Abstract
Aims: The aim of this study was to report the feasibility and the preliminary outcomes after transcatheter aortic valve implantation (TAVI) in the frail and unique high-risk population of patients with systemic sclerosis (SSc) and severe aortic stenosis (AS).
Methods and results: All patients with SSc and severe AS treated with TAVI between November 2007 and June 2013 in our centre were included in the current study. Outcomes were assessed using the Valve Academic Research Consortium 2 (VARC-2) definitions. Of 526 surgical high-risk patients treated in the study period, only six had SSc (1.1%). All SSc patients underwent transfemoral TAVI under conscious sedation. The procedure was successfully performed in all patients. There was one case of a major vascular complication. During a median follow-up time of 550 days (interquartile range 390-1,009 days), five of the six patients were alive, free from any complications and with an NYHA Class I or II. One patient died at 670 days from a stroke of unknown aetiology.
Conclusions: The present case series suggests that the TAVI procedure is feasible in patients with SSc and severe AS.
Introduction
Systemic sclerosis (SSc) is a connective tissue disease characterised by excessive deposition of collagen in the skin and internal organs, immunologic abnormalities and systemic microvascular and macrovascular dysfunction1. Although cardiac involvement is a well-known complication correlated with poor prognosis in patients affected by SSc, valvular involvement is not considered a typical manifestation of scleroderma heart disease2. However, given the prolonged course of the disease, it is not uncommon for SSc patients to present with degenerative aortic valve stenosis (AS). Recent studies have reported that premature onset of severe AS may represent yet another cardiac complication of SSc. If left untreated, the presence of AS might preclude the use of the standard adjunctive vasoactive therapies required to control the scleroderma-related pulmonary artery hypertension (PAH), Raynaud’s phenomenon and digital vasculopathy. Nevertheless, there is a paucity of data on the prevalence and management of severe AS in SSc patients3,4. The aim of this study is to report safety and efficacy outcomes in SSc patients undergoing transcatheter aortic valve implantation (TAVI).
Methods and results
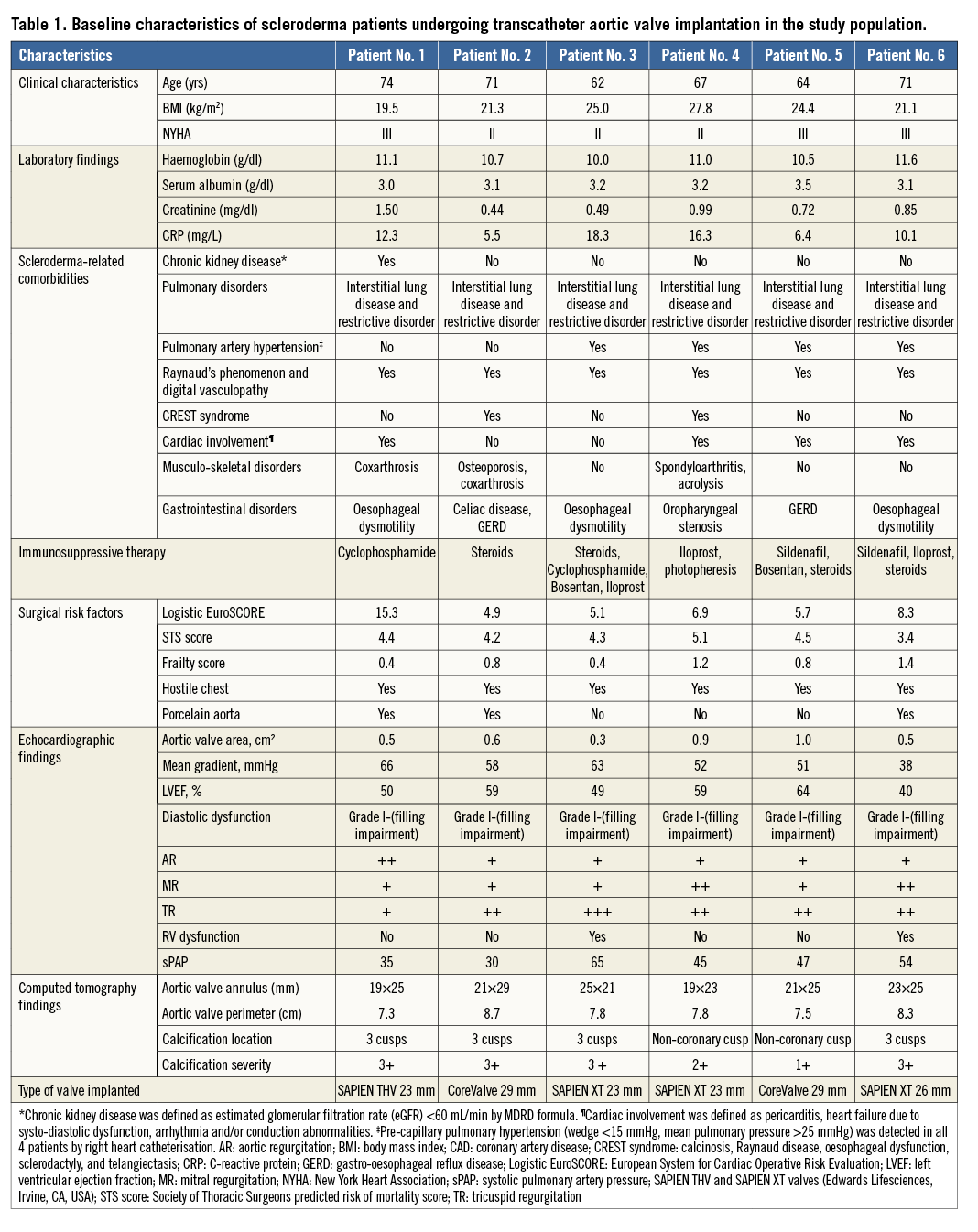
Among 526 surgical high-risk patients undergoing TAVI for severe AS from November 2007 to June 2013 in our hospital, six (1.1%) SSc patients were prospectively analysed. Outcomes were assessed using the Valve Academic Research Consortium 2 (VARC-2) criteria5. Table 1 reports baseline clinical, laboratory and echocardiography characteristics. All patients were female, with a mean age of 68.2±4.6 years. Despite the intermediate mean logistic European System for Cardiac Operative Risk Evaluation (EuroSCORE) and the Society of Thoracic Surgeons (STS) scores, these patients were deemed unsuitable for surgery because of the presence of a hostile chest (thoracic skin disease involvement), significant pre-capillary PAH in 4/6 and porcelain aorta in 3/6. TAVI was successfully performed using the transfemoral approach under conscious sedation in all patients. No intraprocedural deaths occurred. Only one patient had a major periprocedural vascular complication requiring coil embolisation. New left bundle branch block occurred in one patient immediately after implantation of a CoreValve® prosthesis (Medtronic, Minneapolis, MN, USA). Postoperative echocardiography revealed a normal position and function of the prosthesis in all patients. The mean post-implantation prosthetic gradient was 7.4±1.9 mmHg, and only one patient had mild paravalvular aortic regurgitation. No VARC-2 adverse events were observed at 30 days. During a median follow-up of 550 days (IQR 390-1,009), five out of six patients survived without any complications and reported an improved NHYA Class I or II. There was one death 670 days after the procedure due to a stroke of unknown aetiology. One-year follow-up transthoracic echocardiography demonstrated normal function of the valves with a mean prosthetic gradient of 8.2±2.0 mmHg and a mean systolic PAP of 36.3±3.3 mmHg (significantly reduced compared to baseline 46±12.7 mmHg, p=0.014). Amongst patients with pre-TAVI PAH, mean sPAP value reduced from 52.8±9 mmHg (pre-TAVI) to 39.5±5.4 mmHg at one-year follow-up (p=0.005). Only one patient showed mild paravalvular aortic regurgitation, which was already present at post-implantation echocardiography.
Discussion
In the current study, TAVI appeared to be a safe and effective procedure in SSc patients with inoperable AS due to specific comorbidities (thoracic skin involvement and pulmonary fibrosis/hypertension). In our centre, scleroderma patients accounted for 1.1% of patients who underwent transfemoral TAVI for severe AS.
Cardiac involvement is a well-known complication of SSc. Even though the aetiopathogenetic mechanism of AS in SSc remains unknown, the underlying inflammatory burden which accompanies SSc might play a role in accelerating the progression of AS in such patients4. Indeed, SSc is characterised by immune system activation, endothelial dysfunction, widespread microvascular and macrovascular damage and by enhanced fibroblast activity, factors which are also implicated in the development of AS1. Therefore, in SSc patients the presence of AS should be investigated, in order to be identified promptly and managed.
Risk assessment and appropriate patient selection in the SSc population is extremely important, as their cluster of comorbidities may account for a high or prohibitive operative risk for AVR. PAH, pulmonary fibrosis and restrictive lung disease, all frequently encountered in SSc, have a significant impact on outcomes, when these patients undergo AVR4,5. SSc patients are often rendered inoperable due to the presence of hostile chest or porcelain aorta. Notably, all of our patients had hostile chest secondary to chest wall fibrosis. Additionally, porcelain aorta was detected in half of the patients. Frailty, common in SSc, is also an important factor that can significantly affect AVR outcomes. All these high-risk features present in SSc patients render the STS score and logistic EuroSCORE suboptimal models for adequate risk stratification5. A further concern when planning a surgical AVR in SSc patients is the impact of anti-inflammatory/immunomodulatory medications on the periprocedural period and, in particular, on wound healing.
The potential advantages of TAVI over surgical AVR in SSc are the avoidance of general anaesthesia, sternotomy/aortotomy on a hostile chest anatomy, and a shorter in-hospital stay with less complex periprocedural management. Our experience suggests that TAVI is associated with technical success and encouraging long-term clinical outcomes in SSc patients. Operators should be aware of the risk of vascular complications in this particular subgroup of patients who are predominantly female with vessels of smaller calibre, and high rates of macrovascular/microvascular disease. In addition, in order to minimise the risk of acute kidney injury, the contrast administration during both CT scan and TAVI procedure should be reduced and an optimal hydration protocol followed. In the immediate post-procedural period, particular attention must be given to the increased risk of high atrioventricular block especially in SSc patients with baseline conduction disturbances.
Conclusion
In conclusion, although limited by the small sample size, our study suggests that TAVI can be a safe and effective treatment for patients affected by SSc and severe AS at high surgical risk. Further, larger studies are warranted to confirm these results.
| Impact on daily practice SSc patients with severe AS represent a rare patient population at extreme risk for surgical aortic valve replacement. Indeed, this population features particular comorbidities (hostile chest, pulmonary hypertension and fibrosis, porcelain aorta, immunomodulatory therapies) that favour a percutaneous treatment of the AS. The present case series highlights the importance of a multidisciplinary Heart Team evaluation of AS management in SSc patients, who, despite their low-intermediate risk scores, are not always suitable for surgical AVR due to the presence of specific comorbidities. Further, this preliminary experience suggests that TAVI could be a viable therapeutic option in these frail patients, being associated with encouraging long-term clinical outcomes and a low rate of periprocedural complications. |
Conflict of interest statement
M. Montorfano is a proctor for Edwards Lifesciences. A. Latib serves on the Medtronic Advisory Board and is a proctor for Direct Flow Medical. A. Colombo is a minor shareholder of Direct Flow Medical. The other authors have no conflicts of interest to declare.

