Introduction
This is the first article in the EuroIntervention Tools & Techniques series and deals with the step-wise approach in the percutaneous treatment of coronary ostial disease. The following is an overview of its management and highlights the salient technical features to be covered in the online version. The complete, unabridged chapter with dynamic angiographic images can be viewed at www.eurointervention.org
Background
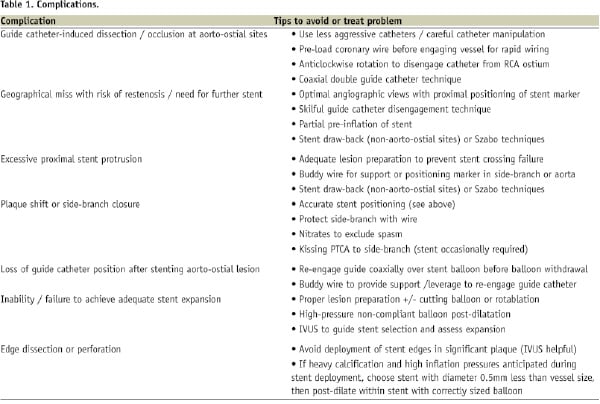
Ostial disease is traditionally defined as a lesion arising within 3 mm of the vessel origin. It may be classified by location as described below: (Figure 1)
1. Classification of coronary ostial disease by location.
– Aorto-ostial – involving the ostia of the RCA, LMS, and aorto-coronary bypass grafts.
– Non-aorto-ostial – involving the ostia of the major coronary arteries not arising directly from the aorta; i.e., the LAD, Cx and ramus intermedius.
– Branch ostial – involving the ostia of branches of the major coronary vessels; e.g., diagonal branches of the LAD; marginal branches of the Cx; and the posterior descending and posterolateral branches of the RCA.
Ostial lesions have a reputation of being fibrotic, calcified, and relatively rigid1,2. Aorto-ostial disease is felt to be additionally resistant to dilatation and prone to recoil due to the greater thickness of muscular and elastic tissue in the aortic wall. In the balloon angioplasty era, treatment of ostial lesions was associated with lower angiographic success than non-ostial lesions. Greater degrees of rigidity and recoil resulted in lower acute gain and higher rates of TLR. In addition, procedural complications such as dissections, vessel closure and myocardial infarction were more frequent3,4.
This led to interest in the use of adjunctive devices such as cutting balloons and rotational atherectomy for modifying or debulking plaque at ostial sites. However, it was not until routine use of stenting that meaningful improvement in outcomes was achieved, albeit with TLR rates still higher than at non-ostial sites5,6. Further progress has been achieved with the use of drug-eluting stents (DES)7 and intravascular ultrasound (IVUS) imaging to reduce restenosis. The difficulties and technical considerations involved in performing PCI on ostial stenoses are introduced briefly in the summarised version below, but full discussion and illustration of these issues and the methods used to achieve success and avoid complications, are addressed in the complete online version.
Indications
The indications for PCI on ostial lesions are in general no different to those for any lesion. However, in certain situations additional judgement and caution are required. These include: ostial LAD stenoses, where a strategy of stenting back into the left main stem may be preferable to precise ostial positioning; side-branch ostial disease, where the balance of risk vs. benefit may favour medical therapy; and ostial stenosis following previous bifurcation PCI, which may be difficult to treat without compromise of the parent or sister vessel. Finally, exclusion of coronary spasm at aorto-ostial sites due to guide catheter engagement is an important consideration. These issues will be discussed in detail.
Difficulties
The technical considerations listed below are discussed and illustrated fully in the web-based version of this article.
– Invasive assessment of ostial disease severity using pressure wire and IVUS interrogation with special considerations for aorto-ostial disease.
– Maintenance of guide catheter position with aorto-ostial lesions.
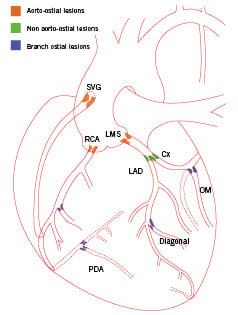
– Precise stent positioning is required for ostial PCI to obtain full lesion coverage yet avoid unnecessary proximal extension into the parent vessel or aorta (Figure 2).
2. Stent positioning at ostial sites with schematic illustration of ideal vs. non-ideal angles.
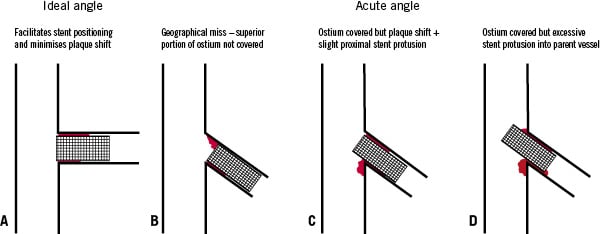
This may be hindered by failure to use appropriate angiographic views to minimise foreshortening or overlap (Figure 3); suboptimal visualisation from guide catheter engagement; and excess stent movement with cardiac contraction.
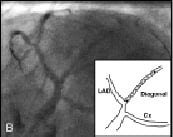
3. Stent positioning during PCI of diagonal branch. (A) Spider view (LAO 28°, caudal 38°) suggesting stent is covering ostium; (B) Change in image intensifier angle (LAO 50° caudal 40°) shows stent will miss ostium.
– Risk of plaque shift and branch compromise.
– Requirement for plaque modification or debulking.
– Stent under-sizing or under-expansion issues.
Methods
The following issues regarding equipment selection and techniques required for PCI on ostial lesions will be discussed along with suggested tips and tricks for dealing with potential problems.
– Femoral vs. radial approach.
– Equipment - selection of appropriate guide catheters and guidewires, with illustration of use of buddy wires for support or as positioning markers.
– Lesion preparation and post-dilatation - compliant vs. non-compliant balloons and the use of adjunctive devices such as cutting balloons, rotational and laser atherectomy.
– Stent selection - DES vs. BMS.
– Use of IVUS to determine PCI strategy and to guide stent selection and expansion (Figure 4).
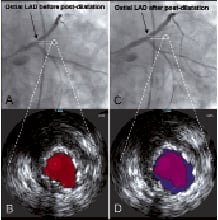
4. Effect of post-dilatation on stent expansion at LAD ostium. (A) before post-dilatation with corresponding IVUS (B) showing stent lumen area; (C & D) after post-dilatation with minimal angiographic change but significant difference in stent expansion on IVUS.
– Stent positioning - as precise stent positioning is critical when performing ostial PCI it is necessary to reiterate that the stent is within the radio-opaque markers on the stent balloon and thus the proximal marker must be positioned proximal to the ostium in any ostial lesion, as illustrated in Figure 5.

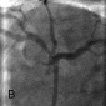
5. Positioning of proximal stent marker for ostial LAD PCI. (A) stent positioned too distally; (B) stent position correct; (C) stent deployment; (D) final result.
The use of multiple angiographic views, techniques for guide catheter disengagement, and tips to minimise stent oscillation will also be illustrated, as will specialised stent positioning methods such as the stent-drawback and Szabo techniques.
– Ostial stenosis following previous bifurcation angioplasty.
– Specialised ostial stenting devices.