Abstract
Aims: Transcatheter aortic valve implantation (TAVI) has emerged as a treatment alternative to surgical aortic valve replacement in elderly high-risk patients with symptomatic severe aortic stenosis. In this patient population, rapid improvement or restoration of quality of life (QoL) is at least as important as improved clinical outcomes. The purpose of the present study was to assess changes in QoL in response to TAVI.
Methods and results: Between August 2007 and August 2010, 62 patients (39% females, age 83±5years) underwent TAVI and were included in this QoL study. QoL was impaired at baseline and improved in all components of physical and mental health at nine months of follow-up: physical functioning (37.0 to 59.0, p<0.0001), physical role functioning (18.3 to 49.1, p<0.0001), general health (55.9 to 64.9, p=0.001), vitality (40.7 to 51.3, p<0.001), social functioning (67.4 to 76.8, p=0.049), emotional functioning (52.0 to 75.8, p<0.001) and mental health (66.6 to 75.8, p=0.05). The subscale bodily pain (60.7 to 70.4, p=0.058) showed a strong trend to improvement, but failed to reach statistical significance. Besides changes in health-related QoL, TAVI significantly improved symptoms (NYHA class 2.6±0.8 to 1.4±0.6, p<0.0001).
Conclusions: TAVI leads to rapid and sustained restoration of all aspects of mental and physical health and effectively alleviates symptoms.
Introduction
Transcatheter aortic valve implantation (TAVI) is a less invasive treatment alternative to surgical aortic valve replacement in elderly high-risk patients with symptomatic severe aortic stenosis. TAVI improves survival compared to medical treatment among patients considered not suitable candidates for surgery1 and is non-inferior to surgical aortic valve replacement in terms of survival among selected high-risk patients2. Apart from the achievement of favourable clinical results in terms of major cardiovascular and cerebrovascular events3-7, TAVI rapidly improves symptoms such as dyspnoea, angina and fatigue, and therefore impacts on quality of life (QoL) and physical capacity8. QoL, particularly in a patient population with limited life expectancy, is an important instrument in assessing patient-specific outcomes of therapeutic interventions. Measures of morbidity and mortality are not able to elucidate life-specific information on physical, emotional and mental well-being but can be supplemented with the patients’ perception of recovery after the intervention.
Although elderly patients with severe aortic stenosis constitute a challenging patient population with frequent comorbidities and overall reduced functional reserve, substantial improvement in physical as well as mental components of health-related QoL has been observed after surgical aortic valve replacement9,10 up to five years after the operation. Compared to conventional surgery, TAVI, due to its minimal invasive character, results in faster recovery and allows for early ambulation. We aimed to assess the improvement of QoL after transfemoral TAVI using a detailed, prospective evaluation with the SF-36 questionnaire before and nine months after intervention.
Methods
PATIENT POPULATION
Between August 2007 and August 2010, 235 consecutive patients with severe aortic valve stenosis at increased risk underwent TAVI at a single institution. Figure 1 summarises the patient flow. Patients undergoing TAVI via transapical (n=53) or transsubclavian access (n=4), and patients who died prior to valve implantation (n=2) were excluded, leaving a total of 176 patients undergoing transfemoral TAVI. Patients were considered to be eligible, whenever they were able to manage independently their everyday life and its necessities, in the absence of dementia at the time of inclusion, showed a willingness to participate actively in the follow-up assessment and were able to complete the German version of the SF-36 questionnaire. Patients were excluded from the study in case of urgent TAVI, an access route other than the femoral access (transapical and subclavian) and those not fluent in German. Applying these criteria, 62 patients were eligible and agreed to participate in this prospective and serial evaluation of quality of life. All patients underwent comprehensive evaluation of feasibility of the procedure and indication prior to TAVI using a standardised protocol including left and right heart catheterisation, aortography, transthoracic (TTE) and transoesophageal echocardiography (TOE) and CT angiography of the chest, abdomen and pelvis prior to the procedure11. Clinical risk assessment was performed with the linear and logistic EuroSCORE and STS Score and patients underwent subspecialty evaluation for complementary risk assessment and treatment recommendation. An interdisciplinary team of interventional cardiologists and cardiac surgeons reviewed the cases and agreed upon subsequent treatment allocation12. The local medical ethics committee approved the study, and all patients signed written, informed consent. The authors are solely responsible for the design and conduct of this study, for all study analyses, the drafting and editing of the paper and its final contents.
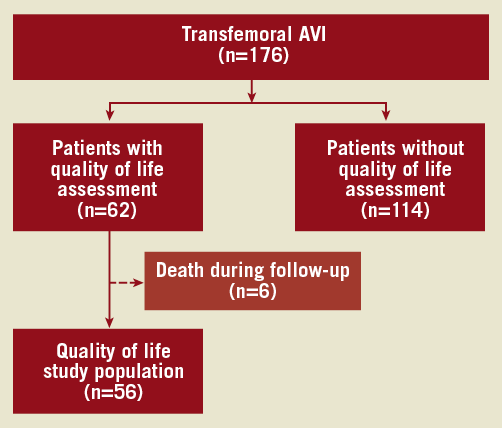
Figure 1. Flow of patients included in the present study.
PROCEDURE
Vascular access was obtained by puncture of the common femoral artery under fluoroscopic guidance. After insertion of the delivery sheath, TAVI was performed using either the Medtronic CoreValve® (Medtronic, Inc., Minneapolis, MN, USA) or the Edwards SAPIEN Transcatheter Heart Valve (Edwards Lifesciences, Irvine, CA, USA) as previously described13.
ENDPOINT DEFINITIONS
Clinical adverse events were adjudicated by a team of interventional cardiologists and cardiac surgeons according to the VARC endpoint definitions as reported elsewhere14. Major adverse cerebro-cardiovascular events (MACCE) were defined as death, myocardial infarction or major stroke.
QUALITY OF LIFE ASSESSMENT
QoL was assessed with the validated German version of the Medical Outcomes Trust Short Form 36 - Item Health Survey (SF-36) at baseline and at 9 months after TAVI. QoL assessment with the SF-36 health questionnaire is the most widely used generic health status instrument and generates a disease-independent assessment on health-related quality of life even in a geriatric patient population15. The 36 short questions reflect QoL in eight different domains: physical functioning (ten items), role limitation due to physical health problems (four items), bodily pain (two items), general health (five items), vitality (four items), social functioning (two items), role limitations due to emotional problems (three items), mental health related to psychological distress and well-being (five items) and one item including a self-evaluation of change in health during the past year. These components were summarised in two metascores (Physical Component Summary [PCS], Mental Component Summary [MCS]) representing the overall physical and mental function. The individual items generate a score for each dimension ranging from 0 to 100, with a higher score indicating a better state of health16.
A clinically relevant difference of the two metascores PCS and MCS from baseline to follow-up was defined as one half of one standard deviation of the difference to baseline assessment, and patient scores were considered similar without difference if the scores were within one fourth of one standard deviation of the mean17.
DATA COLLECTION AND FOLLOW-UP
QoL as well as adverse events were assessed at regular clinical follow-up in hospital or by standardised telephone interview. For patients with suspected events, relevant medical records, discharge letters and documentation of hospitalisation were systematically collected from treating hospitals and physicians in private practice. Baseline clinical and procedural characteristics and all follow-up data were entered into a dedicated database, held at an academic clinical trials unit (CTU Bern, Bern University Hospital, Bern, Switzerland) responsible for central data audits and maintenance of the database.
STATISTICAL ANALYSIS
Continuous variables are presented as mean ± standard deviation (SD) and were compared by means of Student’s t-test analysis. Categorical data are expressed as frequency (percentages), and Fisher’s exact tests were used for baseline and procedural comparisons. All statistical analyses were performed using SPSS statistical package, version 17.0 (SPSS Inc., Chicago, IL, USA). All p-values are results of two-tailed tests and values <0.05 were considered statistically significant.
Results
PATIENT POPULATION
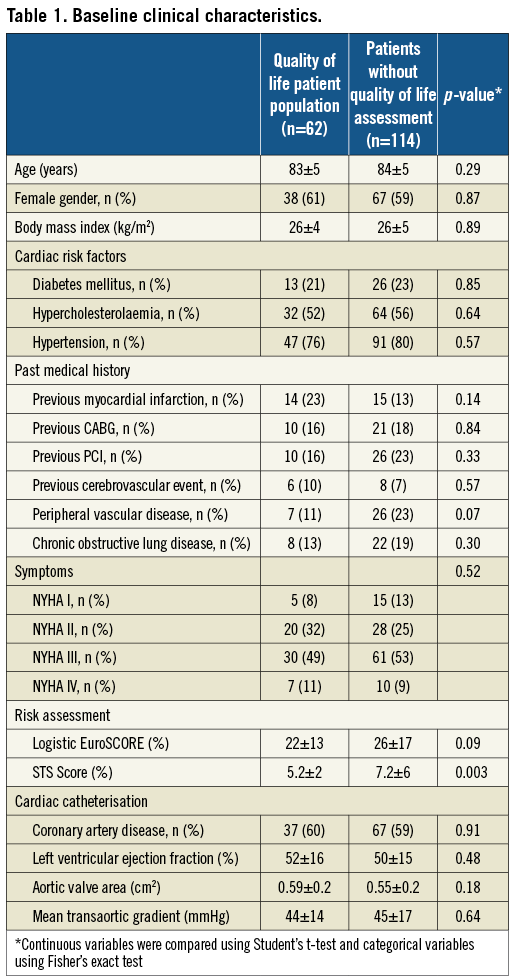
Baseline clinical characteristics of patients representing the QoL subgroup and patients without QoL assessment are shown in Table 1. Apart from a higher preoperative risk as calculated by the STS and the EuroSCORE as well as a higher rate of peripheral vascular disease in the patient population not receiving QoL assessment, there were no significant differences between patients with QoL and without QoL assessment in terms of cardiac risk factors, aortic valve stenosis severity and clinical symptoms.
PROCEDURAL CHARACTERISTICS AND CLINICAL OUTCOME
The majority of patients were treated with a Medtronic CoreValve bioprosthesis (n=54, 87%), whereas 8 (13%) patients underwent transfemoral implantation of an Edwards SAPIEN bioprosthesis. Concomitant percutaneous coronary intervention was performed in 9 (15%) patients, while another 9 (15%) patients underwent staged percutaneous coronary intervention. Compared to patients without QoL assessment, no significant differences were observed in terms of procedure time, type of anaesthesia, valve type allocation and the need for packed red blood cell transfusions of >2 units.
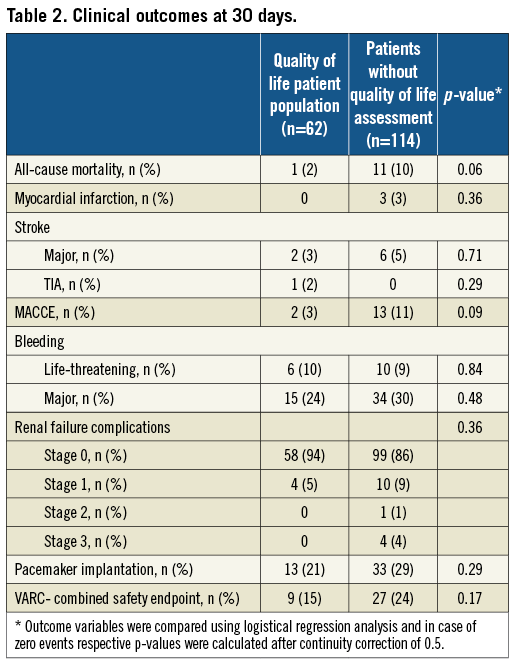
Clinical outcome was assessed at a median follow-up period of 264 days (211 to 351 days) and none of the patients was lost to follow-up. Clinical outcomes at 30 days are shown in Table 2. With the exception of a trend towards a higher rate of all-cause mortality in patients not receiving QoL assessment, there were no significant differences between patients with QoL and without QoL assessment for any VARC-defined endpoint including stroke, bleeding, access site complications and renal failure.
All patients underwent echocardiographic follow-up assessment showing a significant decrease in the transvalvular aortic mean gradient (43.7±14 mmHg to 8.2±4 mmHg, p<0.001) and an increase in aortic valve area (0.59±0.2 to 1.84±0.6, p<0.001) in patients with QoL follow-up assessment.
QUALITY OF LIFE ASSESSMENT (SF-36)
Six patients (10%) of the QoL patient population died during the follow-up period leaving a total of 56 patients for paired comparison of QoL parameters during follow-up.
At baseline, patients with symptomatic severe aortic stenosis showed substantial impairment in physical and mental health as shown in Figure 2. Comparison of baseline values with follow-up data nine months after TAVI showed considerable improvement in all aspects of health-related QoL. TAVI resulted in an increase of QoL in all eight subscales of the SF-36 questionnaire reaching statistical significance in physical functioning (PF, 37.0 to 59.0, p<0.0001), physical role functioning (RP, 18.3 to 49.1, p<0.0001), general health (GH, 55.9 to 64.9, p=0.001), vitality (VT, 40.7 to 51.3, p<0.001), social functioning (SF, 67.4 to 76.8, p=0.049), emotional functioning (RE, 52.0 to 75.8, p<0.001) and mental health (MH, 66.6 to 75.8, p=0.05). The subscale bodily pain (BP, 60.7 to 70.4, p=0.058) showed a strong trend to improvement, but failed to reach statistical significance. Apart from the eight subscales, the two metascores, the physical component summary score (PCS) and the mental component summary score (MCS) also showed improvement (PCS from 31.5 to 39.5, p<0.0001; MCS from 44.7 to 48.2, p=0.046) at 9-month follow-up (Figure 3).
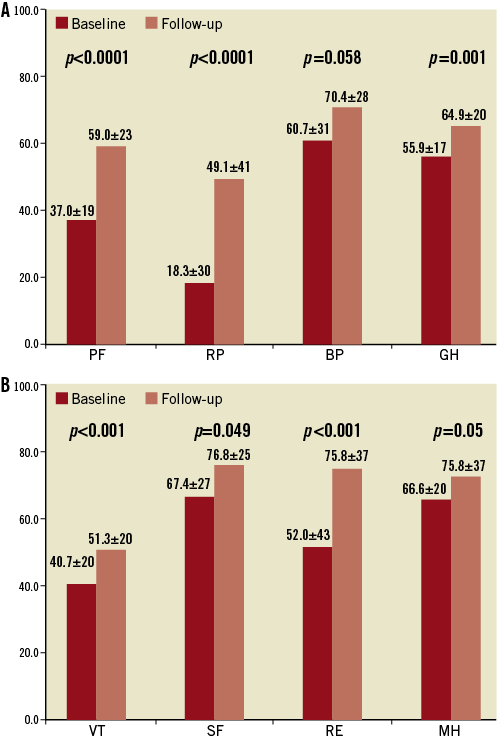
Figure 2. SF-36 data of patients with severe aortic stenosis undergoing transfemoral TAVI at baseline and follow-up. Physical health scales (A) and mental health scales (B) are shown. PF: physical functioning; RP: role physical; BP: bodily pain; GH: general health; VT: vitality; SF: social functioning; RE: role emotional; MH: mental health
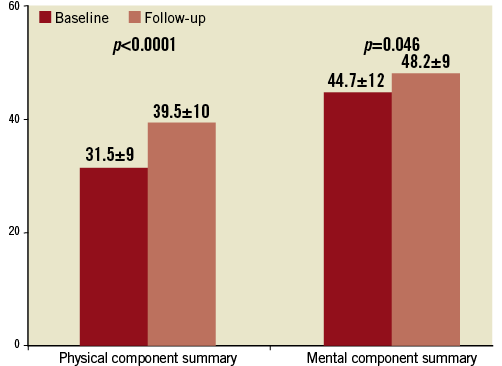
Figure 3. Physical Component and Health Component Summary scores represent the individual and summarised metascores data of the SF-36 health-related questionnaire.
Compared to baseline, the mean improvement in the PCS metascore amounted to 8±10 with a clinically relevant increase in 68% of patients. Accordingly, 32% of patients experienced no improvement or a minor deterioration, which was not related to a higher incidence of periprocedural complications (VARC Combined Safety Endpoint: PCS improvement 8% vs. no improvement 22%, p=0.195).
Analysing the results of the MCS metascore, we observed an overall improvement of 3.5±13 with 43% of patients showing clinically relevant improvement of mental health after TAVI. Conversely, 38% of patients experienced no improvement in the mental component of QoL, and 19% of patients had a minor decrease in these parameters. No significant differences were observed with respect to baseline characteristics, periprocedural complications and clinical outcome parameters between patients with and without improvement of the MCS metascore (VARC Combined Safety Endpoint: MCS improvement 13% vs. no improvement 13%, p=1.00).
Besides changes in physical status and mental health, TAVI substantially alleviated symptoms (Figure 4) and improved physical capacity: New York Heart Association (NYHA) functional class changed from 2.6±0.8 to 1.4±0.6 (p<0.0001) at follow-up. Only 3.2% of patients remained in NYHA class III, and none of them in class IV nine months after TAVI.
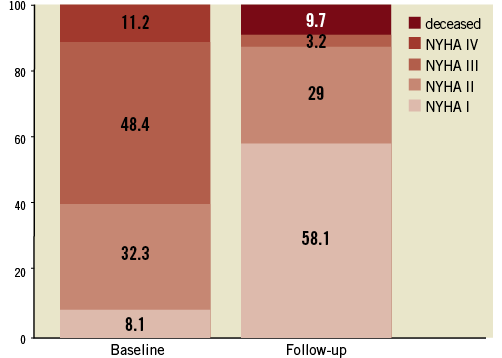
Figure 4. Exercise capacity assessed with the New York Heart Association (NYHA) functional classification in patients undergoing TAVI at baseline and follow-up assessment.
Discussion
The present analysis comprising 62 patients investigated changes in quality of life in response to TAVI, which from a patient’s perspective assumes similar importance to crude clinical outcomes. The main findings are that TAVI effectively alleviates symptoms and provides a rapid and sustained improvement in QoL. The improvements are comparable and similar to those previously described in patients undergoing percutaneous coronary intervention18, cardiac resynchronisation in chronic heart failure19 and radiofrequency ablation therapy in patients with cardiac arrhythmias20. All these cardiac interventions share with TAVI the rapid and sustained effect on symptom alleviation and improvement in all aspects of health-related QoL.
In our cohort of TAVI patients, the largest benefit was observed in physical components of the SF-36 questionnaire. A pronounced effect of clinically relevant improvement in the PCS metascore was present in 68% of patients, while the MCS metascore reached significant improvement in 43% of patients. Considering the improvement on a subscale level of the eight physical and mental elements of the SF-36 questionnaire, all components almost reached the QoL status of an age and gender adjusted normalised Western European reference population16. Taking age and comorbidities of this patient population into consideration, the increase in physical as well as mental-related QoL is remarkable. Pre-existing comorbidities were not associated with a lower change in postoperative perceived QoL and even periprocedural complications had no apparent influence on QoL-related outcome. Age itself is not able to minimise the improvement of postoperative health-related QoL as shown in patients undergoing cardiac valve surgery17. Sedrakyan and colleagues showed an increase of health-related QoL to almost normal levels of a healthy reference population 18 months after either aortic valve or mitral valve surgery. This effect was present in all subscales of the SF-36 questionnaire and not influenced by age at the time of operation. These findings are supported by the results of Lam et al21, in which octogenarians, although they were at higher operative risk and increased morbidity, perceive equal or even better gain in QoL compared to their younger counterparts after surgical aortic valve replacement.
TAVI, as a less invasive technique, shortens the recovery period and offers the possibility of early ambulation compared to conventional surgical aortic valve replacement. As a consequence, early improvement of symptoms and changes in health-related QoL have been observed in previous studies. By evaluating clinical outcome and quality of life three months after TAVI, Krane and co-workers observed significant improvement in symptoms and an increase in physical components of QoL22. In this survey three months after the intervention, the authors were not able to show an improvement in mental components of QoL. Five months after TAVI, Ussia et al were able to present further evidence of favourable outcome in terms of health-related QoL23. Using the shorter version of the SF-36 questionnaire, the SF-12 questionnaire, the authors observed a lasting effect in physical health and a significant improvement in mental components of health-related QoL. The positive effect on mental health might be related to the extended follow-up period as compared to the study of Krane et al. Similar findings were reported by Bekeredjian et al24 showing significant changes of physical as well as mental components compared to baseline QoL assessment six months after TAVI. While the authors pointed out that improvement of QoL was present in all patients, we observed a lack of improvement in either physical or mental components of health-related QoL in a small proportion of our patients. This observation was not related to any baseline or clinical outcome parameters and was more pronounced in the mental subscales of the QoL assessment. Regarding the overall less impressive improvement of mental health in our patient population, it can be speculated that it is more difficult for mental health status to be affected by a single intervention like TAVI.
More recently, the question whether TAVI provides potentially long-lasting improvement of QoL has been addressed by the PARTNER Investigators. In patients deemed inoperable, Reynolds and co-workers were able to show a remarkable increase in health-related QoL after TAVI compared to optimal medical treatment that was maintained at one-year follow-up25. These findings were underlined by the results of Ussia et al26 showing a sustained positive effect in physical as well as mental health components at mid-term follow-up, further confirming our data in patients after transfemoral TAVI.
Study limitations
This study has several limitations. The present report summarises the experience of a single institution with an overall limited number of patients undergoing only transfemoral TAVI procedures. However, the overall improvement in the subscales of the SF-36 questionnaire is comparable with previous reports of QoL after transfemoral TAVI and, as part of the study design, only transfemoral TAVI patients were considered eligible. Furthermore, we extended the previous reported health-related follow-up assessment up to nine months after TAVI, providing more evidence of the sustained benefit of this therapeutic intervention.
Conclusion
Health-related QoL is significantly impaired in patients with symptomatic severe aortic stenosis. TAVI improves all subscales of mental and physical health components and effectively alleviates symptoms.
Funding
This study was supported by research grants from Bern University Hospital and a grant of the Swiss National Science Foundation to SW (SNF Grant 32003B_135807).
Conflict of interest statement
S. Windecker has received honoraria and consultant fees from Edwards Lifesciences and Medtronic CoreValve. L. Buellesfeld is a consultant and proctor for Medtronic. P. Wenaweser is proctor and receives honoraria from Medtronic CoreValve and Edwards Lifesciences. A. Khattab has received speaker honoraria and proctor fees from Medtronic CoreValve and Edwards Lifesciences. The other authors have no conflicts of interest to declare.

