Abstract
Aims: Mitral annular calcification (MAC) negatively influences outcomes in surgical mitral valve (MV) repair for mitral regurgitation (MR). However, there are no data on whether MAC impacts on outcomes of MitraClip percutaneous MV edge-to-edge repair. This study sought to investigate whether the presence of MAC impacts on the procedural success and durability of percutaneous transcatheter repair of MR using the MitraClip.
Methods and results: One hundred and seventy-three patients undergoing MitraClip repair for significant MR were studied. Patients with moderate-or-severe MAC (n=28) were compared to those with no-or-mild MAC. Post-procedural MR severity was not different (p=0.642) and MR reduction to moderate-or-less was equally high in patients with moderate-or-severe MAC (100%) and those without (96.7%), p=1.000. At one year, MR severity was not different (p=0.831), and there was no difference in the repair durability when comparing patients with moderate-or-severe MAC (93.8%) to those without (90.6%), p=1.000. All patients with moderate-or-severe MAC assessed at one year were in NYHA functional Class I-II and had haemodynamic improvements with a decrease in pulmonary artery systolic pressure (-6.5±13.1 mmHg), p=0.021, and end-diastolic left ventricular internal diameter (-3.9±6.5 mm), p=0.034, not different to those achieved by patients without MAC (both p>0.100).
Conclusions: Moderate-or-severe MAC scored by echocardiography and confirmed on fluoroscopy was not associated with decreased procedural success or durability of repair. Patients with moderate-or-severe MAC had improvements in clinical symptoms and haemodynamics, as well as decreased left ventricular dimensions.
Introduction
Mitral annular calcification (MAC) is a degenerative process affecting the fibrous annulus of the mitral valve (MV) and is often associated with mitral regurgitation (MR)1. MAC is commonly found in patients referred for MV surgery and is associated with an increased intraoperative conversion from valve repair to replacement and negatively influences surgical outcomes2. In high surgical risk patients with significant MR, percutaneous edge-to-edge repair with the MitraClip® (Abbott Vascular, Santa Clara, CA, USA) has emerged as an alternative corrective therapy which results in significantly reduced MR, improvement of clinical symptoms, haemodynamics3, and left ventricular function and decreased left ventricular (LV) dimensions4,5. However, it is not known whether MAC impacts on procedural success, durability of repair, and clinical and echocardiographic outcomes in percutaneous edge-to-edge repair of MR.
The development and acceleration in the severity of MAC has been hypothesised to be due to increased MV annular stress from increased afterload conditions such as from elevated systemic blood pressure and outflow track obstruction, leading to increased closing pressure and excess annular tension and resulting annulus degeneration6. MAC is also associated with coronary artery disease (CAD)7, significant chronic kidney disease and haemodialysis8,9, as well as age, female gender, hypertension, and diabetes mellitus10,11. MAC is also associated with increased rates of cardiovascular events and excess mortality12.
MAC is most frequently identified by echocardiography. Multiple studies have utilised echocardiographic scoring systems to classify the severity of MAC9,12,13. Grading is carried out based on the degree of involvement of the mitral posterior annulus. MAC has been classified as mild when it involves less than one third of the annulus, moderate when it involves one third to two thirds of the annulus, and severe when it involves more than two thirds of the annulus9,13,14.
In patients with significant MV disease with concomitant MAC undergoing surgery, the preferred surgical approach is the complete decalcification of MAC and reconstruction of the mitral annulus15,16. This process leads to increased operating time, a significant risk of cardiac rupture and injury to the circumflex artery15,16, and an increased conversion from valve repair to replacement, all of which negatively influences surgical outcomes2. If MV replacement is attempted without annular decalcification, there is increased difficulty with securing the prosthetic valve inside a calcified annulus and a greater potential for periprosthetic leak and inadequate prosthetic valve sizing16. As surgery for MV disease with significant MAC can be challenging, there remains a clinical need for an alternative approach for this clinical situation.
This study sought to investigate whether the presence of MAC without significant leaflet calcification impacts on the procedural success and durability of percutaneous transcatheter repair using the MitraClip.
Methods
Patients who underwent MitraClip therapy between April 2009 and May 2014 were included in the analysis. Patients were divided into two groups based on having no-or-mild MAC versus moderate-or-severe MAC. The grading of MAC severity was performed on baseline pre-procedure transthoracic echocardiogram by two authors independently, disagreements being scored by consensus. Standard criteria were used to define MAC as mild if annular calcification involved one third or less of the posterior annulus, moderate if it involved one third to two thirds of the posterior annulus, and severe if it involved over two thirds of the posterior annulus9,13,14. Subsequently, fluoroscopy was used to confirm the presence of MAC. In cases of significant discrepancy, fluoroscopy was used to relabel patients with mild MAC on echocardiography to moderate-or-severe MAC if significant radiographic MAC was found, and to relabel patients with moderate-or-severe MAC on echocardiography to no-or-mild if no fluoroscopic MAC was found. The number of patients relabelled is reported. The severity and aetiology of MR were assessed by transthoracic and transoesophageal echocardiography by site echo physicians using a multiparametric approach to grade MR as described by the Mitral Valve Academic Research Consortium consensus and by standard American Society of Echocardiography guidelines17,18.
BASELINE DEMOGRAPHICS AND ECHOCARDIOGRAPHIC PARAMETERS
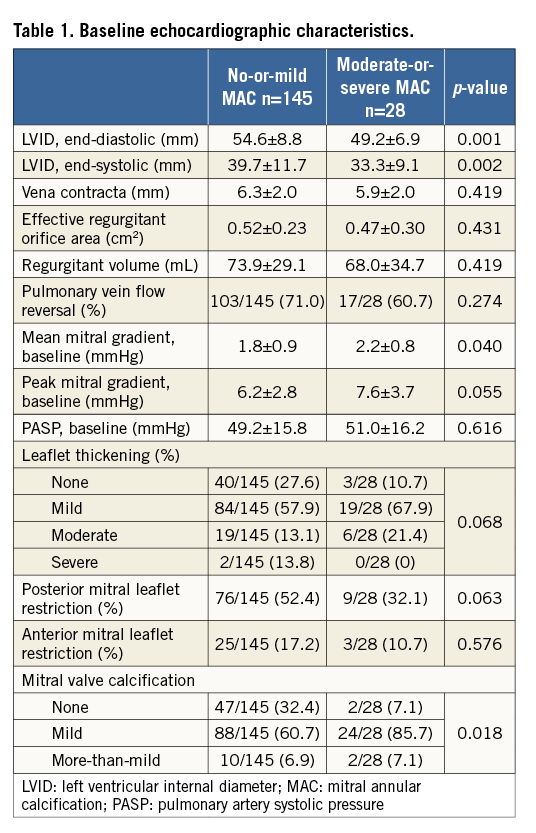
Baseline demographic parameters compared between patients with no-or-mild MAC versus moderate-or-severe MAC included age, female gender, MR severity, chronic heart failure, CAD, myocardial infarction, atrial fibrillation, hypertension, diabetes, hyperlipidaemia, haemodialysis, creatinine, New York Heart Association (NYHA) functional class, Society of Thoracic Surgeons (STS) score, and left ventricular ejection fraction (LVEF). Additional baseline echocardiographic characteristics included are listed in Table 1. Severity of leaflet thickening, restriction, and calcification are graded based on a previously validated scoring system9,13.
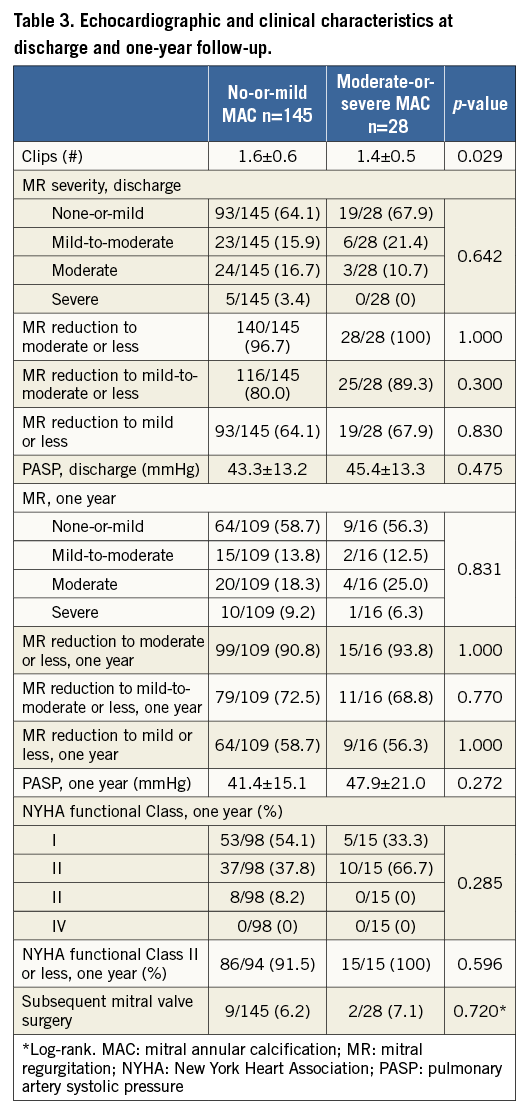
PROCEDURAL SUCCESS AND ECHOCARDIOGRAPHIC AND CLINICAL CHARACTERISTICS AT DISCHARGE AND ONE-YEAR FOLLOW-UP
Procedural success defined as MR reduction to moderate or less, mild-to-moderate or less, and mild or less was reported and compared between patients with and without moderate-or-severe MAC. In addition, pulmonary artery systolic pressure (PASP) at discharge, severity of MR at one year, PASP at one year, NYHA functional class at one year, and subsequent MV surgery were compared between groups.
DURABILITY OF PERCUTANEOUS REPAIR
Durability of repair was defined as successful retention of procedural success on the one-year post-MitraClip repair follow-up transthoracic echocardiogram. In patients who achieved MR reduction to moderate or less (≤2+), persistence of MR reduction of moderate or less at one year was reported and compared between groups. Retention of the same level or better MR reduction for patients who obtained initial MR reduction mild-to-moderate or less, and mild or less is also reported and compared between groups.
CHANGES IN ECHOCARDIOGRAPHIC CHARACTERISTICS AS COMPARED BY PAIRED SAMPLES
End-diastolic left ventricular internal diameter (LVID), end-systolic LVID, ejection fraction, and PASP were compared at the time of baseline transthoracic echocardiogram and at one-year echocardiogram. In addition, PASP was compared at the time of baseline echocardiogram and at post-procedure discharge echocardiogram.
MITRAL ANNULAR CALCIFICATION AND SURVIVAL AFTER PERCUTANEOUS REPAIR
Cox proportional hazards regression for the presence of moderate-or-severe MAC on all-cause mortality is reported. In addition, a multivariate modelling was performed to include pre-specified variables previously reported to be associated with MAC (age, female gender, CAD, hypertension, diabetes, and haemodialysis status), as well as demographic and baseline characteristics that were different between patients with moderate-or-severe MAC and no-or-mild MAC (when p>0.100).
STATISTICAL ANALYSIS
Statistical analysis was performed with SPSS, Version 22 (IBM Corp., Armonk, NY, USA). Fisher’s exact test was used for two-by-two categorical variables, a two-tailed Student’s t-test was used for continuous variables, and a paired samples t-test was used for paired analysis of continuous variables. The Mann-Whitney U test was used for non-parametric variables, and the paired samples Wilcoxon signed-rank test was used for paired analysis of non-parametric variables. The study was approved by our institutional review board.
Results
One hundred and seventy-three patients were included in the analysis and mean clinical follow-up was 29.2±20.4 months; 6/173 (3.5%) patients were followed by their referring physician, and the remaining patients had at least one-year follow-up in the clinic unless the patient was no longer alive. Mean age at percutaneous repair was 77.1±12.5 years and 71/173 (41.0%) were female. MAC was present in 82/173 (47.4%) patients: mild in 54/82 (65.9%) cases, moderate in 18/82 (22.0%) cases, and severe in 10/82 (12.2%) cases. Five patients with mild MAC on echocardiography were found to have significant MAC on fluoroscopy and were relabelled as having moderate-or-severe MAC. Three patients with moderate MAC on echocardiography were found to have no-or-trivial MAC on fluoroscopy and were relabelled as having no-or-mild MAC. No patients with no MAC on echocardiography were found to have significant MAC on fluoroscopy, and no patients with severe MAC on echocardiography were found to have no-or-trivial MAC on fluoroscopy. Examples of patients who were relabelled are illustrated in Figure 1. Fluoroscopic examples of mild, moderate, and severe MAC are illustrated in Figure 2.
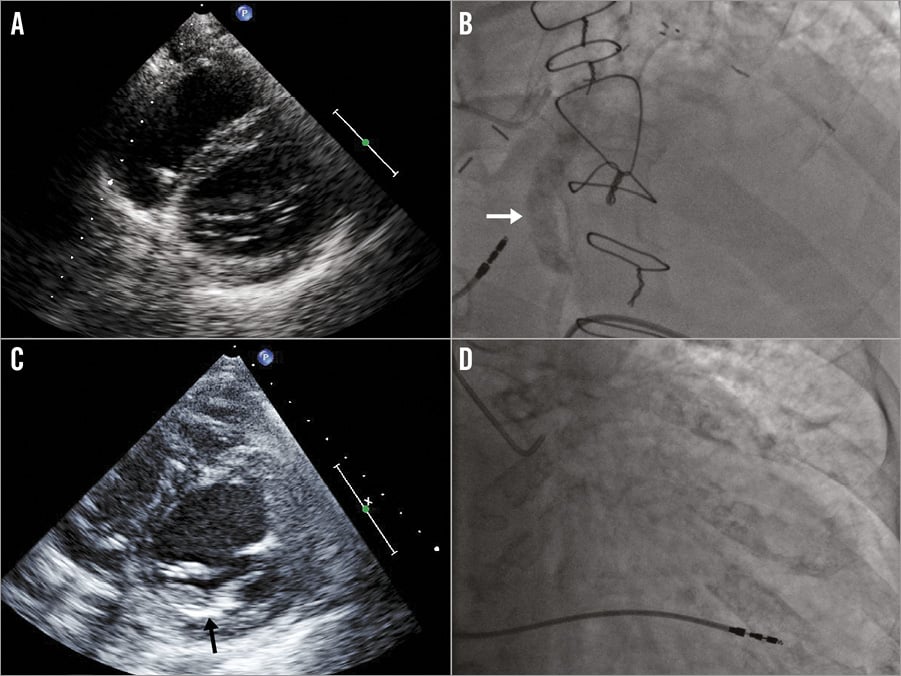
Figure 1. Transthoracic echocardiographic and fluoroscopic examples of patients relabelled after confirmation fluoroscopy. Case example 1. An 89-year-old male with moderate-to-severe mitral regurgitation and prolapse of the posterior leaflet with no mitral annular calcification (MAC) on parasternal short-axis view at the level of the mitral valve (A) relabelled as having moderate-to-severe MAC when confirmation fluoroscopy (B) showed significant MAC (arrow) in a right anterior oblique cranial view. Case example 2. An 84-year-old female with severe central mitral regurgitation and restriction of the posterior leaflet with moderate MAC (arrow) on parasternal short-axis view at the level of the mitral valve (C) relabelled as having no-to-mild MAC when confirmation fluoroscopy (D) did not show the presence of significant MAC in a right anterior oblique caudal view.
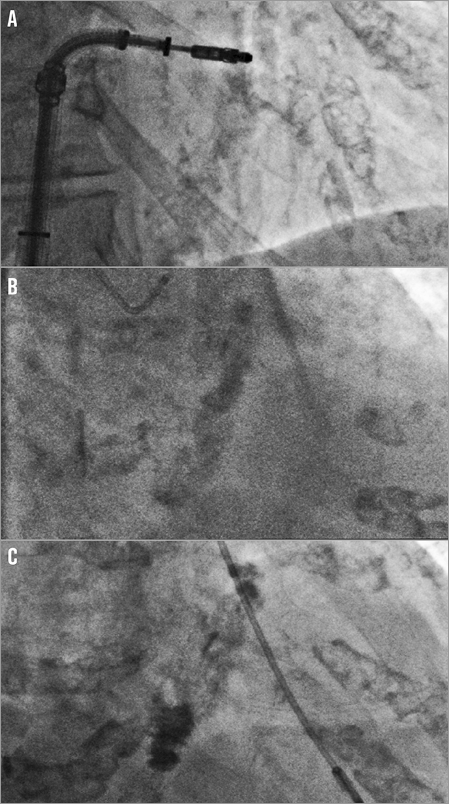
Figure 2. Fluoroscopic scoring of mitral annular calcification. Fluoroscopic examples of mild (A), moderate (B), and severe (C) mitral annular calcification.
DEMOGRAPHIC, BASELINE, AND ECHOCARDIOGRAPHIC CHARACTERISTICS
Patients with moderate-or-severe MAC were older than patients without (84.2±8.1 vs. 75.7±12.8, p<0.001), more likely to be female (60.7% vs. 37.2%, p=0.034), and with a history of hypertension (100% vs. 76.7%, p=0.002). The distribution of NYHA functional class was more severe in patients with moderate-or-severe MAC (Mann-Whitney p=0.043) as was severity of STS score (13.2±7.3% vs. 10.1±8.0%, p=0.048). However, LVEF was higher (59.9±12.8 vs. 49.4±18.1%, p=0.001). The proportion of degenerative and functional MR was not different between the groups (p>0.010). Myxomatous degeneration or Barlow’s disease occurred in 5/173 (2.9%) patients. Demographic and baseline characteristics are summarised in Table 2.
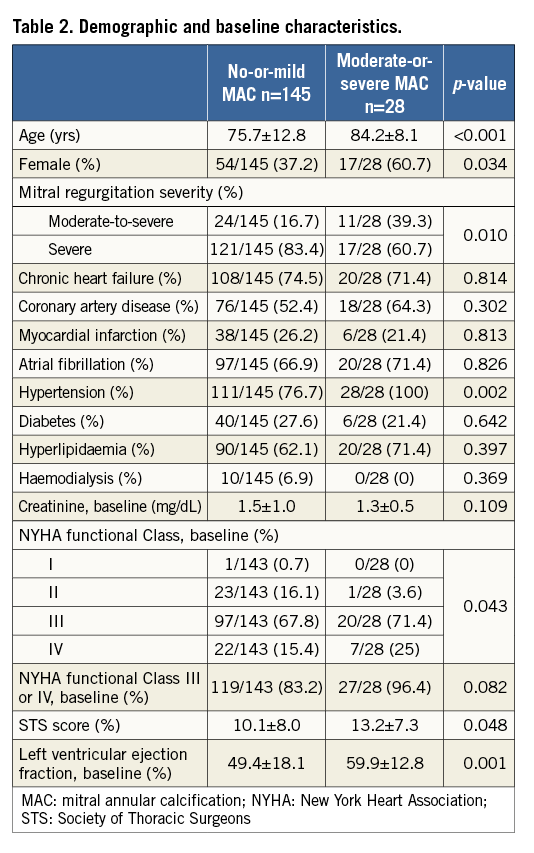
Patients with moderate-or-severe MAC had smaller end-diastolic LVID (49.2±6.9 vs. 54.6±8.8 mm, p=0.001) and end-systolic LVID (33.3±9.1 vs. 39.7±11.7 mm, p=0.002), and a marginally higher mean mitral gradient (2.2±0.8 vs. 1.8±0.9 mmHg, p=0.040). Severity of MR by vena contracta, effective regurgitant orifice area, regurgitant volume, and pulmonary vein systolic flow reversal was not different between the groups (all p>0.100). MV calcification was more severe in patients with moderate-or-severe MAC (Mann-Whitney p=0.018) but overall was low in the entire cohort (none-or-mild 93.1%). There was a trend towards increased leaflet thickening in patients with moderate-or-severe MAC (Mann-Whitney p=0.068) but overall was low in the entire cohort (none-or-mild 84.4%). Baseline echocardiographic characteristics are summarised in Table 1.
PROCEDURAL SUCCESS AND ECHOCARDIOGRAPHIC AND CLINICAL CHARACTERISTICS AT DISCHARGE AND ONE-YEAR FOLLOW-UP
MR reduction to moderate or less occurred in 168/173 patients (97.1%), mild-to-moderate or less in 141/173 patients (81.5%), and mild or less in 112/173 patients (64.7%). Patients with moderate-or-severe MAC were equally likely to have procedural success as compared with patients with no-or-mild MAC with regard to distribution of MR severity (Mann-Whitney p=0.642), MR reduction to moderate or less (100% vs. 96.7%, p=1.000), MR reduction to mild-to-moderate or less (89.3% vs. 80.0% p=0.300), and MR reduction to mild or less (67.9% vs. 64.1% p=0.830).
At one year, MR reduction to moderate or less was present in 114/125 patients (91.2%), mild-to-moderate or less in 90/125 patients (72.0%), and mild or less in 73/125 patients (58.4%). There was no difference in MR severity at one year between patients with moderate-or-severe MAC and patients without (Mann-Whitney p=0.831). PASP at discharge and one year was decreased as compared with pre-procedural PASP (both p<0.05), and NYHA functional class at one year, and subsequent MV surgery (Figure 3) were not different between the groups. Results of echocardiographic and clinical characteristics at discharge and one-year follow-up are summarised in Table 3.
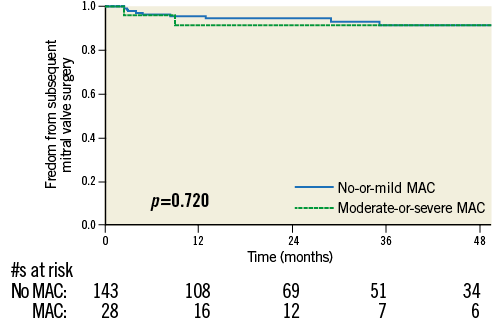
Figure 3. Freedom from subsequent mitral valve surgery. Overall freedom from subsequent mitral valve surgery at 4 years was 91.2±2.7% and did not differ between patients with or without moderate-or-severe mitral annular calcification (MAC) (p=0.720).
DURABILITY OF PERCUTANEOUS REPAIR
In patients with MR reduction to moderate after the procedure, 111/122 (91.0%) retained a reduction of moderate or less at one year. There was no difference in retention of MR reduction between patients with moderate-or-severe MAC (15/16; 93.8%) as compared with patients with no-or-mild MAC (96/106; 90.6%, p=1.000). In patients with MR reduction to mild-or-moderate or less, 81/104 (77.9%) retained a reduction of mild-or-moderate or less at one year. There was no difference in retention of MR reduction between patients with moderate-or-severe MAC (11/15; 73.3%) as compared with patients with no-or-mild MAC (70/89; 78.7%, p=0.738). In patients with MR reduction to mild or less, 58/86 (67.4%) retained a reduction of mild or less at one year. There was no difference in retention of MR reduction between patients with moderate-or-severe MAC (7/12; 58.3%) as compared with patients with no-or-mild MAC (51/74; 68.9%, p=0.515). The distribution of MR severity in 125 patients who had complete baseline, discharge, and one-year echocardiograms is illustrated in Figure 4.
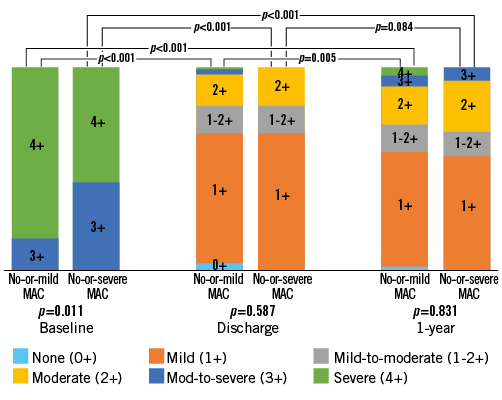
Figure 4. Distribution of severity of mitral regurgitation at baseline, discharge, and follow-up. Patients are divided by the presence of no-or-mild mitral annular calcification (MAC) and moderate-or-severe MAC at time of baseline echocardiogram with fluoroscopic confirmation. Mann-Whitney U test was used to compare between groups at each time point, and a paired samples Wilcoxon signed-rank test was used to compare within each group across time points.
CHANGES IN ECHOCARDIOGRAPHIC CHARACTERISTICS AS COMPARED BY PAIRED SAMPLES
End-diastolic LVID decreased between baseline and one year both in patients with moderate-or-severe MAC (–3.9±6.5 mm, paired samples p=0.034) and in patients with no-or-mild MAC (–1.4±6.7 mm, p=0.039). PASP decreased between baseline and discharge both in patients with moderate-or-severe MAC (–6.5±13.1 mmHg, p=0.021) and in patients with no-or-mild MAC (–6.5±15.5 mmHg, p<0.001). End-systolic LVID nominally decreased between baseline and one year in patients with moderate-or-severe MAC (-1.6±7.7 mm) but did not reach significance (p>0.05). The results of paired samples analysis including changes in mean mitral gradient are summarised in Table 4 and Figure 5.
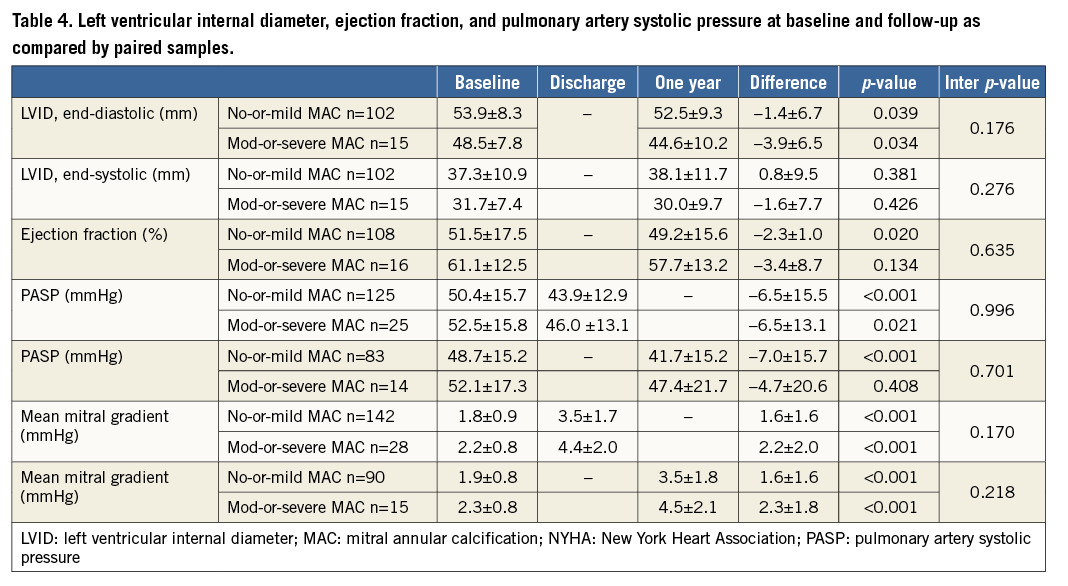
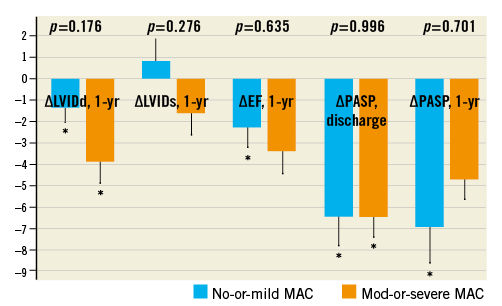
Figure 5. Changes in end-diastolic left ventricular internal diameter, end-systolic left ventricular internal diameter, ejection fraction, and pulmonary artery systolic pressure. Standard error bars, and p-values of between group comparisons are illustrated. Asterisks (*) indicate that the change was statistically significant as compared by paired samples between the stated time points (p<0.05).
MITRAL ANNULAR CALCIFICATION AND SURVIVAL AFTER PERCUTANEOUS REPAIR
By univariate Cox proportional hazards regression, the presence of moderate-or-severe MAC was not associated with all-cause mortality (hazard ratio [HR] 1.280, 95% CI: 0.688-2.380, p=0.436). In a multivariate model that included pre-specified demographic and baseline characteristics of age, female gender, CAD, hypertension, diabetes, and haemodialysis status, as well as the additional variables of MR severity, baseline NYHA functional class, STS score, and LVEF (as these variables were different between the two groups, p<0.100), the presence of moderate-or-severe MAC remained not associated with all-cause mortality (HR 1.121, 95% CI: 0.552-2.275, p=0.753). In this model, NYHA functional Class III or IV was associated with mortality (HR 5.835, 95% CI: 1.287-26.458, p=0.022). Both female gender (HR 0.605, 95% CI: 0.350-1.046, p=0.072) and STS score per 1% (HR 1.037, 95% CI; 0.998-1.077, p=0.063) trended towards an association with all-cause mortality. The hazard ratio for age per one year was 1.017 (95% CI: 0.984-1.052, p=0.311).
Discussion
MAC is commonly found in patients referred for MV surgery for repair of significant MR and is associated with an increased intraoperative conversion from valve repair to replacement and negatively influences surgical outcomes2,19. However, our study demonstrates a high procedural success rate and durability of MR reduction in patients who underwent percutaneous MitraClip repair in the presence of MAC without severe leaflet calcification. Excellent surgical results can be obtained in experienced centres for MV surgery even in the presence of MAC; however, in patients with prohibitively high surgical risk from comorbidities and older age, the MitraClip procedure offers an alternative option for repair. Significant MAC as scored by transthoracic echocardiography and confirmed by fluoroscopy was associated with equally high MR reduction and durability of repair which was not affected by the presence or severity of MAC. Moreover, patients with or without significant MAC had decreases in LV dimensions, PASP, and improvements in NYHA functional class.
The overall age of patients included in the study is over a decade older than the typical age reported for patients undergoing MV surgery2, and represents a high surgical risk cohort. Patients with moderate-or-severe MAC were nearly a decade older than patients with no-or-mild MAC with higher STS scores. While LVEF was lower in patients with no-or-mild MAC, patients with moderate-or-severe MAC were more limited as assessed by NYHA functional class. Echocardiographic measures of MR severity vis-à-vis vena contracta width, effective regurgitant orifice area, regurgitant volume, and prevalence of pulmonary vein flow reversal were not different between patients with moderate-or-severe MAC and those without. Interestingly, despite the association of haemodialysis with MAC8,9, patients on haemodialysis in our cohort had either no MAC (2.9%) or mild MAC (2.9%), which may be due to random chance given the overall low incidence of haemodialysis in the entire cohort (10/173; 5.8%), non-significant p-value=0.369. In these patients, median time on haemodialysis was only five months (IQR 19.5 months), with 7/9 (77.8%) on haemodialysis for a short time (<13 months).
Procedural success and durability of repair were similarly high in patients with or without moderate-or-severe MAC, and moderate-or-less MR was achieved in >95% of patients. Durability of repair at one year as well as NYHA functional Class I-II at one year were achieved in >90% of patients. The need for subsequent MV surgery was uncommon (6.4%, 2.4-year mean follow-up), and occurred equally frequently in patients with moderate-or-severe MAC and in those without (p=0.720). While annular decalcification and reconstruction are needed for optimal surgical repair16,20,21, favourable LV remodelling occurs in percutaneous repair4, a phenomenon we observed in patients with significant MAC as well. In paired samples analysis of echocardiographic parameters, both patients with moderate-or-severe MAC and those without had decreases in PASP and LV dimensions. We found no differences in the success rate, durability, or clinical and echocardiographic outcomes of percutaneous repair of MR for patients with or without significant MAC. These results are in contrast to previous reports of surgical edge-to-edge mitral repair, in which patients with annular calcification had significantly greater reoperation rates (77±22%) than those patients without annular calcification (95±4.6%), p=0.0320. The stark differences in results between surgical repair and MitraClip repair may be due to careful case selection in the latter case, with avoidance of patients with severe leaflet calcification.
The results of our study support the feasibility and midterm durability of repair using the MitraClip device for carefully selected MR patients with significant MAC and without severe leaflet calcification. There are alternatives under investigation including the transcatheter implantation of valves originally designed for placement in the aortic position in the native MV anchored by MAC22, an approach that would be specifically suitable where there is severe extension of calcification onto the leaflets. Moreover, a plethora of percutaneous transcatheter MV replacement devices designed for placement in the native MV is emerging23. However, the procedural success and long-term durability data of these novel devices are lacking. In the absence of those data, our study confirms that the MitraClip is a safe and effective option for patients with MR and significant MAC.
Limitations
This was a single-centre retrospective study. The large experience in our single site helped in the uniformity of assessment and care of the patients. However, the number of patients with severe MAC in this series is small. As such, the potential complications with percutaneous repair in patients with MAC have not been fully elucidated by this series. Further studies are warranted to investigate the incidence of complications, such as leaflet rupture, in this patient cohort. Myxomatous degeneration or Barlow’s disease with bulky billowing leaflets and multi-segmental prolapse was present only in 2.9% of the cohort and our findings may not be generalisable to these patients due to their small numbers. The grading of MAC was qualitative and not quantitative, as performed by computed tomography Agatston score; nonetheless, our data are clinically applicable to patients undergoing the MitraClip procedure. The echocardiographic data and clinical data were analysed by the local site without confirmation from an independent core lab or adjudication of clinical data by an independent monitor.
Conclusions
Our study demonstrates the safety, feasibility, and midterm durability of the MitraClip in the treatment of MR in patients with significant MAC but without severe leaflet calcification or thickening. Patients with moderate-or-severe MAC had demonstrable improvements in clinical symptoms and decreased left ventricular dimensions.
| Impact on daily practice Mitral annular calcification (MAC) is commonly found in patients referred for surgical repair of mitral regurgitation (MR) but is associated with increased intraoperative conversion from repair to replacement and worse outcomes, in part due to the need for decalcification and reconstruction of the mitral annulus. Data about its impact on pecutaneous MR repair are lacking. This study demonstrates that significant MAC was not associated with decreased procedural success or durability of repair with the MitraClip device. Percutaneous MV repair, therefore, provides a therapeutic option for patients with significant concomitant MAC and MR, with similar and demonstrable improvements in clinical symptoms, haemodynamics, and left ventricular dimensions as those found for patients without significant MAC. |
Funding
There were no sources of support for the research.
Conflict of interest statement
R. Siegel has received consulting fees from Abbott and is a member of the speakers bureau for Philips Ultrasound. A. Trento has received lecture fees from Abbott Cardiovascular. S. Kar has received grant support and/or consulting fees from Abbott Vascular, Boston Scientific and St. Jude Medical. The other authors have no conflicts of interest to declare.