Abstract
Aims: Transcatheter aortic valve implantation (TAVI) is an emerging alternative to medical therapy reserved to a limited population with severe aortic stenosis. Quality-of-life (QoL) is a critical measure of effectiveness of TAVI in this patient population. In this prospective study, we sought to assess one year changes in QoL in patients who underwent TAVI.
Methods and results: From June 2007 to July 2010, 149 consecutive patients underwent TAVI using the 18 Fr CoreValve (Medtronic Inc, Minneapolis, MN, USA) or the Edwards SAPIEN XT heart valve (Edwards Lifescience, Irvine, CA, USA) at our institution. Of these, 143 patients with successful prosthesis implantation comprised the study population. The SF-12v2 Health-Survey questionnaire provides scales for physical (physical component summary [PCS]) and mental (mental component summary [MCS]) health. Among patients included in the present analysis, device success was obtained in 138 patients (96.5%). Mean preprocedural SF-12v2 scores showed an important upgrading after TAVI: PCS improved from 28.3 to 44.0 at five months and 42.4 at 12 months (p<0.001). MCS increased from 38.0 to 47.3 at five months and 48.2 at 12 months (p<0.001). Both the physical and mental score summaries at follow-up of these post-TAVI patients were not significantly different from the anticipated thresholds of the general Italian population over the age of 75 years. NYHA functional class improvement was reported in all patients.
Conclusions: Our results showed a marked mid-term improvement in functional status and physical and mental health in patients who underwent TAVI.
Introduction
Surgical aortic valve replacement (SAVR) is the gold standard for the treatment of severe symptomatic aortic stenosis (AS)1. In the last years, the introduction of transcatheter aortic valve implantation (TAVI) has expanded the therapeutic possibilities for successful treatment of AS. TAVI was first performed in humans in 20022 and has been subsequently used successfully in several thousands elderly patients with AS at high-risk for SAVR3-7. The recently published Placement of Aortic Transcatheter Valves (PARTNER) randomised trial Cohort B demonstrated that TAVI remarkably reduced the mortality, as compared with standard therapy in patients not suitable candidates for surgery8. In addition, The PARTNER Cohort A results showed that short and mid-term outcomes after TAVI compare favourably with SAVR9.
In the high-risk population that is offered this treatment at present, it is important to assess the impact of TAVI on patients’ physical and mental well-being and improvement in quality-of-life (QoL), in addition to traditional endpoints such as morbidity and mortality10-12. Although it has been demonstrated that TAVI improves the functional class and QoL in such patients at short-term follow-up10-12, there is a paucity of data on benefits in physical and mental well-being and QoL at longer follow-up.
The aim of this prospective, single centre study was to assess changes in the patient’s QoL one year after TAVI for severe AS.
Methods
Patient population
From June 2007 to July 2010, among all patients with severe symptomatic AS consecutively referred for TAVI by other institutions or independent cardiologists and screened to assess their eligibility for TAVI, those who actually had a high surgical risk or contraindications to SAVR were evaluated for TAVI.
Screening included a comprehensive clinical evaluation, trans-thoracic echocardiogram and, if necessary, transesophageal echocardiography, coronary angiography, aortic and iliofemoral and 64-multislice computed tomography. A multidisciplinary team including cardiologists, cardiothoracic surgeons, anaesthesiologists, geriatricians and interventional cardiologists who evaluated all available clinical and imaging data. A consensus decision was then arrived at to determine eligibility for TAVI13. The decision to perform TAVI was made in patients with severe symptomatic AS; contraindications to, or high risk for SAVR, life expectancy ≥1year, anatomy suitable for intervention and no need for coronary bypass surgery. Patients were eligible for QoL assessment if they were not affected by dementia and were able to read and write Italian.
TAVI procedure
All procedures were performed under local anaesthesia and analgesia under fluoroscopic guidance in a standard cardiac catheterisation laboratory with surgical backup by a dedicated team of experienced operators. General anaesthesia was employed when the trans-subclavian approach was used. Briefly, the stenotic valve was crossed retrogradely and predilated with an appropriately sized balloon. Next, the self-expanding CoreValve Revalving System (CRS) (Medtronic Inc, Minneapolis, MN, USA) device or the Edwards SAPIEN (ES) XT heart valve (Edwards Lifescience, Irvine, CA, USA) was positioned across the aortic annulus and deployed with aortic root angiography at every stage to ensure optimal deployment. Technical details of the transfemorall3,14 and trans-subclavian15 procedures have been detailed previously. Upon completion of the procedure, all patients were transferred to the intensive care unit for post-procedure monitoring and continued medical management16.
Quality-of-life and functional class assessment
Functional status was determined in all patients using the New York Heart Association (NYHA) functional class, whereas QoL was assessed with the Medical Outcomes Study (MOS) Short Form-12 version 2 (SF-12v2) tool. All the characteristics of this questionnaire and the scoring system have been previously described in detail9. Briefly, the SF-12v2 consists of 12 questions, grouped into eight multi-item domains, which measure functioning in different dimensions of subject health: physical functioning (PF), physical health related to age- and role-specific activities (“Role-Physical”) (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), personal feelings of performance in age- and role-specific activities (“Role-Emotional”) (RE), and mental health (MH). These items contribute to generate two scores (the mental component summary [MCS] and the physical component summary [PCS]) which were compared with those expected for the general population of a similar age. To minimise physicians’ or relatives’ influence, the research staff made sure that all patients were able to comprehend the questions and would be able to give appropriate answers.
The questionnaire was administered to patients during their first clinical evaluation within hospitalisation for the TAVI procedure, at 5-months, and again at 12-months after the procedure. On each occasion, the patients returned the questionnaires to the physician in a sealed envelope.
Definitions
Device success, cardiovascular death, periprocedural and spontaneous myocardial infarction, strokes, bleedings and vascular access site and access-related complications were defined according to the Valve Academic Research Consortium (VARC)17.
Statistical analysis
Continuous variables were presented as mean ±SD and compared with the use of the paired or unpaired t-test, as appropriate, in case of normal distribution, or the Wilcoxon or the Mann-Whitney, as appropriate, in case of non-normal distribution. The normality of the data was assessed with the Kolmogorov-Smirnov test. Categorical variables were presented as counts and percentages and compared with the use of Fisher’s exact or χ2 test, as appropriate. Changes in QoL parameters from baseline to 5-months and to 12-months follow-up were assessed using the ANOVA test with Bonferroni adjustment. A two-sided p-value of less than 0.05 was considered of statistical significance. All data were processed using the Statistical Package for Social Sciences, version 17 (SPSS, Chicago, IL, USA).
Results
Among 149 consecutive patients who underwent TAVI with self-expanding CRS and balloon-expandable ES devices, 143 with successful prosthesis implantation completed SF-12v2 at baseline and were enrolled in this study. Baseline demographic and clinical variables of these patients are presented in Table1. Mean age was 81.0±4.6 years and 59.4% of patients were female. All patients had severe symptomatic AS (mean aortic valve area [AVA] 0.59±0.19cm2). Overall, the population was at high surgical risk with a predicted mortality of 23.4±14.7% using the logistic EuroSCORE and 7.9±4.0% by the STS-mortality score. The majority of patients (N=92; 64.3%) were in NYHA functional class 3 or 4 before the procedure. Transfemoral access was used in 140 patients (97.9%); in three patients (2.1%) where the transfemoral approach was not feasible, a trans-subclavian access was used to implant aCRS device. The prostheses’ type and size are listed in the Table2.
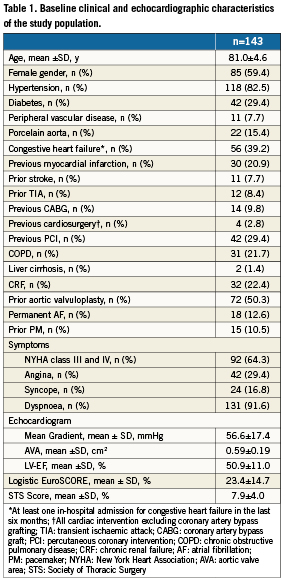
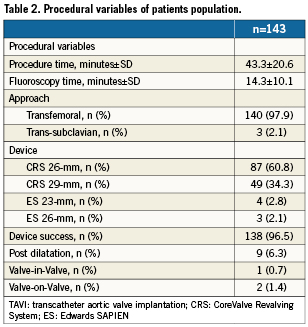
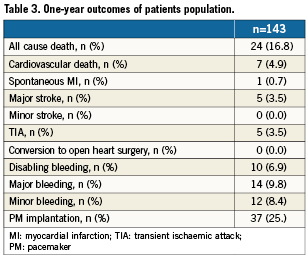
Among patients included in the present analysis, device success was obtained in 138 patients (96.5%). Prosthesis under-expansion causing haemodynamic instability was managed successfully in nine cases (6.3%) with post-implant balloon dilatation; prosthesis (CRS) migration occurred in two cases and was successfully managed with implantation of two (in-series) CRS prostheses18; one case of sub-optimal CRS positioning (too-high) was managed with the “Valve-in-Valve” technique19. The acute procedural success was confirmed by invasive measurement of the transvalvular peak-to-peak gradient and was <5mmHg in all patients. This was confirmed by the echocardiographic results, showing a significant reduction in mean aortic valve gradient (from 56.6±17.4mmHg to 11±5mmHg; p<0.001). During hospitalisation, all-cause death occurred in nine patients (6.3%), among those, five (3.5%) were cardiovascular death. Major stroke occurred in four patients (2.8%), there was no incidences of minor stroke. TIA occurred in five patients (3.5%), Disabling, major and minor bleedings occurred in 10 (7.0%), 14 (9.8%) and 12 (8.4%) patients, respectively, whereas major and minor vascular complications occurred in 12 (8.4%) and eight (5.6%) patients, respectively. New, definitive pacemaker implantation was required in 35 patients (24.5%). Cumulative clinical outcomes beyond hospital discharge up to one-year at follow-up across the study population are reported in Table3.
Postoperative changes in quality-of-life and functional status
In the following paragraph, the presentation style for SF-12v2 parameter results is xx/xx/xx for baseline/5-month/12-month follow-up. Pvalues indicates differences between baseline and 12-month follow-up.
Scores of perceived quality-of-life both at baseline and at follow-up are schematised in Figure1. Overall, patients experienced a marked and sustained improvement with regard to physical functioning (27.0/41.1/40.8; p<0.001), role-physical (28.6/41.6/41.3: p<0.001), bodily pain (37.5/49.0/48.0; p<0.001), general health (24.0/43.3/43.2; p<0.001), vitality (41.0/50.9/49.6; p<0.001), social functioning (35.2/44.5/45.0; p<0.001), role-emotional (29.5/43.6/ 42.7; p<0.001), and mental health scores (37.8/48.3/48.6; p<0.001). Mean pre-procedural SF-12v2 scores showed a severe impairment of perceived quality-of-life compared with the general Italian population >75 years, both for physical (baseline-PCS 28.3) and mental scores (baseline-MCS 38.0) (Figure2). After five months, an improvement in both scores (PCS 44.0-MCS 47.3; p<0.001) was observed. Interestingly, both the physical and the mental score summaries at five months of these post-TAVI patients were not appreciably different from the anticipated thresholds of the general Italian population over the age of 75 years. These remarkable results were maintained at 12-month follow-up (PCS 42.4-MCS 48.2; p<0.001 for both PCS and MCS when compared with baseline; p=0.673 for PCS and p=0.872 for MCS when compared with 5-month follow-up) (Figure2).
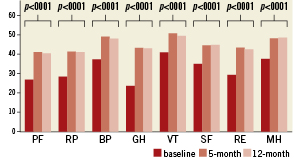
Figure 1. Short Form 12v2-Item Health Survey scores of all eight health components before five months and 12 months after TAVI. PF (Physical Functioning): limitations in lifting, climbing, bending, kneeling, walking, or running; RP (Role-Physical): degree of physical health to perform activities typical for the specific age and social responsibility, such as a job, community activities, and volunteer work; BP (Bodily Pain): intensity and duration of bodily pain and limitations in activities due to pain; GH (General Health): beliefs and evaluations of overall health; VT (Vitality): feelings of energy, pep, fatigue, and tiredness; SF (Social Functioning): ability to develop, maintain, and nurture mature social relationships (including family, friends, and spouse); RE (Role-Emotional): personal feelings about job performance, work, or other activities; MH (Mental Health): emotional, cognitive, and intellectual status.
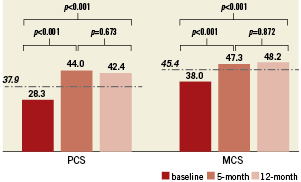
Figure 2. Results of PCS (physical component summary) and MCS (mental component summary) scores before, at 5 months and at 12 months after TAVI compared with general Italian population. Data obtained show that patients have a significant improvement in physical and mental status after TAVI (P<0.001). * The dotted line indicates the values of PCS and MCS scores in a representative sample of Italian population of 75-year-olds (5,283 adults).
At 5-month follow-up, among the 143 patients included the study, PCS score increased in 106 (74.1%), worsened in nine (6.3%) and remained unchanged in seven (4.9%). On the other hand, MCS score increased in 85 patients (59.4%), worsened in 12 (8.4%) and remained unchanged in 25 (17.5%). At 12-month follow-up PCS score increased in 111 patients (77.6%) and remained unchanged in six patients (4.2%) when compared with the baseline, while MCS score increased in 57 patients (48.7%), but worsened and remained unchanged in 25 (21.4%) and 35 patients (29.9%), respectively (Figure3).
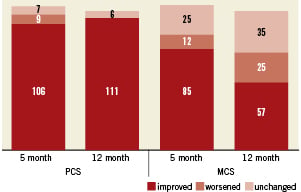
Figure 3. Changes in PCS and MCS scores among study population during follow-up intervals.
NYHA class 3/4 at 5-month was virtually absent in the study population (six patients in NYHA class 3, 4.2%; p<0.001 compared with baseline). This benefit was sustained at 12-month (seven patients in NYHA class 3, 4.9%; p<0.001 when compared with baseline, and p=0.752 when compared with 5-month follow-up) (Figure4). Those patients who did not show a significant increase in MCS did not NYHA class3.
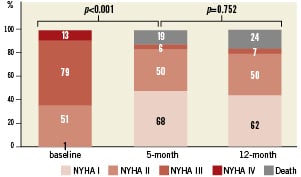
Figure 4. NYHA functional class baseline, at 5- and 12-months follow-up of the study population.
Patients not included in the study population
Six patients (4.0%) were excluded from this analysis. In detail, two patients were excluded due to CRS implantation failure (prosthesis not released) and four patients did not satisfy the inclusion criteria, because two had dementia and two were unable to complete the questionnaire.
Discussion
The main finding of this study is that TAVI in elderly patients with severe AS and high risk for cardiac surgery is followed by improvements in QoL that are sustained at one year as assessed with the well-validated SF-12v2. The magnitude of this improvement 12months after the procedure is slightly lower when referring to the mental component of QoL perception. The purpose of this prospective analysis was to demonstrate that the short-term improvement in the personal perceived QoL of the patients after TAVI, described previously by our group10 as well as other authors11,12, was maintained at one year follow-up.
Recently, results from The PARTNER randomised trial Cohort B and Cohort A have led percutaneous transfemoral TAVI to assume the position of the best therapy in high risk AS patients declined surgery8,9. Nevertheless, the population which currently undergoes this procedure makes the assessment QoL parameters fundamentally important in addition to the usual evaluations of TAVI results. In fact, in elderly and frail patients, comfort in daily life appears to be equally important to the improvement in life expectancy and the survival rate. Several surgical series have already demonstrated the benefit of conventional heart valve replacement/repair in terms of QoL20-23.
In accordance with our prior published results10, pre-procedural SF-12v2 scores of our patient cohort demonstrated a severe impairment in perceived QoL, compared with the general Italian population over the age of 75 years. A sub-analysis of eight health-scales derived by the Sf-12v2, indicated markedly low scores for physical functioning both for mental and physical scores. In this analysis, all mean values of these scales improved at 5-month and maintained at one year. These results are consistent with and extend those reported by Bekeredjian and colleagues12, where a population of 80 octogenarians who underwent TAVI with the CRS device experienced asignificant improvement in all the eight health components (assessed by the Short Form 36-Item Health Survey), six months after the procedure. Another study by Krane and colleagues11, which investigated QoL changes at three-months follow-up, showed a remarkable increase for parameters describing the physical health and, accordingly, a significantly increased physical health summarised score. However, contrary to the results described by Bekeredjian12, this study did not demonstrate an improvement for mental health parameters, except for the vitality score. As highlighted by the authors, these findings might be explained by the fact that follow-up period of three months was probably too short to translate the early physical recovery into an improvement of the mental health scores. Interestingly, our findings are consistent with those recently reported in a subanalysis of The PARTNER Cohort A randomised trial24. The PARTNER investigators, using the Kansas City Cardiomyopathy Questionnaire, the SF-12 Health Status Survey and the EQ-5D, showed that both study arms (TAVI patients and SAVR patients) experienced an improvement of QoL at 1-year, but the degree of improvement was greater among the patients treated with TAVI.
The mid-term benefit in both PCS and MCS scores appears to be important. These results add meaningfully to those previously reported by our group at an earlier follow-up10, where an improvement in both scores was observed in 30 consecutive patients at five months follow-up (PCS improved from 28.5 to 41.3 and MCS improved from 37.8 to 48.3; p<0.001). The present study tends to underline the proof of sustained durability in QoL up to one year after TAVI. None of the patients in this study experienced a worsening of QoL after the procedure as measured with the PCS score, in contrast, the MCS score remained unchanged or worsened slightly in a half of patients. This finding might be explained by the presence of several comorbidities and other important conditions frequent in the elderly (osteoporosis or loss of independence), which can affect patients’ mental well-being over time.
Finally, symptom relief evaluated with NYHA functional class was observed in the majority of patients included in this series at both follow-up intervals. Interestingly, all patients who did not show an increase in MCS after TAVI at 1-year were in NYHA classI or II.
We chose to investigate the general status of patients with the Short Form-12 version 2 questionnaire, which is easy to use, understand and can be completed by most participants in less than a third of the usual time needed to complete the SF-3625,26 reducing respondent burden and improving response rates. These characteristics were important key features for its application to a population of elderly patients. The 98.3% response rate for each survey reported in this study, corroborates this understanding. Moreover, it was observed that SF-12v2 yields results that are comparable to those that would be obtained with the original SF-3627.
Study limitations
The main limitation of this study is its non-randomised nature, as well as the single-site data collection. Also, the relatively small sample size might be an important limitation, even if the study represents one of the largest experiences of QoL assessment after TAVI ever reported. However, we believe that the prospective enrolment of all consecutive patients treated with TAVI at our centre lends significance to these results.
Conclusions
The results from this study show that both high-surgical-risk and elderly patients affected by severe symptomatic AS experienced an improvement in QoL after TAVI. This procedure is able to preserve a high degree of independence at 1-year follow-up. Further studies are needed to confirm these results and to assess their longer-term durability.
Acknowledgement
The authors thank the ETNA foundation for its support.
Conflict of interest statement
Gian Paolo Ussia, is a proctor physician for Medtronic Inc.; all other authors have no conflicts of interests to declare.