The majority of transcatheter aortic valve implantation (TAVI) studies aimed to recruit “inoperable” patients or patients at “too high risk for surgical AVR”; the operative risk was evaluated by clinical judgement in association with a more quantitative assessment based on scoring systems, especially the EuroSCORE1 or STS (Society of Thoracic Surgeons) risk score2. However, with the introduction of TAVI in Germany an unexpected decrease in the number of “surgical” aortic valve replacement (AVR) from 18,588 in 2008 to 17,344 in 2009 was observed, while previous to that, the number of AVR increased by approximately 200 patients per year3,4. It seems that patients previously considered for surgical AVR underwent TAVI.
The main problem in clinical trials as well as daily practice is currently the quantitative assessment of operative risk: although it is clear that the logistic EuroSCORE highly overestimates the operative risk in aortic valve patients5-8, in three of seven of the recently published larger TAVI studies, only the EuroSCORE was used9-11. In order to exemplify the performance of the EuroSCORE and STS risk score we compared the predicted mortality in several TAVI studies and in “high-risk” patients undergoing isolated AVR at our institute (Mediclin Heart Institute Lahr/Baden, Lahr, Germany) to the observed 30-day mortality12 in Figure 1: the logistic EuroSCORE overestimates the observed mortality about three times in TAVI and in surgical AVR patients. This miscalculation may lead to a relative overestimation of the operative risk after AVR and an overoptimistic interpretation of the short-term outcome after TAVI.
A main counter-argument against the currently available risk scores is that several important risk factors, e.g., porcelain aorta, frailty or, especially for transcatheter AVI, e.g., size of peripheral vessels and state of aortic annulus, are not included in present risk models13. However, the STS risk score predicted the operative mortality almost properly not only after surgical AVR but also after transcatheter AVI (Figure 1).
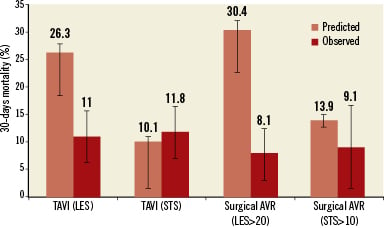
Figure 1. Comparison of mean observed and predicted 30-day mortality by logistic EuroSCORE (LES) and the STS-PROM (STS) from several TAVI studies and from data of patients undergoing isolated AVR in the authors institute (Mediclin Heart Institute Lahr/Baden, Lahr, Germany) with a EuroSCORE greater than 20 (LES>20) and with a STS-PROM greater than 10 (STS>10). TAVI (LES)9-11,14, TAVI (STS)14-16.
According to our experience in octogenarians undergoing AVR, the combination of the three simple risk factors: very high age, reduced ejection fraction and being underweight, already indicates an excessive operative risk (30-day mortality: 12.7%, STS: 9.6±6.2)8. Regarding also the 6-month mortality of 26% in these high-risk octogenarians after surgical AVR, the need for a less invasive therapy, possibly TAVI, becomes obvious.
Ideally, the current risk scores should be improved concerning additional risk factors and should consider the long-term benefit of an intervention. At the moment, we suggest the use of the STS risk score2, because the quantitative assessment of an interventional risk is necessary to identify high-risk patients and to enable a simple risk-adjusted comparison between different therapies and studies.
Conflict of interest statement
I. Florath has a research grant for stentless Freestyle® heart valve studies from Medtronic Inc., Duesseldorf, Germany. A. Albert has no conflict of interest to declare.

