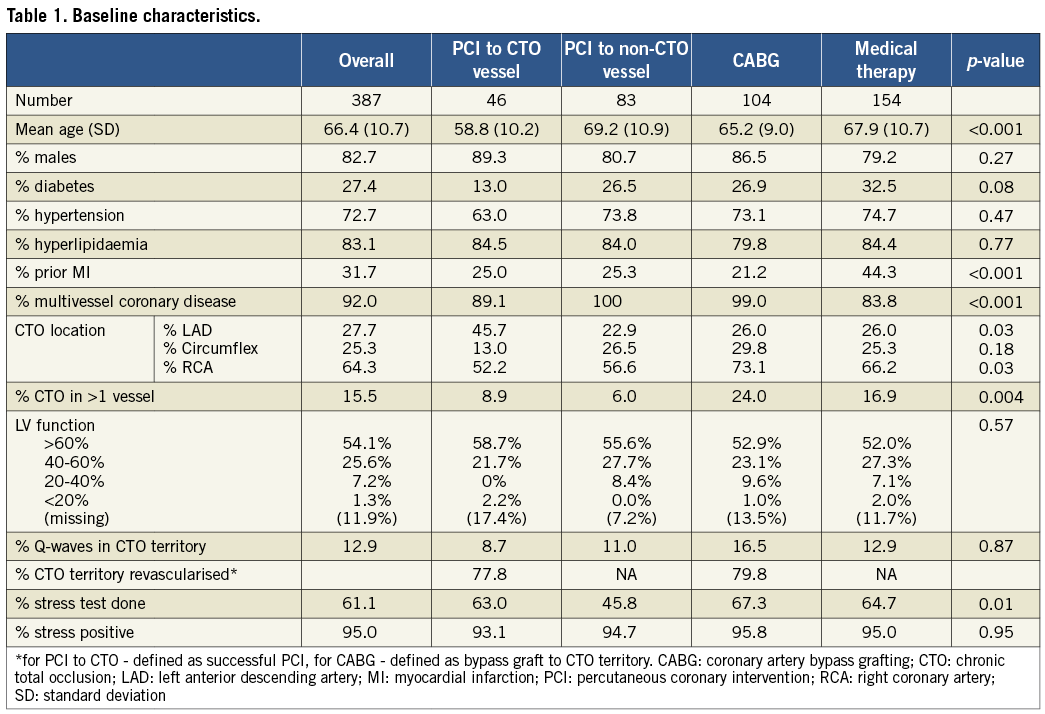
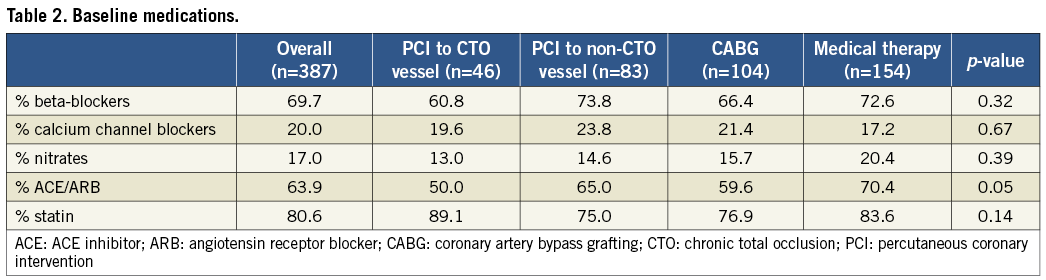
There were important differences among patients in the four treatment categories. Patients who underwent a PCI to the CTO artery were younger, with a mean age of 58.8 years, compared to 66.4 years for the overall group. In general, these patients had fewer comorbidities, with 13% having diabetes mellitus and 25% with a previous MI, compared to 27.4% and 31.7% for the overall group. In Table 2, baseline anti-ischaemic and secondary prevention medications are summarised for each treatment strategy. Although 69.7% of patients were on β-blockers, substantially lower proportions were on calcium channel blockers (20%) or nitrates (17%). There was no statistically significant difference between groups. In contrast, most patients were on appropriate secondary prevention medications, with 63.9% on either ACE inhibitors or angiotensin receptor blockers (ARB), and 80% on a statin medication.
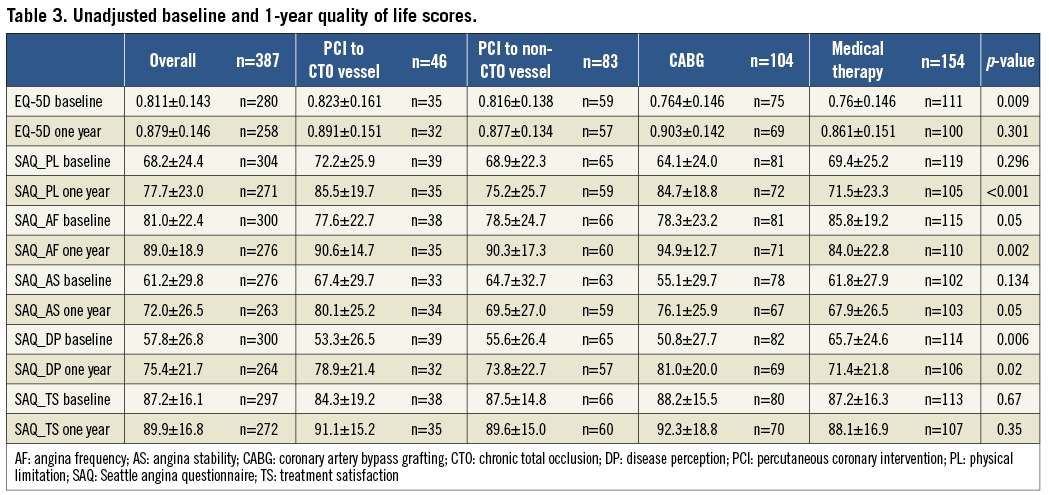
Baseline and one-year unadjusted scores on the quality of life instruments are found in Table 3. In general, patients with CTO had moderate amounts of angina, with a mean score of 81.0 on the angina frequency subscale of the SAQ. The impact of these symptoms on their overall disease perception was substantial with a baseline score of only 57.7 in this subscale. Nonetheless, there was a substantial range in both baseline symptomatology in the overall CTO group and between patients in each of the treatment strategies.
ADJUSTED MODELS
The results of our adjusted regression models are shown in Figure 1 and Figure 2, with adjusted mean quality of life scores shown for each treatment strategy both at baseline and one year. In each model, we assessed changes in quality of life both over time from baseline to one year, and in comparison to patients treated with medical therapy, our reference group.
In generic health-related quality of life, as measured by the EQ-5D, patients in all treatment categories except medical therapy had statistically significant improvements at one year compared to baseline (Figure 1). However, when contrasting treatment groups, only patients who underwent CABG (0.921 at one year vs. 0.787 at baseline) had a significant improvement compared to patients who were treated medically (0.880 at one year vs. 0.861 at baseline).
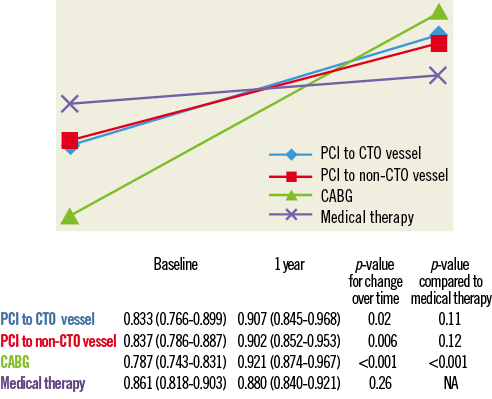
Figure 1. Changes in EQ-5D. PCI: percutaneous coronary intervention; CTO: chronic total occlusion; CABG: coronary artery bypass grafting. EQ-5D is measured between 0 and 1, with 1 indicating better quality of life.
In the cardiac-specific quality of life domains of the SAQ, substantial differences were observed between the treatment groups. As seen in Figure 2, patients treated with medical therapy generally had higher scores (i.e., better) at baseline in physical limitation, angina frequency and disease perception. However, medically treated patients had no statistically significant change in score on any of the SAQ domains over one year.
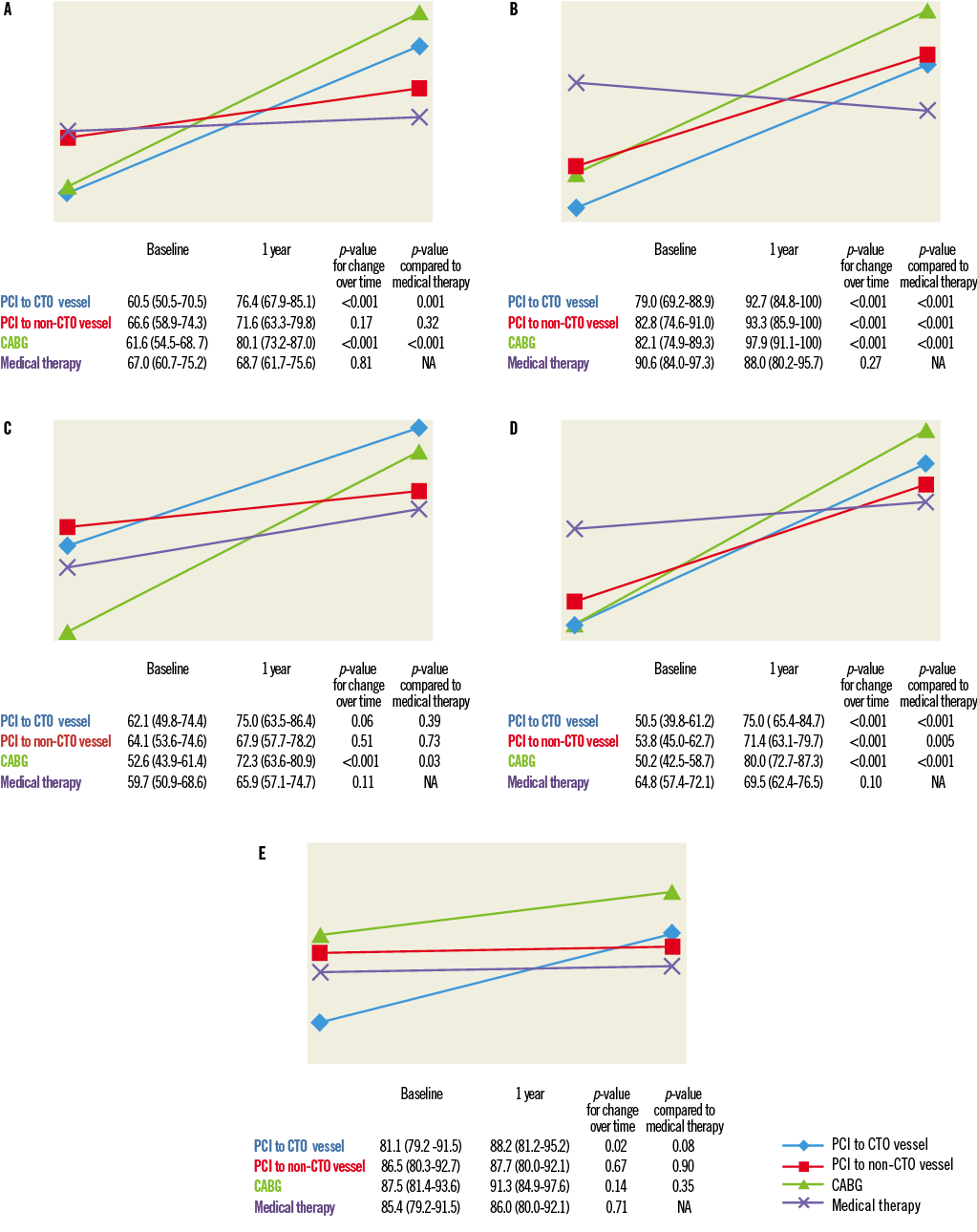
Figure 2. Seattle Angina Questionnaire changes. A) Changes in physical limitation sub-domain of Seattle Angina Questionnaire. B) Changes in anginal frequency sub-domain of Seattle Angina Questionnaire. C) Changes in anginal stability sub-domain of Seattle Angina Questionnaire. D) Changes in disease perception sub-domain of Seattle Angina Questionnaire. E) Changes in treatment satisfaction sub-domain of Seattle Angina Questionnaire. SAQ is measured between 0 and 100, with 100 indicating better quality of life. PCI: percutaneous coronary intervention; CTO: chronic total occlusion; CABG: coronary artery bypass grafting
In contrast, patients with revascularisation of the CTO territory by either PCI or CABG had improvements over time in the majority of the SAQ domains: physical limitation, angina frequency, angina stability and disease perception. In addition, patients with PCI to the CTO were the only group to have improvements in treatment satisfaction over time (88.2 at one year vs. 81.1 at baseline; p-value 0.02). When compared to medical therapy patients, patients with PCI to the CTO or CABG had significant improvements in most of the SAQ domains, including physical limitation, disease perception, angina frequency, and disease perception.
For the patients in whom PCI was performed to the non-CTO artery, there were mixed effects in the cardiac-specific quality of life indices. There was improvement over time in angina frequency, and disease perception, both of which were significant compared to medical therapy patients. However, these were of a lesser degree than those of patients in the PCI to CTO and CABG groups.
Discussion
In this prospective cohort study of patients with CTO, we found that patients with CTO revascularisation by either PCI or CABG had significant improvements in quality of life indices compared to patients treated medically or with only limited revascularisation. However, fewer than 50% of patients had an attempt to revascularise the CTO artery territory; as such, there is opportunity for more aggressive treatment of these patients.
CTOs are considered the “last frontier” of PCI. The predominant focus of initial studies in this area was on whether these lesions could be treated percutaneously4,5. With the development of novel techniques with acceptable safety profiles, there has been a shift in focus to whether these lesions should be treated19. To this end, observational studies have shown improved survival in successful versus failed PCI of a CTO20. Moreover, indirect evidence from studies comparing complete versus incomplete revascularisation by either surgery or PCI reinforce the potential prognostic improvements associated with CTO intervention. However, given the absence of randomised trial data, these indications are controversial. Appropriateness guidelines for coronary revascularisation published by the American College of Cardiology and other groups reflect this uncertainty, with the majority of scenarios involving CTOs scored as having uncertain indications for revascularisation21.
Health status and quality of life indices are increasingly used in cardiovascular studies, and reflect the increasing importance of these patient-perspective endpoints as an indication for therapy. Although some studies have shown reduction in angina, as quantified by the healthcare provider, there are only two studies in the literature evaluating health status changes in CTO patients11. In their study published in 2011, Grantham and colleagues compared CTO patients with successful versus failed PCI in the FlowCardia Approach to CTO Recanalization (FACTOR) trial11. In the 55% of patients with successful PCI, they found a statistically significant improvement in the SAQ domains over a one-month period, compared to those with a failed procedure11. This improvement was principally in symptomatic patients11. This is similar to what Borgia and colleagues found in their study of 302 consecutive CTO patients treated with PCI12.
We have extended this previous knowledge by evaluating the relationship between CTO territory revascularisation and health status changes. Particular strengths of our study are its generalisability, in that we evaluated patients undergoing all potential treatment options available to providers, including PCI to the non-CTO artery. This treatment modality is frequently favoured by PCI operators, given its relative technical ease compared to PCI of the CTO artery. Indeed, almost a quarter of CTO patients in our study received this option. In addition, we did not exclude patients in whom aggressive treatment was planned, but not successful; in fact, 20% of both CABG and PCI to the CTO patients ultimately did not have revascularisation of the CTO territory. With the emergence of new, specialised CTO tools, we would expect this failure rate to decrease, and thus we may be underestimating the impact of CTO revascularisation in contemporary practice. Moreover, by evaluating health status changes over one year, we incorporate potential effects of restenosis and the time required for recovery from surgery.
Several novel insights follow from our study. First, despite the technical advances in CTO PCI and the improved safety profile and success rates, patients with CTO continue to be undertreated, with fewer than 50% of CTO patients having the CTO territory revascularised. Second, patients in whom the CTO territory was treated aggressively tended to have worse symptoms at baseline, but had substantial improvements with one-year health status that were greater than those in patients in whom the CTO territory was treated conservatively. Balanced against this is the fact that these patients were younger with fewer comorbidities. As such, it is unclear if this observation reflects appropriate patient selection based on baseline symptom severity, or a risk-treatment paradox, whereby sicker patients did not receive aggressive care. Further study is necessary to disentangle these complex issues.
Finally, patients who had PCI to the non-CTO territory had improvements in some quality of life domains, but of a lesser magnitude than more complete revascularisation; as such, our results suggest that this should be considered an interim option for CTO patients, with careful re-evaluation to ensure patients have improved adequately.
Our study must be interpreted in the context of several limitations that merit discussion. Although we had data on baseline medications, we lacked information on initial medication doses or on subsequent medication intensification; it is possible that the patients in the medical therapy arm were undertreated. Nonetheless, our findings represent real-world medication practice and, therefore, are probably generalisable. Ours was an observation dataset, and thus patients in each treatment group had non-balanced confounders. To deal with this selection bias, we used advanced statistical techniques for risk adjustment and were able to adjust for important variables such as CTO location, LV function, and presence of Q-waves. Importantly, we did not abstract data on anatomical complexity, using a reproducible and quantifiable scale such as the SYNTAX score. As such, we cannot exclude the possibility that there was residual confounding between the groups, due to such factors as anatomical complexity, which accounted for the differences we observed. Although Q-waves were similar between groups, viability testing was infrequently performed in our cohort; therefore, we were unable to adjust for this important variable. In addition, as our study was not blinded, there is the possibility of a placebo effect in patients who knew that their CTO was treated, either by PCI or CABG, which may have had an impact on their responses in the quality of life surveys. Finally, only a third of the overall group with CTO completed the quality of life surveys, and there was a substantial amount of missing data. However, in our sensitivity analyses we found the overall cohort to be similar to patients who completed surveys and, using multiple imputations to account for missing data, we found that our conclusions remained robust (Online Appendix A-Online Appendix C). Given these limitations, our observations should be considered hypothesis-generating, not confirmatory.
Conclusions
In conclusion, we found that aggressive revascularisation of the CTO territory by either PCI or CABG was associated with improvements in quality of life. Our findings suggest that more aggressive management of the CTO artery in patients with coronary occlusion may be warranted, especially in patients with multivessel disease, and reinforce the need for larger randomised studies in this highly prevalent patient population.
Acknowledgements
We acknowledge and thank Kimberley Lew and Param Narine for their invaluable assistance.
Funding
This work was funded in part by a Canadian Institute of Health Research (CIHR) Operating Grant MOP (102487) and Team Grant (CTP 82943). Dr Ko is supported by a New Investigator Award from CIHR. Dr Strauss holds the Reichmann Chair in Cardiovascular Sciences at Sunnybrook Health Sciences Centre, University of Toronto. Dr Wright is supported by a Tier 1 Canada Research Chair in Imaging for Cardiovascular Therapeutics.
| Impact on daily practice We found that coronary CTOs are relatively common in a multi-centre prospective registry and that the minority are revascularised by either CABG or PCI. Patients who did have revascularisation of the CTO territory had significant improvements in self-reported quality of life. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement