In this issue of EuroIntervention, Thuijs et al1 report on the predictive performance of the Society of Thoracic Surgeons (STS) risk score in patients undergoing coronary artery bypass surgery (CABG) or percutaneous coronary intervention (PCI) for left main coronary artery disease (CAD) in a post hoc analysis of the EXCEL trial2.
The authors have assessed the STS predicted risk of mortality, stroke, and renal failure risk models for 30-day outcomes in both the CABG and PCI cohorts. The main findings were the following: (1) the STS score predictive accuracy for 30-day mortality and acute kidney injury was good for CABG but poor for PCI; and (2) the STS score predictive accuracy for 30-day stroke was good for both CABG and PCI.
While the authors should be congratulated for a clear and concise presentation of the data, the findings are not surprising for several reasons. First, and as the authors point out, the STS score was originally derived from a logistic model sourced from a cohort of patients undergoing open heart surgery with variables independently associated with adverse events after CABG, not after PCI. Therefore, it is not surprising that the STS risk score demonstrated poor predictive accuracy for mortality and renal insufficiency after PCI. Indeed, the less invasive nature of percutaneous revascularisation is well known to be associated with significantly lower short-term mortality and major adverse events such as bleeding, infection, readmission, and acute kidney injury. Second, only a few factors predict periprocedural (30-day) mortality after PCI, with the anatomical/technical complexity of the procedure being, by far, the most important one3. The well-known SYNTAX score is probably the best tool to capture the anatomical complexity of a percutaneous procedure, and is, therefore, the most predictive score for major adverse events after PCI4. Obviously, the STS score does not consider the anatomical complexity and extent of CAD, once again explaining the lack of predictive accuracy for 30-day adverse events. Finally, it is also not surprising that the STS score demonstrated a good predictive value for stroke among patients undergoing PCI. Indeed, a non-negligible proportion of stroke after PCI (and CABG) is explained not by technical factors but rather by patient-related factors and concomitant comorbidities (e.g., atrial fibrillation, peripheral vascular disease, prior stroke), which were similar at baseline in the PCI and CABG groups.
The lack of predictive accuracy of the STS score relative to non-surgical procedures (percutaneous intervention) has been shown in other fields. Indeed, the STS score was shown to be non-predictive for transcatheter aortic valve procedures5. This led to the development of more appropriate scores, such as the TAVR score6. To entertain the idea that a score developed from and for surgical procedures will also bring predictive value for less invasive counterparts could be seen as overly optimistic. Historically speaking, risk stratification for complex CAD or left main coronary artery revascularisation has evolved over the past decade and has consistently demonstrated the superiority of combining anatomic factors and clinical factors to ensure the accurate predictability of risk models7,8,9. These efforts culminated in the emergence of the individualised SYNTAX score II, in which six clinical variables were combined with the anatomical SYNTAX score to derive two distinct and individualised risks for PCI and CABG for a given patient10. Ultimately, the use of the SYNTAX score II paired with a Heart Team discussion, which provides a “safety net” for these scores, provides the best chance for appropriate risk stratification and selection of the most appropriate therapy for a given patient11.
What does the article by Thuijs et al mean in practice? The clear message from this article is that a single score (STS in the current situation) is insufficient to capture the entire complexity of a patient in need of complex revascularisation and is insufficient for adequate risk stratification of patients undergoing left main coronary artery (LMCA) revascularisation. While the quest to design a “perfect” predictive approach for both PCI and CABG is still ongoing (SYNTAX score II is a good start), most experienced clinicians, when facing complex CAD or CAD involving the left main coronary artery, sequentially do the following: (1) clinically assess patient risk for surgical revascularisation (visually/clinically and/or via STS or EuroSCORE calculation); (2) assess anatomical complexity for revascularisation (via SYNTAX score or visually/instinctively); and (3) discuss (in person or virtually) with involved colleagues (cardiothoracic surgeons and interventional cardiologists) and come to a consensus (officially called the Heart Team approach).
In brief, each patient presenting with LMCA disease is complex and deserves a comprehensive and individualised approach. Whether a single score would ever be able to capture, integrate, and deliver an accurate risk prediction leading to an appropriate revascularisation strategy recommendation remains to be demonstrated. In the meantime, a shared decision-making approach, integrating anatomical, clinical, and other holistic factors including a Heart Team approach, should remain the standard of care (Figure 1).
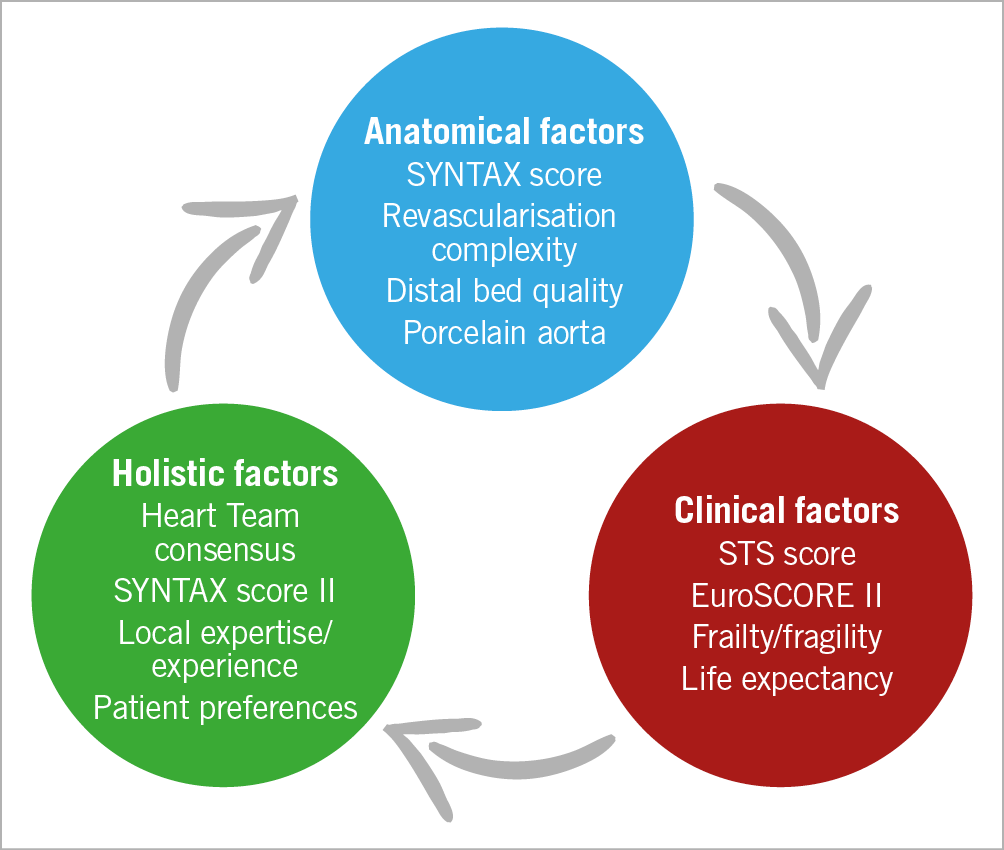
Figure 1. Potential factors and considerations involved in the shared decision-making process for patients undergoing complex and left main coronary artery disease revascularisation. STS: Society of Thoracic Surgeons
Conflict of interest statement
P. Généreux reports receiving speaker fees from Abiomed, Edwards Lifesciences and Cordis, being a consultant for Abiomed, Boston Scientific, Cardiovascular Systems, Inc., Cordis, Edwards Lifesciences, Medtronic, Opsens, Soundbite Medical Solutions Inc., Pi-Cardia, Saranas, Siemens and SIG.NUM, and being a shareholder in Soundbite Medical Solutions Inc., SIG.NUM, Pi-Cardia, and Puzzle Medical. The other author has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.