Abstract
Background: MAC is commonly found in patients affected with MR, and it is associated with high morbidity, mortality and worse cardiac surgical outcomes. Transcatheter edge-to-edge repair could be an alternative treatment, although there is little evidence in this population.
Aims: The aim of this study was to analyse the safety, efficacy and durability of MitraClip implantation in patients affected with mitral regurgitation (MR) and mitral annulus calcification (MAC).
Methods: We analysed the outcomes of 61 suitable patients affected with severe MR and moderate or severe MAC (the “MAC” group) and 791 patients with no or mild MAC (the “NoMAC” group) treated with the MitraClip device.
Results: Procedural success was similar (91.8% vs 95.1%, p=0.268, in MAC and NoMAC, respectively), with a very low rate of complications. At one-year follow-up, 90.6% of MAC and 79.5% of NoMAC patients had MR grade ≤2 (p=0.129), 80% in both groups remained in NYHA Functional Class ≤II, and a significant reduction in cardiac readmissions was observed (65% vs 78% in MAC vs NoMAC, p=0.145). One-year mortality tended to be higher in MAC patients (19.7% vs 11.3%, p=0.050), with no difference in cardiovascular mortality (15.3% vs 9.2%, p=0.129).
Conclusions: MitraClip use in selected patients with moderate or severe MAC is safe, feasible and achieves good clinical and echocardiographic results at one-year follow-up.
Introduction
Mitral annular calcification (MAC) is a chronic degenerative process of increasing prevalence in developed countries which can be present in up to 24% of patients referred for mitral valve surgery123. It has been associated with several conditions including age and female sex, and some cardiovascular risk factors such as hypertension, diabetes mellitus, dyslipidaemia and smoking habit or chronic kidney disease. However, the mechanisms in which these conditions could lead to the development of MAC are still not clear. Clinically, MAC has been related to the presence of vascular disease, arrhythmia and mitral valve disease1245678.
Anatomically, MAC is found most commonly in the posterior annulus, but calcification might extend beyond the annulus19 to the leaflets and subvalvular apparatus. Surgery of the mitral valve in this setting remains a challenge, MAC being a strong predictor of mortality and worse cardiac surgical outcomes in previous surgical reports1101112131415161718. In recent years, surgical techniques have evolved in this field accomplishing better survival rates; however, there remains a non-negligible rate of post-operative complications1619. The high morbidity of patients with MAC together with the surgical complexity have fuelled an urgent need for less invasive strategies for treating these patients.
Transcatheter edge-to-edge mitral valve repair with the MitraClip system (Abbott Vascular) has been established as a valid alternative to surgery in high surgical risk patients with severe mitral regurgitation (MR)20212223242526. However, its efficacy in patients affected with MAC remains uncertain, given the paucity of data and the poor outcomes observed with the Alfieri surgical technique in this setting272829. Moreover, these patients have been excluded from randomised clinical trials, based on the assumption that this calcification might extend to the
leaflets or might induce high mitral gradients after edge-to-edge repair. Hence, we sought to analyse the safety and efficacy of the MitraClip system in patients who presented moderate or severe MAC and who were otherwise suitable candidates for this treatment, focusing on procedural success, durability and clinical benefit in a “real-world” setting.
Methods
The Spanish MitraClip multicentre registry prospectively included all consecutive patients with symptomatic MR grade ≥3 undergoing transcatheter mitral valve repair from June 2012 in 24 participating institutions. This study evaluated the data from all patients enrolled by seven of these participating institutions. All patients signed informed consent for the procedure and all studies were performed with the approval of the local ethics committee.
In all participant sites, patients were evaluated by a multidisciplinary team, which included a non-interventional cardiologist, an interventional cardiologist, a cardiothoracic surgeon and an anaesthetist. All patients deemed to be at high risk for surgery were considered for percutaneous repair. Anatomically, patients with calcification that extended to the margin of the leaflets, had short (<7 mm) or thick leaflets (>5 mm) or had a preprocedural mean gradient greater than 5 mmHg or a mitral area <4 cm² were declined for percutaneous repair.
Baseline demographics and echocardiographic parameters
Baseline demographic parameters included age, gender, weight and height, hypertension, diabetes mellitus, renal impairment and chronic haemodialysis, smoking, atrial fibrillation, previous cerebrovascular disease, ischaemic heart disease, New York Heart Association (NYHA) Functional Class, Society of Thoracic Surgeons (STS) score and heart failure hospitalisation during the previous year. Baseline echocardiographic parameters were based on preprocedural transthoracic echocardiography (TTE) and transoesophageal echocardiography (TEE) following the European Association of Cardiovascular Imaging recommendations3031. A categorical classification of MAC grade based on preprocedural echocardiography was used considering: 1) mild calcification of the annulus, when calcification was limited to less than one third of the annulus; 2) moderate calcification, when it involved one third to two thirds of the annulus, and 3) severe calcification, when it involved more than two thirds of the annulus or in case of a thickness >4 mm79. Two groups were defined according to the MAC grade: “NoMAC”, when no or mild annulus calcification was present, and “MAC”, when moderate or severe mitral annulus calcification was found.
Procedural success and complexity
Technical success was defined as correct implantation of at least one clip and the absence of procedural mortality or emergent cardiovascular intervention related to the implantation of the device or vascular access32. Procedural success was defined as MR grade reduction to 2 or less32. Procedure duration, number of clips and acute complications were recorded in order to assess the complexity of the repair. Procedure duration was defined as the duration from anaesthetic induction to the end of the procedure. Procedure-related bleeding and its severity were defined according to the Bleeding Academic Research Consortium (BARC) criteria32.
Echocardiographic and clinical follow-up
At follow-up, NYHA Class, MR grade, mean mitral gradient, systolic pulmonary artery pressure (SPAP), left ventricular ejection fraction (LVEF) and left ventricular dimensions were recorded as well as the need for subsequent mitral valve surgery, heart failure rehospitalisation and mortality.
Statistical analysis
Frequencies were calculated for categorical variables whereas mean±standard deviation (SD) or median (interquartile range) were calculated for numerical variables according to their distribution. Assessment of normality was performed using the Shapiro-Wilk test. Differences between groups were tested using the chi-square test for categorical variables and the Student’s t-test, Kruskal-Wallis or Mann-Whitney U test for continuous variables. A 95% level of significance was applied in the statistical tests (p<0.05). The Kaplan-Meier survival estimator was used to determine the time to all-cause mortality, cardiovascular mortality and readmissions for heart failure at one-year follow-up. Data from the survival curves and event-free survival rates along with the log-rank test were used for comparison between groups. Multivariate analysis of the association of MAC grade was performed using Cox proportional hazards modelling. The Stata 13.1 statistical package was used for data analysis (StataCorp).
Results
Baseline demographics and echocardiographic parameters
The baseline characteristics of the two groups are shown in Table 1. A total of 852 patients were included. Of these, 256 (30%) presented some degree of MAC: 42 (5.5%) were found to have moderate MAC and 19 (2.5%) had severe MAC. Therefore, 61 patients were allocated to the MAC group and 791 to the NoMAC group. MAC patients were older (78.3±8.7 vs 72.8±10.4 years old, p=0.001) and mostly female (44.3% male in the MAC group vs 66% male in the NoMAC group, p=0.001), more frequently had a history of previous non-mitral valvular intervention (24.6% vs 11.3%, p=0.002) and presented worse NYHA Functional Class (95% vs 85% NYHA Class ≥3, p=0.037) and STS score (4 vs 3, p=0.027) at the time of repair. On the other hand, NoMAC patients were more commonly smokers (48.5% vs 29.5%, p=0.004). There were no differences between groups in relation to hypertension, diabetes mellitus, chronic kidney disease or haemodialysis, previous stroke, ischaemic heart disease, rate of previous percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) as well as for the EuroSCORE II.
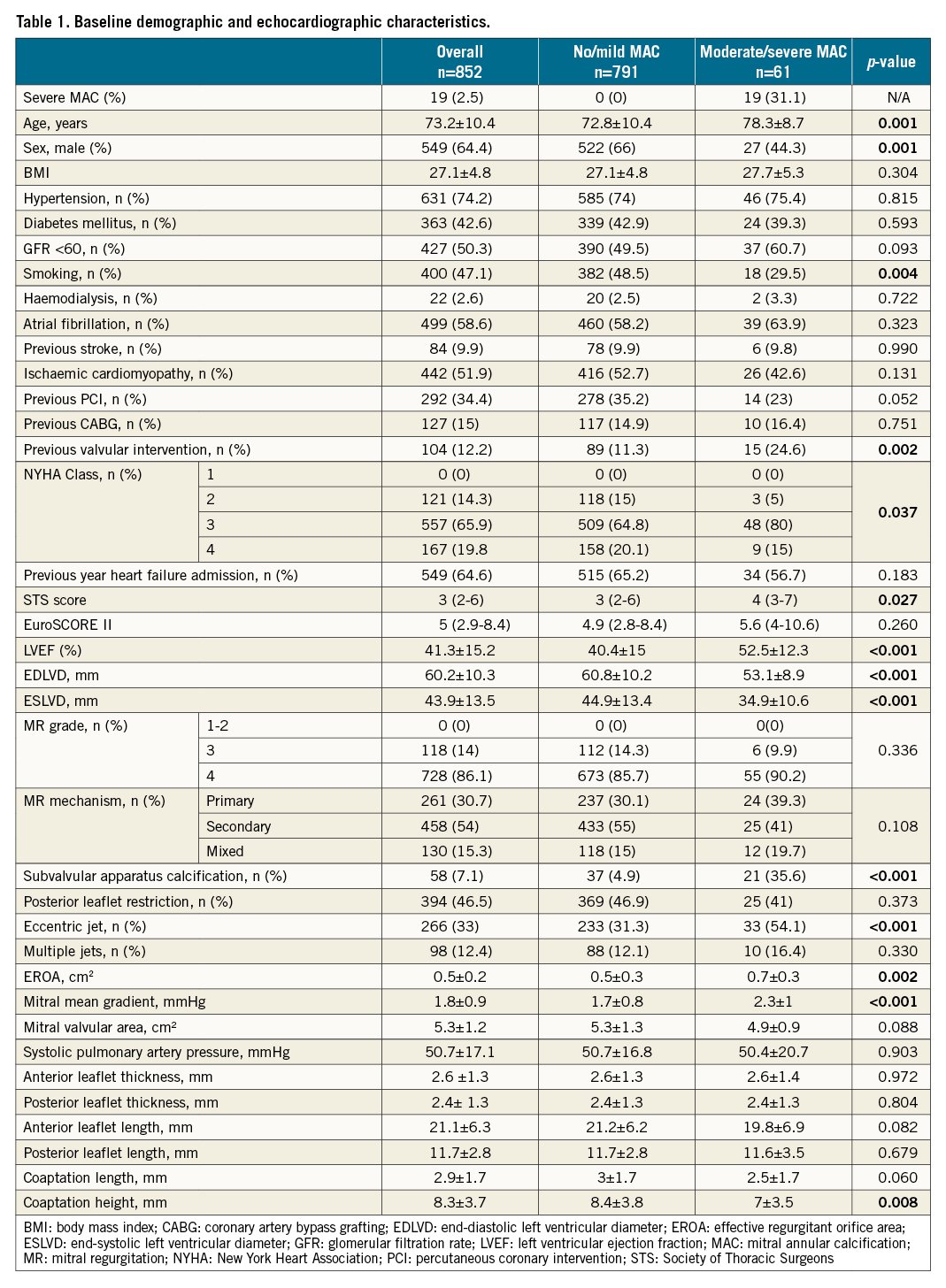
Echocardiographic analysis showed that MAC patients had smaller left ventricular diameters (end-diastolic left ventricular diameter [EDLVD] 53.1±8.9 vs 60.8±10.2 mm, p<0.001 and end-systolic left ventricular diameter [ESLVD] 34.9±10.6 vs 44.9±13.4 mm, p<0.001) and better LVEF (52.5±12.3 vs 40.4±15%, p<0.001). The mechanisms of MR were equally distributed between the groups (primary in 39.3% vs 30.1%, secondary in 41% vs 55%, and mixed in 19.7% vs 15.3% in the MAC and NoMAC groups, respectively). Most of the patients (90.2% of MAC patients and 85.7% of NoMAC patients) presented MR grade 4 at the time of repair, although the MAC group exhibited larger effective regurgitant orifice areas (EROAs) (0.7±0.3 vs 0.5±0.3 cm², p=0.002). MAC was mostly localised in the posterior annulus (77% of the patients) and, as expected, MAC patients had more challenging anatomies as they presented with greater subvalvular apparatus calcification (35.6% vs 4.9%, p<0.001), more eccentric jets (54.1% vs 31.3%, p<0.001), and higher baseline transvalvular gradients (2.3±1 vs 1.7±0.8 mmHg, p<0.001), compared to NoMAC patients.
Procedural outcomes and complexity
Procedural data are shown in Table 2. Procedural success was similar in both groups (technical success: 95.1% vs 98.1%, p=0.144; procedural success: 91.8% vs 95.1%, p=0.268, in the MAC and NoMAC groups, respectively) without differences in procedural duration (144±61 vs 135±66 min, p=0.327, MAC vs NoMAC, respectively). Residual gradient was higher in MAC patients (3.0 vs 3.6 mmHg, p=0.001) being greater than 5 mmHg in 18.5% of them, in comparison to 5% of NoMAC patients, p=0.001 (Figure 1A).
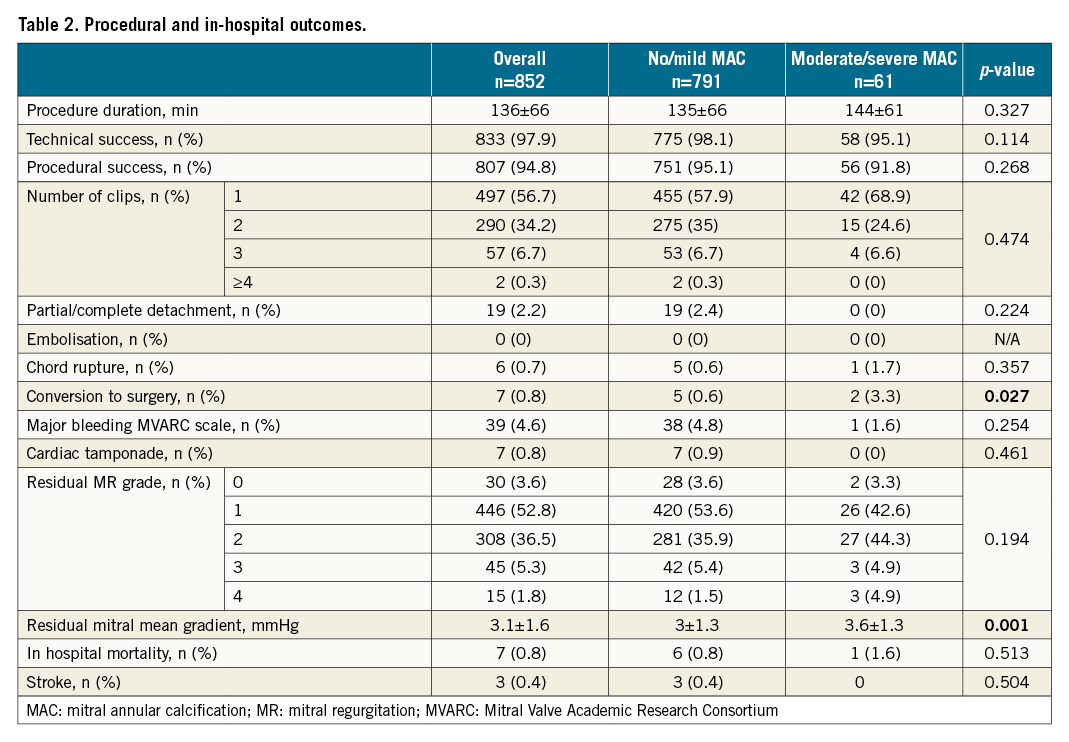
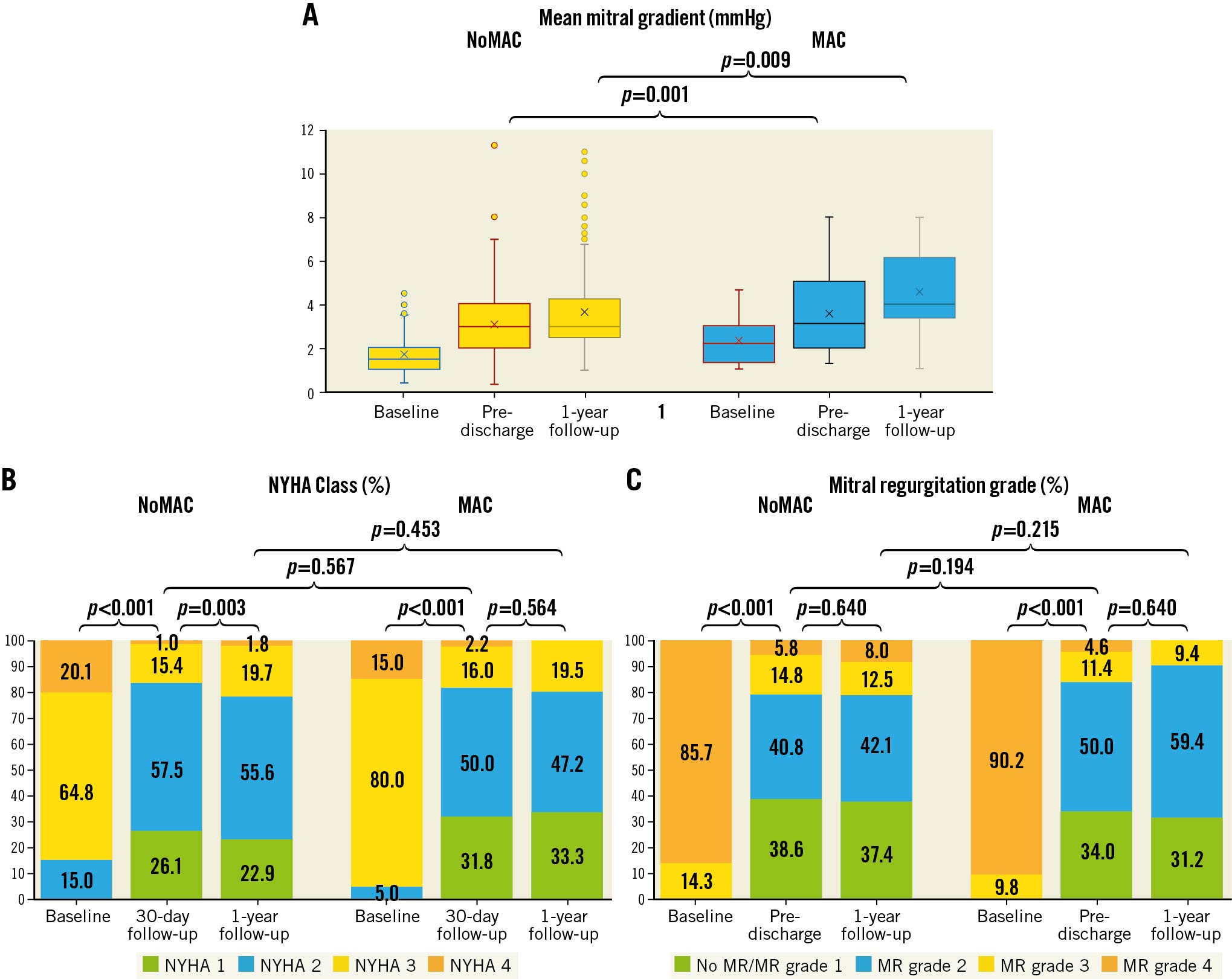
Figure 1. Haemodynamic and clinical follow-up. A) Changes over time in mean mitral gradient during follow-up according to mitral annulus calcification (MAC) grade. B) Changes over time in New York Heart Association (NYHA) Functional Class during follow-up according to MAC grade. C) Changes over time in mitral regurgitation (MR) grade during follow-up according to MAC grade.
Procedural complications were infrequent and occurred in 4 MAC patients and 70 NoMAC patients, mostly vascular access bleeding (p=0.549). Conversion to surgery during index hospitalisation occurred in 2 patients (3.28%) in the MAC group and 5 patients (0.63%) in the NoMAC group (p=0.027). Seven in-hospital deaths were reported, 1 in the MAC group, the others in the NoMAC group (p=0.513). Three strokes occurred during the index hospitalisation, all in the noMAC group (p=0.504).
Echocardiographic and clinical follow-up
Median follow-up was 455 days (204-916) in the MAC group and 385 days (160-726) in the NoMAC group. At 30 days, most patients had experienced an improvement in MR severity of at least one grade (93% in both groups, p=0.576), as well as an improvement in NYHA Functional Class of at least one grade (82% in both groups, p=0.567), most (~80%) being in NYHA Functional Class ≤II (p=0.692) (Figure 1B).
At one-year follow-up, 90.6% of MAC patients and 79.5% of NoMAC patients had residual MR grade 2 or less (p=0.129) (Figure 1C). A reduction in SPAP was observed in both groups; there were no significant changes in LVEF between baseline and one-year follow-up echocardiogram (Table 3). Mean gradient after clip implantation increased significantly in both groups between discharge and one-year follow-up (Table 3). There was no association at Cox analysis between preprocedural mitral valve area, MR grade or LVEF changes with the increase of mean gradient at follow-up (hazard ratio [HR] 0.8, 95% confidence interval [CI]: 0.2-4.2, p=0.802; HR 1, 95% CI: 0.9-1.1, p=0.787; HR 0.92, 95% CI: 0.6-1.5, p=0.745, respectively). Only 9 patients (1.14%), all in the NoMAC group (p=0.250), required reintervention during follow-up: 1 underwent a heart transplant, 2 had a mitral valve replacement, and 6 had a redo transcatheter mitral valve repair.
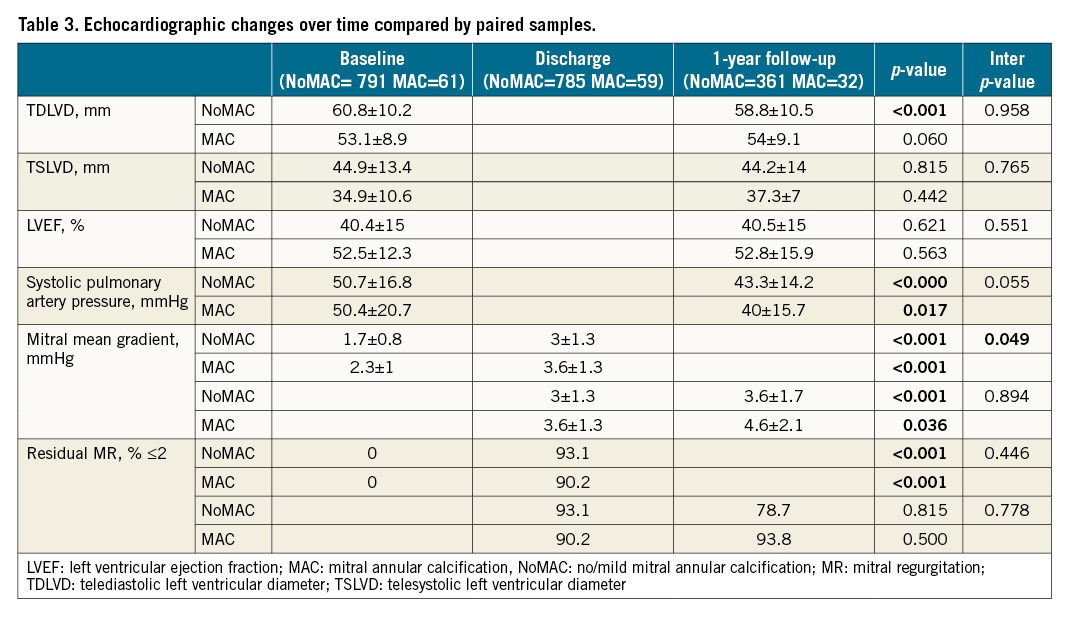
Clinically, patients remained in NYHA Functional Class II or less in 80.5% and 78.5% of MAC and NoMAC patients, respectively (p=0.453) (Figure 1B). Along with NYHA Class improvement, a global reduction in readmissions for heart failure within the year post MitraClip procedure was observed (21.3% vs 14.4%, p=0.145, for the MAC and NoMAC groups, respectively), translating into a reduction of almost 78% and 65%, respectively (p=0.145), as compared to the year before the procedure.
There were 11 patients in the MAC group for whom two years of follow-up data were available: 72.7% of them maintained an MR grade of 2 or less and an NYHA Class II or less. None of them required any additional mitral intervention during this period.
At one year, all-cause mortality was higher among MAC patients (19.7% vs 11.3%, p=0.050), with no differences in cardiovascular mortality (15.3% vs 9.2%, p=0.129). Of the 101 deaths within the first year of follow-up, 79 were cardiovascular and 22 were non-cardiovascular. Adjusted Cox model regression survival analysis showed that there was a marginal correlation of MAC with one-year all-cause mortality (HR 2, 95% CI: 0.9-4.3, p=0.070) but not with cardiovascular mortality (HR 2, 95% CI: 0.8-5.1, p=0.123) or unplanned cardiovascular readmission (HR 1.5, 95% CI: 0.8-3, p=0.210). Mean gradient of ≥5 mmHg at discharge was also not an independent predictor of all-cause or cardiovascular mortality (HR 2.1, 95% CI: 0.5-8.6, p=0.321, and HR 1.3, 95% CI: 0.5-3.2, p=0.624, respectively) or an independent predictor of unplanned cardiovascular rehospitalisation (HR 0.8, 95% CI: 0.31-2.00, p=0.633) in the MAC cohort.
As shown by Kaplan-Meier curves at one-year follow-up (Figure 2), there was a higher all-cause mortality risk in MAC patients (p=0.030) with no significant differences between groups in cardiovascular mortality (p=0.159) and rehospitalisation due to heart failure (p=0.115).
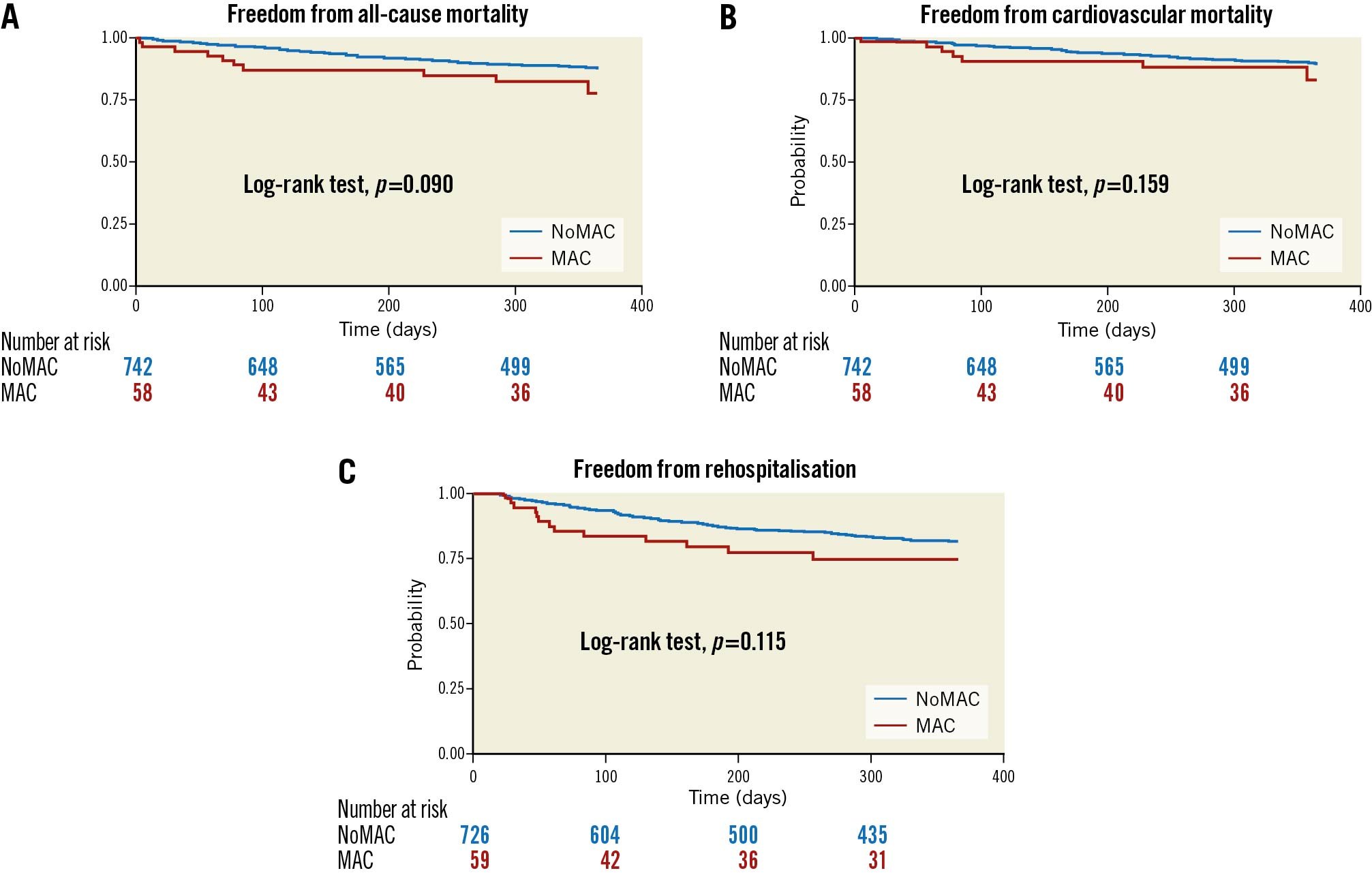
Figure 2. One-year survival curves for the composite event (A) all-cause mortality, (B) cardiovascular-related mortality, and (C) freedom from heart failure rehospitalisation, according to MAC grade.
Discussion
The main findings of this study are the following: 1) Transcatheter edge-to-edge repair with the MitraClip system in selected patients with moderate or severe MAC is comparable to patients without MAC in terms of feasibility, as demonstrated by the high technical success rate and the low incidence of procedural complications, despite a higher rate of conversion to surgery. 2) At one-year follow-up, the durability of the repair in selected patients with moderate or severe MAC is similar to that in those without MAC. 3) As expected, mean mitral gradients after MitraClip implantation were higher in MAC patients but it this did not imply significantly worse outcomes in terms of mortality or unplanned cardiac readmissions. 4) Patients with moderate or severe MAC also benefitted clinically from this procedure, as they experienced significant and sustained improvement in symptoms and no significant differences in cardiovascular mortality at one year (Central illustration).
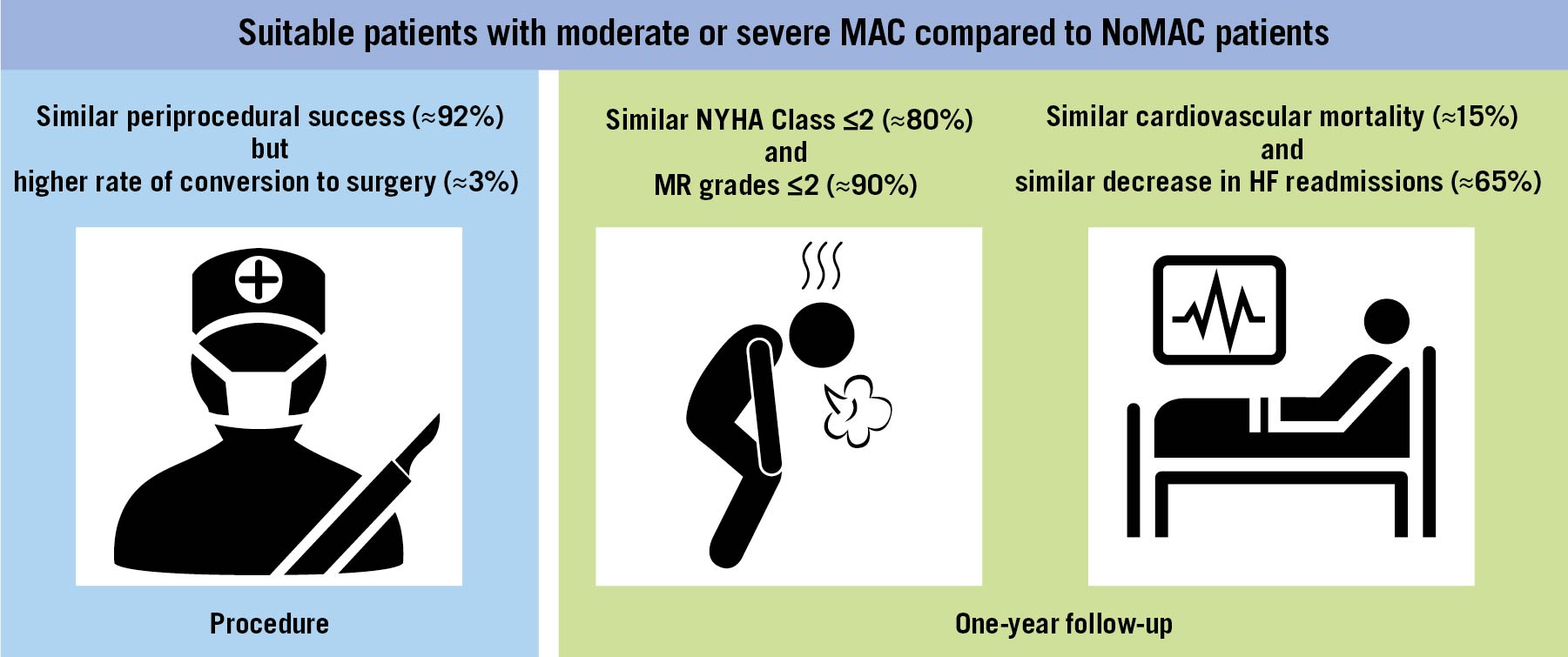
Central illustration. Transcatheter edge-to-edge mitral valve repair in patients with mitral annulus calcification.
Patients with severe MR and MAC represent a major surgical challenge as MAC implies complex surgery and a higher rate of post-operative complications and, in some series, repair failure101112131415161718. Therefore, a need for less invasive and yet efficient alternative therapies arises. The MitraClip system has become an effective alternative to open heart surgery for treating MR in high surgical risk patients20212223242526. However, even though MAC patients are often turned down for mitral valve surgery, they are also typically excluded from randomised clinical trials and from early feasibility studies with transcatheter mitral valve replacement therapies.
To date, only one single-centre study has assessed the safety of mitral valve repair with the MitraClip system in patients with MAC33. A total of 28 patients with moderate or severe MAC were assessed, showing high procedural success and similar improvements in MR grade and Functional Class, as compared to patients with no or mild MAC.
To date, the present study constitutes the largest multicentre experience conducted with the MitraClip device in patients with significant concomitant MAC and MR. In our study, from a cohort of 852 patients, 61 patients were found to have moderate or severe MAC on the preprocedural echocardiogram, 19 (31%) of whom had severe MAC. From a clinical standpoint, MAC patients were older and had a more advanced Functional Class. They also exhibited higher preprocedural transvalvular gradients along with larger EROAs despite there being no differences in mitral valve area, potentially implying a greater MR in this group. However, this could also reflect a different haemodynamic situation, as these patients have smaller ventricles with higher LVEFs. Of note, percutaneous repair was feasible in the vast majority of patients, with 98% technical success and 95% procedural success, in line with previous studies with the MitraClip device20212223242526. Only 5 patients with moderate or severe MAC had an unsuccessful procedure: 2 of them experienced a posterior leaflet tear and massive MR that led to emergent cardiac surgery, and for the remaining 3 patients, a reduction in MR grade ≤2+ could not be achieved. Both patients who experienced a posterior leaflet tear presented moderate MAC with no extension to the subvalvular apparatus, neither of them had a short or restrictive posterior leaflet, or calcified or thin leaflets. As for the 3 patients in whom an MR grade ≤2 could not be achieved, 2 of them presented severe MAC and subvalvular apparatus calcification and a preprocedural mitral gradient of 3 mmHg and only a final MR grade 3 could be obtained with a final post-procedural gradient of 6 and 4 mmHg, respectively. The third patient had moderate MAC with no extension to the subvalvular apparatus but had multiple jets. In that patient, finally no clip was implanted, as a satisfactory reduction of MR grade could not be achieved. Larger studies are needed to determine predictors of success in this population. However, the overall the results obtained in this study are encouraging considering that patients with MAC exhibited more complex anatomies (increased subvalvular apparatus calcification and more eccentric jets) and higher MR grades.
As expected, immediate post-procedural gradients were significantly higher in MAC patients: ≥5 mmHg in 18.5% of them but <8 mmHg in all cases. Nonetheless, even although a residual gradient ≥5 mmHg has been previously described as a potential predictor of worse clinical outcomes, in our cohort it was not independently associated with an increase in all-cause or cardiovascular mortality or unplanned cardiac readmissions at follow-up, in line with the results obtained in the COAPT trial3435 (see also R. Halaby, Lack of association of mitral valve gradient after MitraClip with outcomes in functional mitral regurgitation: results from the COAPT trial. Presented at ACC.20 World Congress of Cardiology Virtual, March 29, 2020). The mean gradient after clip implantation also increased significantly in both groups between discharge and one-year follow-up (Table 3). There are some possible explanations for this, e.g., improvement in LVEF or decrease in mitral valve area, but none of them could be proven in our cohort as we found no association at Cox analysis between the former variables and mean gradient at follow-up.
Importantly, in the MAC group, there were no cases of clip detachment, embolisation or stroke, and only one in-hospital death. However, there was a higher conversion to cardiac surgery (3.28%) during index hospitalisation than in the NoMAC group due, in the two patients that experienced this complication, to posterior leaflet tear that led to massive MR. Nonetheless, overall these results are remarkable considering the relatively higher periprocedural mortality rates observed in the early experience with transcatheter mitral valve replacement (up to 14% vs 1.6% in the MAC group of the present study), which may be considered as another interesting alternative in the presence of moderate or severe MAC and risk of left ventricular outflow tract obstruction36373839.
Repair durability in this setting might have been considered an important concern. This is based on the absence of long-term durability data for transcatheter mitral valve repair in such patients and also on the basis of an unfavourable surgical predicate with the Alfieri technique in this setting, which resulted in higher gradients, reduced durability and increased need for reoperation27. Nonetheless, in our study, transcatheter mitral repair with the MitraClip device in MAC patients resulted in sustained clinical and echocardiographic improvements at one-year follow-up, with 80% of patients remaining at NYHA Functional Class I-II and with a residual MR ≤2 in 91% of MAC patients. Importantly, no reintervention was required in those patients within the first year after the MitraClip procedure (0% in the MAC group, 1.1% in the NoMAC group).
Overall, these findings translated into a substantial reduction in the number of heart failure-related rehospitalisations following the procedure, as compared to the number of admissions of these patients the year before the MitraClip procedure was performed, similar to the benefit observed in patients without MAC. This clinical and echocardiographic benefit was also maintained in the 11 MAC patients for whom two years of follow-up data were available: an NYHA Class I or II was still observed in 72.7% of them along with an MR grade of 2 or less in 72.7%, without any additional mitral intervention during this period. These results reinforce the potential use of transcatheter edge-to-edge repair to treat symptomatic patients with high grade MR at increased surgical risk and severely calcified mitral valve annulus, in the absence of significant mitral stenosis or leaflet calcification.
There was a marginal correlation of all-cause mortality with MAC patients, even though MAC was not found to be an independent predictor for all-cause or cardiovascular mortality at one year. It is noteworthy that MAC patients are often elderly, with increased morbidity, mortality and cardiovascular disease, often making them ineligible for open heart surgery due to pre-existing comorbidities or technical reasons (high calcium burden). Hence, this association is probably due to a higher comorbidity burden in these patients, rather than the procedure itself, which carried a low rate (<2%) of in-hospital mortality.
Overall, use of the MitraClip device in patients with significant annular calcification resulted in significant clinical improvement with durable reduction of MR at one year. Our results highlight the safety and efficacy as well as the one-year durability of transcatheter edge-to-edge repair in patients with MAC. This constitutes a reasonable alternative to surgery in this subgroup of patients and may probably be considered the first choice therapy in patients ineligible for surgery and with favourable anatomy for percutaneous edge-to-edge repair.
Limitations
Our study had several limitations. First, it was a retrospective observational multicentre study which has limitations inherent to its nature. In addition, the grading of MAC was qualitative and based on echocardiography, with no centralised core laboratory adjudication of echocardiographic data or clinical events. Second, medical treatment before and after the procedure was not systematically recorded and may have influenced post-operative outcomes. Finally, the study population was limited to one specific type of transcatheter edge-to-edge repair device (MitraClip); therefore, the results may not be generalisable to other edge-to-edge therapies. Of note, the study was conducted in a highly selected MAC population and the procedures were performed in highly experienced centres. Thus, further research is required before generalising these results.
Conclusions
Percutaneous repair with the MitraClip system in patients with significant MAC and high surgical risk is safe and feasible, with sustained improvement in NYHA functional class and MR reduction at one year in the vast majority of patients (~80%). These results suggest that percutaneous edge-to-edge repair may be considered as a valid alternative to surgery in selected patients with severe MR and MAC, in the absence of significant mitral stenosis or leaflet calcification. Further evaluation in larger-scale trials is required to determine predictors of procedural success and long-term outcomes in MAC patients treated with the MitraClip system.
Impact on daily practice
MAC is a condition commonly found in patients affected with severe MR that is associated with a high morbidity and mortality and worse surgical outcomes. Therefore, the need for a less invasive and yet efficient alternative to surgery arises in this setting. In this study, transcatheter edge-to-edge repair with the MitraClip system in selected patients with moderate or severe MAC was found to be a safe and feasible alternative that achieved a significant reduction of MR grade and a substantial clinical improvement at one-year follow-up. Thus, MitraClip implantation emerges as a valid therapeutic option in this population, even though larger studies are needed in order to determine predictors of good clinical outcomes.
Conflict of interest statement
R.D. Estevez-Loureiro, L. Nombela-Franco, L. Sanchis, C-H. Li and D. Arzamendi have served as proctors for Abbott Vascular. X. Freixa, R. Estévez-Loureiro, and L. Nombela-Franco are consultants for Abbott Vascular and have received personal fees from Abbott. C-H. Li has received personal fees from Abbott. All other authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Supplementary data
To read the full content of this article, please download the PDF.