Transcatheter aortic valve implantation (TAVI) is increasingly used to treat younger patients with longer life expectancy. Consequently, it can be expected that a considerable portion of these patients will outlive their transcatheter aortic valve (TAV). In the event of TAV failure, redo-TAVI may be the preferred solution. However, redo-TAVI outcomes may vary depending on the patient’s anatomy and TAV-in-TAV combination. In this viewpoint, we highlight different TAV stent designs and leaflet positions and discuss their impact on specific aspects of TAV-in-TAV.
A first aspect to consider when planning redo-TAVI is that the leaflets of the first index TAV will be pushed aside by the second TAV, thereby creating a neoskirt-covered stent. The neoskirt height has important implications for the periprocedural risk of sinus sequestration and future coronary access12. As illustrated in Figure 1, the neoskirt height varies across different TAV designs and also depends on the implantation height of the second TAV, at least when the second TAV is a short-frame balloon-expandable valve (BEV). This is one of the main reasons why a BEV may be the preferred choice for redo-TAVI, as one can taper the neoskirt height to the patient’s anatomy and coronary ostia. Importantly, the functional neoskirt height will also vary according to the index TAV implantation depth. If the index TAV was implanted high relative to the aortic annulus, this will result in a higher functional neoskirt as compared to a low index TAV implantation3. This also explains the relatively low functional neoskirt in the case of BEV-in-ACURATE, as the nominal ACURATE (Boston Scientific) implant depth is 5-7 mm. In contrast, there is a trend to implant the Evolut TAV (Medtronic) ever higher, aiming to reduce conduction disorders; however, this results in a higher functional neoskirt in the case of redo-TAVI.
Besides the height of the neoskirt, the index TAV stent design above this neoskirt is also of importance in terms of coronary access4. In Figure 1, the lowest accessible stent frame cell in the case of BEV-in-self-expanding valve (SEV) implantation is indicated in green. The larger the SEV stent frame cells, the easier it should be to cannulate the coronary arteries selectively. Coronary access may also be more difficult in case of commissural misalignment of the index TAV and could be further compromised in case of misaligned SEV-in-SEV stent frames, as this would result in even smaller accessible cells above the neoskirt4.
Another aspect to be considered is the degree of index TAV leaflet overhang in case of BEV-in-SEV, especially if the BEV is implanted low; in this case, the index TAV leaflets may not be entirely pushed aside. This may result in considerable leaflet overhang, which may have an impact on valve performance and durability35. The extent of leaflet overhang that is acceptable and whether the index TAV failure mechanism (e.g., early failure with more mobile leaflets versus late failure with stiffer leaflets) is important are currently unknown. Figure 1 shows the degree of leaflet overhang for different TAV-in-TAV combinations. In the case of a low BEV-in-SEV implant, considerable leaflet overhang can be anticipated. This leaflet overhang could be minimised with a higher BEV implant, as long as the coronary access would not be threatened.
A final aspect to consider when using BEV for redo-TAVI is that this may result in further index TAV expansion and/or underexpansion of the second TAV2. The degree of possible index TAV expansion must be considered when performing preprocedural risk prediction of coronary obstruction at cardiac computed tomography analysis; however, different TAV types may be more (e.g., Evolut) or less (e.g., ACURATE) easy to expand further. Possible BEV underexpansion in case of redo-TAVI may result in leaflet “pinwheeling”, which can cause increased leaflet stress and reduced valve durability. However, these aspects need more (pre-) clinical investigations, before assigning specific recommendations.
In conclusion, when treating patients with longer life expectancy and/or planning redo-TAVI, it is of critical importance to consider the patient-specific anatomy of the aortic valve complex and be knowledgeable about TAV stent designs and leaflet positions. Several TAV-in-TAV aspects must be taken into account to obtain the best possible redo-TAVI outcome.
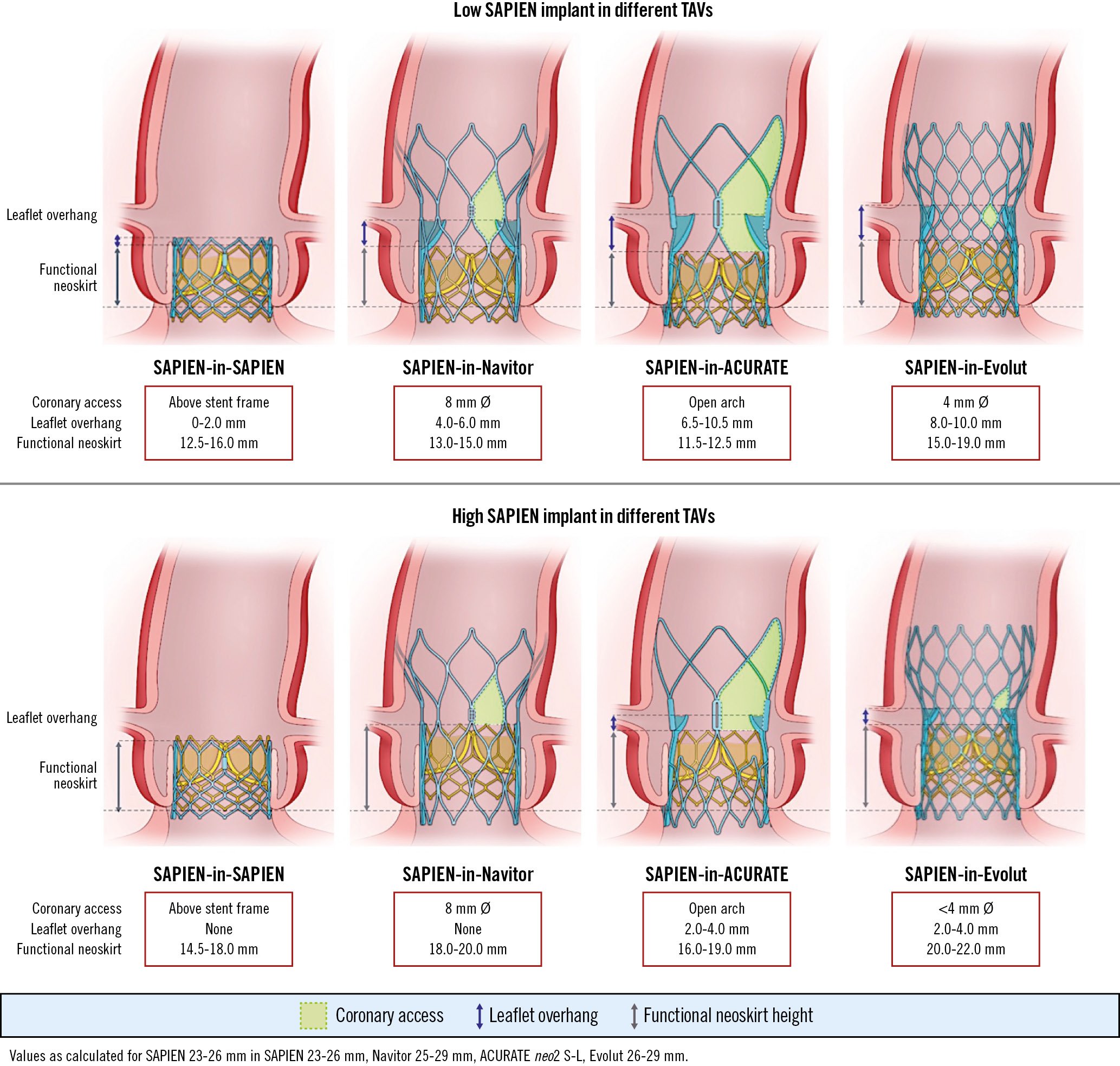
Figure 1. Impact of different TAV-in-TAV combinations and implant positions on redo-TAVI outcomes. The index TAVs are depicted at a nominal implant depth. The second balloon-expandable TAV can be implanted at different heights; this figure shows the recommended lowest versus highest SAPIEN position for redo-TAVI in different TAV platforms. Navitor (Abbott); ACURATE (Boston Scientific); Evolut (Medtronic); these aspects are the same for the older-generation TAVs of these respective devices. TAV(I): transcatheter aortic valve (implantation)
Conflict of interest statement
O. De Backer received institutional research grants from and has been a consultant for Abbott, Boston Scientific, and Medtronic. J. Sathananthan received research grants from and is a consultant for Edwards Lifesciences, Medtronic, and Boston Scientific. H. Danenberg is a proctor for Medtronic and Edwards Lifesciences. J. Webb is a consultant for Edwards Lifesciences. L. Sondergaard is Chief Medical Officer and Divisional VP for Medical Affairs at Abbott Structural Heart; and has received consultant fees and/or institutional research grants from Abbott, Boston Scientific, Medtronic, and SMT. U. Landes has no conflicts of interest to declare.