Abstract
Aims: Despite primary angioplasty being the recommended treatment for patients with acute myocardial infarction with ST-elevation, recent studies have shown a great heterogeneity in the access to this form of treatment in Europe. The project “Stent for Life”, an initiative of the European Society of Cardiology which Portugal joined in February 2011, aims to improve this situation.
Methods and results: The objective of this study was to re-evaluate the basic Portuguese performance indicators for primary angioplasty. A national survey called “Moment Zero” was implemented for a one-month period for this purpose. Nineteen Portuguese centres of interventional cardiology, where primary angioplasty is carried out, were invited to participate in this study. From 9th May to 8th June 2011, 14 centres participated in this study and 185 patients were included with a mean age of 62±14 years, of which 76.8% were male. 17.5% of the patients presented with a medical history of diabetes mellitus, 8.4% had previous percutaneous coronary intervention, 7.6% myocardial infarction and 1.1% coronary artery bypass surgery. Only 29% of the patients used the single national number for medical emergencies (112) to call for support. The median patient delay was 120 (73-240) minutes. The median pre-hospital transportation system delay was 104 (73-240) minutes. The median door-to-balloon delay (D2B) was 64 (30-110) minutes and was not significantly different between patients who contacted the National Institute for Medical Emergency (INEM) and patients who did not contact this service: 69 (30-109) minutes versus 60 (30-111) minutes. In 56% of the cases, patients entered a local hospital before transferring to a hospital with primary angioplasty facilities. The time between the admission to the local hospital and admission to a hospital with an interventional cardiology unit was 109 (73-173) minutes.
Conclusions: The main barriers to a better performance of the primary angioplasty programme in Portugal, as revealed by “Moment Zero”, are the low number of patients who contacted the INEM and the high number of patients who attended centres without interventional cardiology units, resulting in long delays spent in secondary transportation to the institutions with such services. The D2B delay, although close to the 90 minutes recommended by the guidelines, is not a good indicator of the overall performance of primary angioplasty in Portugal.
Introduction
Several randomised clinical trials1-5 and meta-analyses6 have shown that primary angioplasty, also known as primary percutaneous coronary intervention (p-PCI), is superior to fibrinolysis in reducing mortality as well as the risk of reinfarction and stroke. The European Society of Cardiology recommends reperfusion by p-PCI as soon as possible in patients with acute myocardial infarction with ST-elevation (STEMI), in the first 12 hours after onset of symptoms and with persistent ST-elevation (or new left bundle branch block) in the 12-lead ECG. The recommended time from the first medical contact (FMC) until p-PCI should be ≤2 hours for any STEMI and ≤90 min in patients symptomatic for less than two hours with extensive anterior STEMI and low haemorrhagic risk7,8.
Despite having a reasonably well-established primary angioplasty network, Portugal was one of the countries in Western Europe with lower rates of p-PCI per million inhabitants at the beginning of this millennium9,10. The project “Stent for Life”, an initiative of the European Society of Cardiology which Portugal joined in February 2011, aims to improve this situation11.
In the absence of national data which would allow a thorough assessment from the starting point of the disease (i.e., a national prospective registry which would include all Portuguese patients with STEMI), a prospective registry, defined as “Moment Zero”, was designed with the purpose of assisting the Stent for Life Task Force in the launch of an action plan, aimed at the fields where the performance deficits would be most critical.
Methods
The study was based on a survey sent to all centres of mainland Portugal with an interventional cardiology unit active 24 hours/7 days and which follow p-PCI protocols. The objective was to register, for one month (from 9th May to 8th June 2011), all catheterised patients with a presumed diagnosis of STEMI up to 12 hours after the onset of symptoms.
The purpose of the survey was to determine if the patient did or did not use the single national number for medical emergencies (112) in order to obtain direct assistance from the National Institute for Medical Emergency (INEM), as well as the transportation used to attend the centre for primary angioplasty. It was also noted if the patient attended another hospital before attending an institution with p-PCI.
The survey also aimed to register the observed time periods between the onset of pain and the primary angioplasty treatment: 1) patient delay (time between the onset of pain and the moment of first medical contact - FMC); 2) pre-hospital transportation delay (time between FMC and hospital attendance); 3) local hospital delay (time between attendance at the local hospital and attendance at the hospital with p-PCI facilities); 4) door-to-balloon (D2B) delay (time between attendance at the hospital with p-PCI and application of the first vascular opening device in the lesion that caused the infarction).
System delay was defined as the sum of transport delay and D2B; for cases where the patient attended a local hospital this period was also added. For patients without FMC who presented directly at a hospital with p-PCI facilities, the system delay was equal to D2B delay.
Treatment delay was defined as the time between the onset of symptoms and application of the first vascular opening device in the lesion responsible for the infarction (sum of patient delay and system delay).
No data were collected regarding the clinical outcomes of the performed interventions.
Statistical analysis
Qualitative variables were summarised by counts and percentages and quantitative variables by median and interquartile range, unless otherwise specified (e.g., age).
The Mann-Whitney non-parametric test was performed to compare the groups of patients who did and did not contact INEM in relation to quantitative variables.
Statistical tests were two-pronged considering a significance level of 5%.
Statistical analysis was performed through the software IBM® SPSS® Statistics 18.
Results
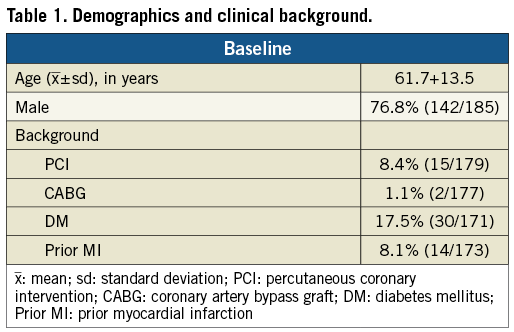
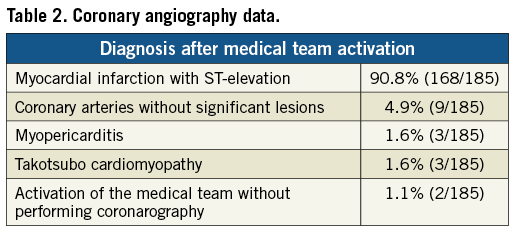
Of the 19 centres which perform p-PCI in mainland Portugal, 14 participated in this study (representing 79% of the patients treated by this procedure in 2011) and included data from 185 patients, which represented the total number of patients assessed and treated during that period. Table 1 presents demographic data and clinical background information. Patients’ mean age was 62±14 years and 76.8% were male. In 90.8% of the patients the diagnosis of STEMI was confirmed and in 4.9% coronarography did not show significant lesions (Table 2).
Only 29% of the patients used the national single number for medical emergencies to request assistance. This single number allows direct access to the INEM, which has the responsibility for pre-hospital transportation.
The median patient delay was 120 (73-240) minutes. There was a statistically significant difference (p=0.002) between the group of patients who contacted the INEM for support and the group of patients who did not: median of 98 (60-148) minutes vs. 166 (89-279) minutes.
The median pre-hospital transportation delay was 104 (60-153) minutes, while the median D2B delay was 64 (30-110) minutes. D2B delay was not significantly different between patients who contacted the INEM for assistance and patients who did not: median of 69 (39-109) minutes vs. 60 (30-111) minutes. These results are shown in Figure 1.
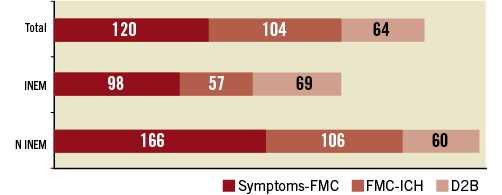
Figure 1. Treatment delay.
INEM: called the National Medical Emergency Institute; N INEM: did not call the National Medical Emergency Institute; Symptoms-FMC: beginning of symptoms to first medical contact (patient delay); FMC-ICH: first medical contact to interventional cardiology hospital (pre-hospital transportation delay); D2B: door-to-balloon delay
In 56% of cases, patients attended a local hospital before attending the hospital with p-PCI facilities. The median local hospital delay was 109 (73-173) minutes.
The median system delay was 110 (75-166) minutes. This time was significantly lower in patients who were directly transported to a centre with an interventional cardiology unit in comparison with patients who had a first medical contact in a hospital without that unit (88 vs.130; p=0.002). System delay showed a lower trend in the group of patients who contacted the INEM for assistance compared with the group who did not: 84 (69-172) minutes vs.115 (81-164) minutes, p=0.099.
The median treatment delay was 276 (179-46) minutes, with a significantly lower time in the group of patients who contacted INEM (206 vs. 312; p=0.024). Treatment delay in the subgroup of patients who were previously assisted in a hospital without an interventional cardiology unit was significantly higher than the subgroup of patients that did not attend a local hospital (338 vs. 226; p=0.003).
Discussion
PATIENT DELAY
This study highlights the low percentage of patients who used the national single number for medical emergencies to request assistance (29%). These results confirm the official data published by the Portuguese Ministry of Health in 2009 and 2010, in which only 23% of patients resorted to the INEM through this contact number12. By means of a public advertising campaign, the Stent for Life Task Force in Portugal has been focusing its attention on raising awareness of the symptoms of myocardial infarction and the proper actions to be carried out in order to obtain timely and adequate treatment.
An important aspect to be addressed by this campaign is to reduce the proportion of patients who attend the hospital more than 12 hours after the onset of symptoms. According to the National Registry of Acute Coronary Syndromes, from 2002 to 20089, of the 37.3% of patients not submitted to any revascularisation procedure, the cause in 55% of cases was attendance at the hospital more than 12 hours after the onset of symptoms. One final aspect revealed by this study was a long time period from the onset of symptoms to FMC (median of 120 minutes).
The performance of different media campaigns has provided conflicting results regarding the impact of patient delay time13. The only campaign which evaluated the effect of this period on mortality found no difference in mortality during the year of the campaign compared with the previous period14.
SYSTEM DELAY
The median system delay was 110 minutes, a value within the recommended guidelines (which is 120 minutes)7,15. However, the analysis of system delay in the different ways a patient arrives at the primary angioplasty centre suggests that it is possible to obtain a lower system delay if the patient were to be directly transported to a centre with an interventional cardiology unit without having passed through a centre without that unit (88 vs.130 minutes) and will possibly be lower if the initial contact was through the INEM (84 vs.115 minutes).
Pre-hospital transportation delay was lower in patients who contacted the INEM, compared to patients who did not (57 min vs.106 minutes). At present, the INEM vehicles are equipped with telemetry and a physician and a nurse, who monitor the patient during transportation, contact the attending cardiologist at the hospital with an interventional cardiology unit directly by phone. This allows the timely preparation of the angiography room for the arrival of the patient without needing to pass through the emergency room.
The first initiatives designed to improve the performance of p-PCI were mainly focused on intra-hospital timings. D2B Alliance considered the D2B delay “a key indicator of quality of care in STEMI patients treated with p-PCI”. Recently, several authors have highlighted the system delay as the indicator of service quality and clinical outcomes16-18. This study demonstrates that the isolated evaluation of the D2B delay is not a good indicator of the global performance of p-PCI. Overall, the median period was 64 minutes, not substantially different from guideline recommendations7,15. For D2B delay, no significant differences were observed between patients who contacted the INEM (median of 69 minutes) and patients who did not (median of 60 minutes).
Unequivocally, the high number of patients who attended local hospitals before being admitted to a hospital with p-PCI (56%) was the main cause for the long time period between onset of symptoms and hospital attendance. An important barrier to overcome is the secondary transportation between local hospitals and centres with p-PCI facilities. This transportation is not the responsibility of the INEM, who are only accountable for pre-hospital transportation. There is no national system defined for this type of transportation and, once the patient is seen by a physician in a hospital, the level of care provided by healthcare professionals must not be reduced. Therefore, further transportation must be carried out in an ambulance, with the supervision of a physician. Due to the shortage of physicians in the emergency units, this procedure leads to prolonged local hospital delays.
These results are in accordance with other, single-centre studies, carried out in Portugal19,20.
SUMMARY
The association between the time of myocardial ischaemia and STEMI prognosis is clearly established. It is thus a priority to obtain myocardial perfusion within the shortest time interval. Through its “know-how”, the Stent for Life Initiative may be of great assistance in improving the performance of p-PCI21. The main barriers to overcome include the low number of patients who contact the single national number for medical emergencies, as well as the high number of patients who attend local hospitals without p-PCI facilities, with consequential high delays in the secondary transportation to the interventional centres.
The D2B delay, despite being close to the 90 minutes recommended by the guidelines, is not a good indicator of the overall performance of p-PCI in Portugal.
Acknowledgements
The author of this study would like to acknowledge the support given by Dr Sofia de Mello (Project Manager of SFL Portugal) and Dr Ernesto Pereira (Task Force Member) for providing valuable assistance in data collection and analysis.
Participating centres: Hospital Braga (Dr. João Costa), Hospital S. João (Dr João Carlos Silva), Hospital Santo António (Dr Henrique Carvalho), Centro Hospitalar Vila Nova de Gaia (Dr Vasco Gama Fernandes), Hospital de Viseu (Dr João Pipa), Centro Hospitalar de Coimbra (Dr Leitão Marques), Hospital de Leiria (Dr João Morais), Hospital Fernando da Fonseca (Dr Pedro Farto e Abreu), Hospital de Santa Maria (Dr Pedro Canas da Silva), Hospital Pulido Valente (Dr Pedro Cardoso), Hospital de Santa Marta (Dr Rui Ferreira), Hospital Curry Cabral (Dr Luís Mourão), Hospital Garcia de Orta (Dr Hélder Pereira), Hospital Setúbal (Dr Ricardo Santos), Hospital de Évora (Dr Lino Patrício e Dr Renato Fernandes) and H de Faro (Dr Victor Brandão).
Conflict of interest statement
The author has no conflict of interest to declare.