Abstract
Aims: The aim of the study was to investigate the changes in quality of life (QoL) following transcatheter aortic valve implantation (TAVI) up to two years’ follow-up.
Methods and results: One hundred consecutive patients (46 females, mean age 79.7±6.1 years) with at least two years’ follow-up who underwent TAVI in our institution, between November 2007 and September 2009, were enrolled in this study. Peak and mean aortic gradients were 87.8±25.8 mmHg and 53.3±15.4 mmHg, respectively. Mean log EuroSCORE was 27.9±15.9. Patients had multiple comorbidities. All patients underwent a standardised prospective screening pathway, including QoL evaluation with the 36-item short-form health survey (SF-36v2®) and the Minnesota Living with Heart Failure Questionnaires (MLHFQ). The scores obtained preoperatively were compared with those obtained at two years’ follow-up. An Edwards SAPIEN valve (Edwards Lifesciences, Irvine, CA, USA) was implanted in 67 patients (55 transfemoral and 12 transapical) and a CoreValve (Medtronic, Inc., Minneapolis, MN, USA) was implanted in 33 patients (26 transfemoral and seven transaxillary). Thirty-day mortality was 4%. Actuarial survival was 80.6±4.1%, 72.6±4.7% and 63.2±6.3% at one, two and three years, respectively. Mean SF36-physical improved from 31.9±8.8 to 51.5±9.5 (p<0.0001) and SF36-mental improved from 44.7±11.6 to 49.5±8.6 (p=0.0002). Mean MLHFQ decreased from 41.5±14.5 to 15.9±13.7 (p<0.0001). QoL score changes were not influenced by age or comorbidities.
Conclusions: TAVI in high-risk surgical candidates is associated with favourable short and long-term survival and with improvement of QoL up to two years after the procedure.
Introduction
Degenerative aortic valve disease is currently the most common valvular disease requiring hospitalisation in Western countries, with a prevalence of 4.6% in adults over 75 years1. This subset of the population is continually growing and imposes a challenge for health care resources. When symptoms of aortic valve disease are present, life expectancy is reduced and quality of life (QoL) is suboptimal. Surgical aortic valve replacement (SAVR) is the standard of care for patients with severe symptomatic aortic stenosis (AS), providing relief of symptoms as well as improving survival and QoL2,3. SAVR has also been shown to improve QoL in the elderly subpopulation4,5. Unfortunately, SAVR is frequently denied in elderly patients, because the prognostic benefit is underestimated, while perioperative morbidity and mortality are overestimated6. Transcatheter aortic valve implantation (TAVI) provides an alternative in this subset of inoperable or high-risk surgical patients7,8.Since advanced age and comorbidities have a strong impact on the QoL of patients, the role of TAVI in patients with very advanced clinical status has been questioned and not yet fully elucidated at mid and long-term follow-up. The aim of this study was to evaluate the changes of QoL in a series of consecutive high-surgical-risk patients two years after TAVI for severe symptomatic AS.
Methods
PATIENTS
From November 2007 to July 2009, 100 consecutive patients underwent TAVI at our institution. For the aim of the present study, we chose this study period in order to have a minimum follow-up of two years in all patients.
All the patients included presented the criteria for intervention of the European Society of Cardiology guidelines for the management of valvular heart disease3. Inclusion criteria, according to the EACTS/ESC consensus position statement for TAVI procedures9, were: severe symptomatic AS, aortic valve annulus diameter from 19 mm to 27 mm and contraindication to conventional surgery because of comorbidities or anatomical/technical issues (such as porcelain aorta or prior coronary artery bypass grafting with open grafts). Informed written consent was obtained from all the patients.
All patients were evaluated by a dedicated multidisciplinary valve team (composed of cardiac surgeons, interventional cardiologists, anaesthesiologists and radiologists expert in cardiovascular imaging). Preprocedural assessment included transthoracic echocardiography (TTE), carotid ultrasonography, spirometry and evaluation of the peripheral access sites, aortic anatomy, valve annulus size and coronary anatomy by CT angiography and/or arterial angiography.
Clinical decision-making was based on a multimodality screening process including evaluation of surgical risk by EuroSCORE and STS algorithm (http://www.euroscore.org/ and http://209.220.160.181/STSWebRiskCalc261/). High surgical risk was defined as a logistic EuroSCORE ≥20% and/or STS score ≥10%. Adjunctive risk criteria were advanced liver cirrhosis, severe neurological impairment and frailty, according to physician judgement. In an attempt to increase objectivity, patient status was also assessed with additional tests including Mini Nutritional Assessment (MNA)10, Charlson Comorbidity index (CCI)11 and six-minute walk test (6-MWT)12. Cognitive disorders were assessed by means of the Mini Mental State test13. Figure 1 shows the flow of the patients.
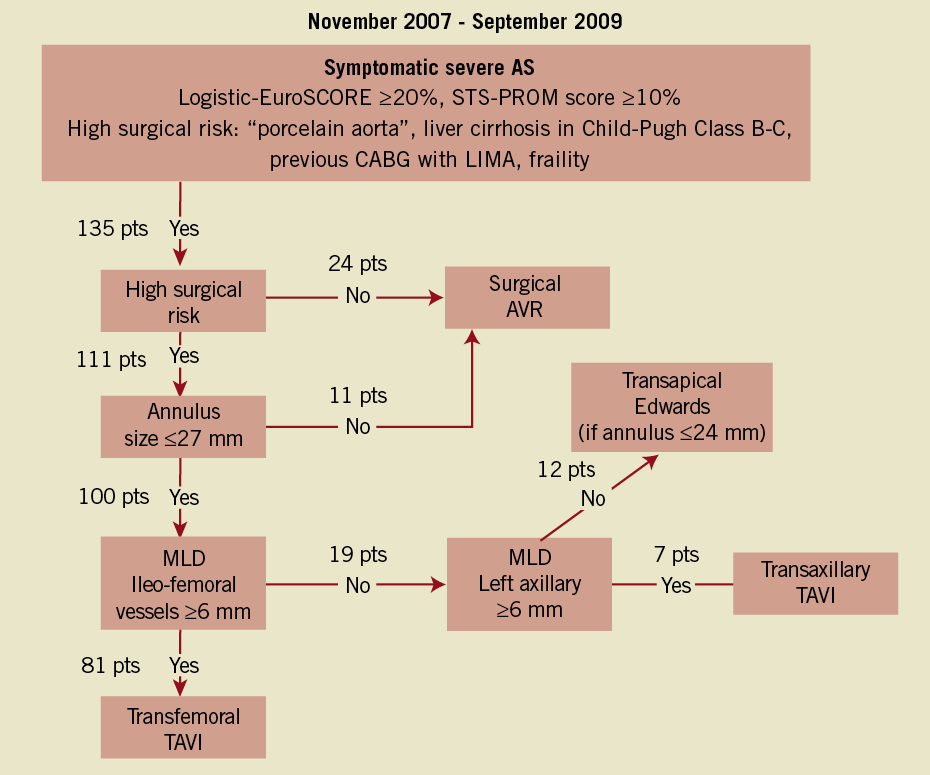
Figure 1. Clinical flow of the patients in our institution.
The QoL of the patients was quantified by the Minnesota Living with Heart Failure Questionnaire (MLHFQ)14 and by the 36-item short-form health survey (SF-36v2®)15. The MLHFQ is a 21-item disease-target measure, which is specifically designed to assess the effects of heart failure and its treatment on QoL. The SF-36 is a multipurpose, short-form health survey with 36 questions and represents one of the most used instruments to assess health-related QoL. The final result is composed of two metascores: the physical component summary (SF-36 physical, which correlates with the physical functioning and the limitations to physical health) and the mental component summary (SF-36 mental, which correlates with psychological distress and wellbeing). Both questionnaires were given to all patients at their first clinical evaluation before the procedure and again by outpatient visit following the procedure at regular intervals every six months and at the last available follow-up. All the patients included in this study were able to comprehend the questions. All the preoperative and follow-up data, which have been defined according to the Valve Academic Research Consortium (VARC) criteria16, have been entered prospectively in a dedicated database and then harvested retrospectively for the aim of this study. The QoL scores obtained preoperatively were then compared to those obtained at the last follow-up. SF-36 values observed in a general Italian elderly population (age 75-84 years) were used as cut-off to define QoL restoration after the procedure (47.5 for SF-36 physical domain and 49.2 for SF-36 mental domain)17.
PROCEDURE
All the TAVI procedures were performed in the catheterisation laboratory, under fluoroscopic guidance. General anaesthesia or deep sedation was employed according to the anaesthesiologist’s judgement.
Two devices were used during the study period: the SAPIEN valve (Edwards Lifesciences, Irvine, CA, USA) and the third-generation CoreValve Revalving System (Medtronic, Inc., Minneapolis, MN, USA). The SAPIEN valve consists of three bovine pericardial leaflets mounted within a balloon-expandable stainless-steel stent. Prosthesis sizes included 23 mm and 26 mm, requiring either a 22 Fr or 24 Fr (transfemoral) or a 26 Fr (transapical) sheath for delivery. The retrograde transfemoral approach was preferred whenever it was possible. In patients with small or diseased iliofemoral arteries, TAVI was performed by the transapical antegrade approach, through a left anterolateral mini-thoracotomy. For the transapical approach, femoral access and cardiopulmonary bypass were always on stand-by, to allow for a rapid surgical conversion in case of complications.
Before deployment of the SAPIEN valve, a balloon aortic valvuloplasty (BAV) was performed using standard techniques under rapid pacing (ranging from 160 to 220 beat/min), in order to predilate the stenotic valve.
The CoreValve Revalving System consists of three porcine pericardial leaflets mounted in a self-expanding nitinol frame (26 and 29 mm sizes), implanted with an 18 Fr introducer sheath compatible system. The CoreValve was usually implanted retrogradely from the femoral artery with the standard technique16. In a minority of patients with inappropriate peripheral access from the groin, a transaxillary approach was used.
In patients undergoing transfemoral implantation, a totally percutaneous procedure adopting preclosure with one or two 10 Fr Prostar XL closure devices (Abbott Vascular, Abbott Park, IL, USA) was performed in most patients.
After the procedure, the patients were transferred to the intensive care unit and monitored. Before discharge, a TTE, ECG and chest x-ray were routinely performed in all patients. Clinical and echocardiographic follow-up was scheduled at our out-patient unit at 30 days, six months, 12 months and then yearly following the intervention.
STATISTICAL ANALYSIS
Statistical analysis has been conducted using the JMP 8.0 software (SAS Institute Inc., Cary, NC, USA). Continuous variables are presented as mean±SD and categorical variables are expressed as percentages. Univariable comparisons have been performed with either the paired t-test and ANOVA for parametric, or the Wilcoxon test for non-parametric continuous data, and with the chi-square test for categorical data. Survival has been reported using the Kaplan-Meier method. A p-value < 0.05 was considered statistically significant, and all reported p-values are two-sided.
Univariate analysis of predictors of QoL restoration at two years was performed with logistic regression.
Results
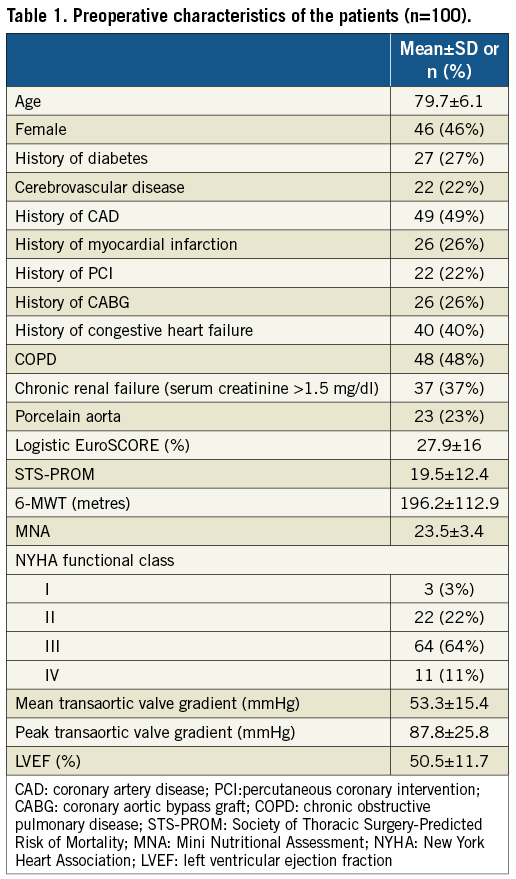
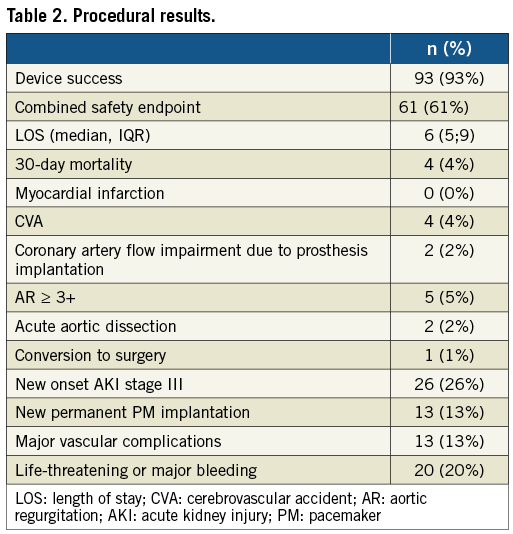
A SAPIEN valve was implanted in 67/100 patients: in 55 patients by transfemoral access, while in 12 patients a transapical approach was preferred. In 33/100 patients, a CoreValve prosthesis was used (26 transfemoral and 7 transaxillary). Baseline characteristics of the patients are summarised in Table 1. Device success was achieved in 93% of the patients. In one patient, an acute type A aortic dissection requiring emergency conversion to surgery occurred. Thirty-day mortality was 4% (four patients died: two from cardio circulatory arrest, one from haemorrhagic shock due to a retroperitoneal haematoma, one from cerebral bleeding). Major vascular complications, defined according to the VARC criteria16 occurred in 13/100 patients, including: two cases of acute aortic dissection, seven iliac or femoral ruptures treated with unplanned surgical or endovascular procedures and/or requiring blood transfusion of ≥4 units, one avulsion of external iliac artery, two femoral artery thromboses, one left ventricular apex bleeding in transapical approach. The incidence of life-threatening bleeding was 20%. The incidence of new onset heart block requiring permanent pacemaker was 13% (13 patients). Combined safety endpoint according to the VARC criteria was reached in 61%. The median length of hospital stay was six days (IQR 5-9 days). Table 2 summarises the periprocedural results. Mean preprocedural SF-36 and MLHFQ showed a severe impairment of the QoL in almost all patients (average SF-36 physical 31.9±8.8; average SF-36 mental 44.7±11.6; average MLHFQ 41.5±14.5).
Follow-up was 100% complete (median 24.9 months IQR 20.4-32.9 months - range 0.1-44 months). All the survivors had at least two years of clinical and instrumental follow-up. Actuarial survival was 80.6±4.1%, 72.6±4.7% and 63.2±6.3% at one, two and three years, respectively (Figure 2). No significant differences were observed in terms of survival depending on the different approaches (transfemoral, transapical or transaxillary, p=0.2) or according to the type of valve (SAPIEN vs. CoreValve; p=0.7).
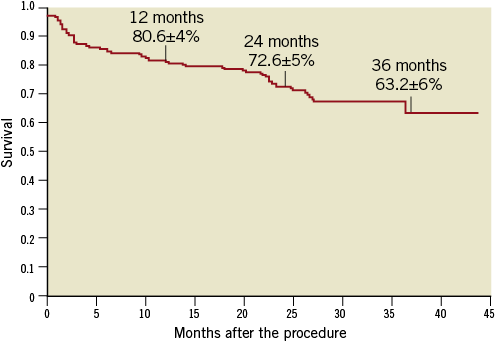
Figure 2. Overall survival at follow-up.
At one year, the mean SF36-physical improved from 31.9±8.8 to 50.2±8.7 (p<0.0001) and SF36-mental improved from 44.7±11.6 to 50.1±6.9 (p=0.0002); mean MLHFQ decreased from 41.5±14.5 to 15.9±13.3 (p<0.0001). At two years, mean SF-36-physical was 51.5±9.5 (p<0.0001), SF36-mental was 49.5±8.6 (p=0.02) and mean MLHFQ was 15.9±13.7 (p<0.0001) with a significant improvement as compared to preoperative values (Figure 3).
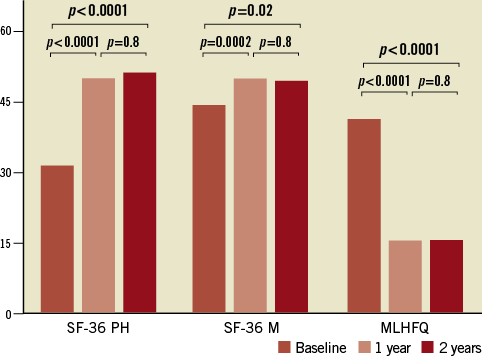
Figure 3. SF-36 and MLHFQ indices at baseline, one year and two years after TAVI . PH: physical; M: mental
The improvement of the QoL indices was observed in all subsets of patients, independently from comorbidities and age. The perceived QoL according to the SF-36 mental domain improvement was not significant in patients with history of diabetes, history of cerebrovascular disease, history of coronary artery disease, history of acute myocardial infarction, previous PCI and CABG, or chronic renal failure (Table 3).
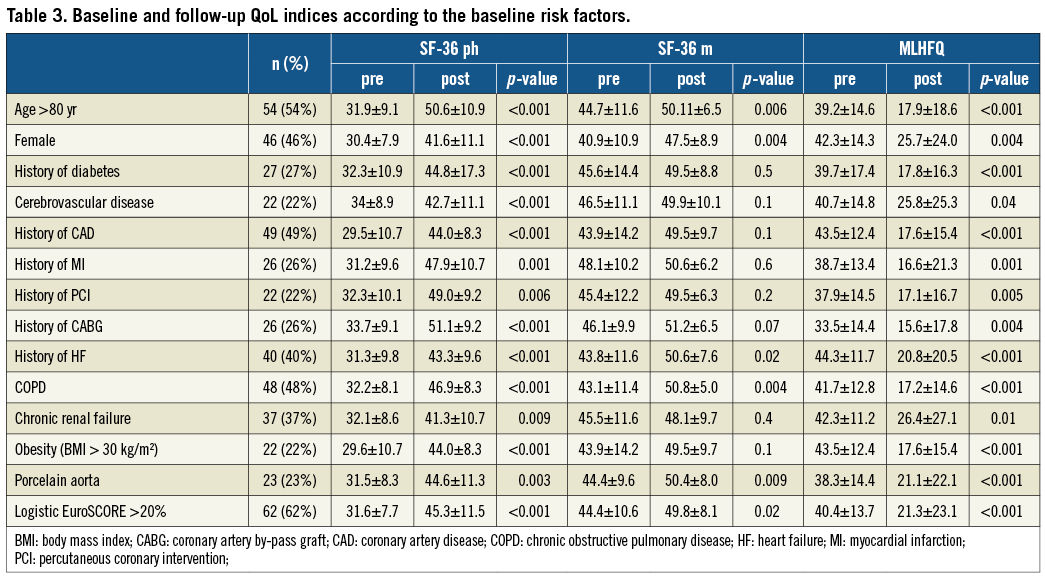
Patients with preoperative chronic renal failure (defined as a serum creatinine >2.0 mg/dl) and obesity (defined as a BMI >30 kg/m2), in spite of a significant improvement of QoL, had a worse SF-36 physical score at follow-up if compared to patients without these comorbidities (p=0.0009 and p=0.03 respectively).
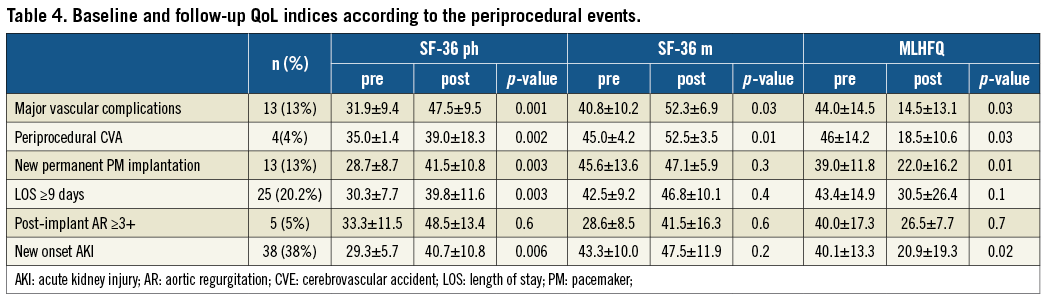
Patients treated by transapical approach had a significantly higher MLHFQ score than those treated by the transfemoral and transaxillary approaches (respectively 31.5±32.3; 13.8±8.5 and 19.6±11.7; p=0.0006). No difference was observed among the three groups as far as the SF-36 was concerned.
Patients who suffered from periprocedural complications also experienced a significant improvement in their SF-36 physical domain scores, with the exception of those who had significant residual aortic regurgitation after TAVI (Table 4). The SF-36 mental domain index did not change significantly in all patients with a complicated periprocedural course, with the exception of patients with vascular access issues. The improvement of MLHF scores was not present in patients with prolonged LOS (longer than eight days) and in those with residual moderately severe and severe AR.
At two years, QoL restoration was achieved in 71.4% of the survivors for SF-36 physical domain and in 61.8% for SF-36 mental domain. No predictors of QoL restoration at two years were identified by univariate analysis.
Discussion
Our data show that most patients who underwent TAVI benefit from an improved QoL after the procedure, which is maintained up to two years after the procedure. In our experience, improvement in QoL is also observed in patients with more critical preoperative status. These findings strongly support the indication for TAVI in those patients who are denied surgery because of advanced age or multiple comorbidities.
As recently demonstrated by the PARTNER A and B cohorts7,8 and by several other reports18-22, this study confirms that TAVI in inoperable and high-risk surgical candidates is associated with excellent short and medium-term results in terms of morbidity and mortality. However, reporting morbidity and mortality provides only partial information about the patients’ wellbeing after the treatment and the effect on overall health care resource expenses related to a procedure. Several studies support the indication for surgical AVR in elderly people with preserved cognitive function and good life expectancy, since QoL improvement/preservation may be a more appropriate goal for cardiac surgery in advanced age compared to increasing life span4,5,23,24.
Perceived QoL in the elderly is the result of multiple factors, including cardiac and non-cardiac comorbidities. Most of these factors are not related to AS; however, octogenarians submitted to SAVR have an improvement in QoL, symptoms and physical ability comparable with younger patients4,5.
QoL improvement in high-risk patients one year following TAVI have recently been reported by different authors. The results of the PARTNER B cohort have demonstrated that among inoperable patients with severe aortic stenosis, compared with standard care (medical treatment and balloon aortic valvuloplasty), TAVI resulted in significant improvements in health-related QoL that were maintained for at least one year25. Ussia et al reported an improvement in physical and mental health one year after the procedure in a series of 149 consecutive patients who underwent transfemoral CoreValve implantation26. In this study, the QoL was assessed by the SF-12v2® questionnaire and a striking improvement was observed in both physical and mental scores.
The aim of our study was to investigate changes in QoL in a large series of consecutive patients submitted to TAVI, using all the conventional approaches (transfemoral, transapical and transaxillary) and both percutaneous aortic valve prostheses (SAPIEN and CoreValve), and who have been followed rigorously for up to two years after the procedure.
Because of the evident impact of many extra-cardiac factors on the QoL of the elderly patients in our study, we utilised two different instruments to estimate the health-related QoL: a generic profile measure such as the SF-36v2® questionnaire (that includes a global evaluation of physical functioning, role limitations due to physical problems, bodily pain, general health perceptions, energy/vitality, social functioning, role limitations due to emotional problems, mental emotional distress and change in perceived health), and a disease-target measure such as the MLHFQ (specifically designed to assess the effects of heart failure and its treatment on QoL).
The SF-36 has previously been used in a cardiac patient population, as well as in elderly patients after AVR5. In our study, preprocedural SF-36 physical and mental and MLHFQ showed an important impairment in perceived QoL in all patients, if compared with the data from the elderly Italian population27. All the investigated scores improved following the procedure. The major improvement in QoL was observed in the first year after the procedure, while from year one to year two QoL was stable among the patients.
In our series, the comorbidities mostly related to a worse level of QoL were chronic renal failure and morbid obesity, probably because of the physical limitations that are involved in these conditions. Procedural issues have limited impact on longer-term QoL and the improvement in QoL is independent of the type of prosthesis implanted. We found that patients who underwent transapical access had higher MLHFQ scores at follow-up, but this was potentially influenced by a selection bias since the transapical approach at our institution has been considered the last technical option after any other approach has been found inappropriate.
Also, we found that patients who had residual moderately severe to severe AR (AR> 2+) after TAVI appeared not to have a significant improvement in QoL indices at follow-up. Although this raises an intriguing issue, the number of patients in this study with such a complication is very small (n=5) and thus further evaluation is warranted before any conclusion can be undertaken in this regard.
Limitations of the study
The study is based on single institution data collection. A low number of patients have been treated with different devices and the number of patients in the subgroups is small.
The absence of a control group does not allow comparison with SAVR and medical therapy. Another important limitation is that in the study period only the SAPIEN device was available, while the SAPIEN XT device was not available.
In conclusion, TAVI in high-risk surgical candidates is associated with favourable short and long-term survival and with improvement of QoL up to two years after the procedure.
The improvement of QoL has been demonstrated using both a generic test such as the SF-36v2® questionnaire as well as a disease-target test such as the MLHFQ. Although all patients treated have an improvement in perceived QoL, an important burden of extra-cardiac comorbidities (especially chronic renal failure and obesity) could result in a suboptimal level of QoL following the treatment of AS.
Conflict of interest statement
The authors have no conflicts of interest to declare.

