Abstract
Aims: Patients with Ebstein’s anomaly of the tricuspid valve may have right-to-left shunt at atrial level resulting in hypoxaemia, high haematocrit and hyperviscosity syndrome. The purpose of this study was to assess the results of percutaneous closure of atrial right-to-left shunt in patients with Ebstein’s anomaly.
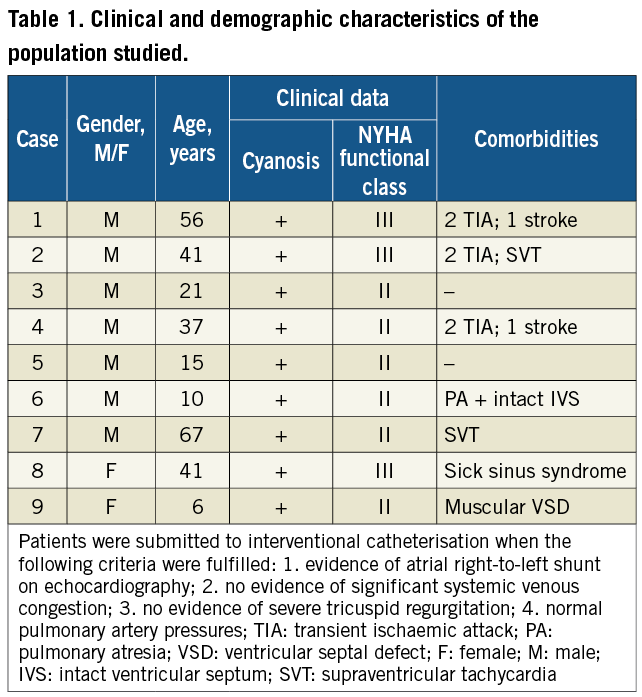
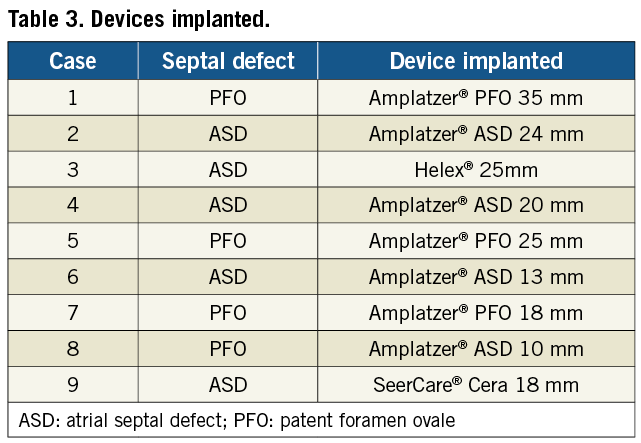
Methods and results: Records of patients treated between January 2002 and June 2010 were reviewed. Their condition before and after shunt closure (clinical data, oxygen saturation and haematocrit) were studied. During this period nine selected patients with Ebstein’s anomaly and right-to-left shunt at atrial level were treated. Ages ranged from six to 67 years; seven were male. Mean pulmonary artery pressures were under 25 mmHg in all. Three patients had previous episodes of stroke and three had very high haematocrit, two of whom required therapeutic phlebotomies. Test occlusion of the shunt was performed in all patients with a balloon catheter, revealing an increase in systemic oxygen saturation, with right atrial pressures remaining <18 mmHg in all. Percutaneous closure of atrial shunt was achieved in all. There were no major complications. Arterial oxygen saturations increased in all patients from 85.0±4.5% to 96.7±1.5% (mean±standard deviation). Medium follow-up was five years. The three patients with very high haematocrit levels had a decrease in its values from 62.9±2.8% to 45.5±3.9% after device occlusion. Both therapeutic phlebotomy programs were discontinued. All patients reported a marked improvement in effort tolerance.
Conclusions: Percutaneous closure of atrial right-to-left shunt in selected patients with Ebstein’s anomaly offers significant improvement, abolishing hypoxaemia and hyperviscosity and preventing paradoxical embolisation.
Introduction
Ebstein’s anomaly of the tricuspid valve (EA) is a rare congenital heart disorder which occurs in about 1-5 per 200,000 live births, accounting for <1% of all congenital heart defects1. Patients with EA have malformation of the tricuspid valve and the right ventricle (RV) and a variety of associated cardiac abnormalities, including atrial septal defect (ASD), patent foramen ovale (PFO), conduction system abnormalities, pulmonary stenosis or atresia and ventricular septal defect1. Dilatation of the right atrium (RA) is almost always present in EA, except for the very mild forms, and two thirds have dilatation of the RV. The dysplastic tricuspid valve is very frequently incompetent and may rarely be stenotic1. Atrial arrhythmias frequently occur especially at older ages1.
In the presence of an interatrial communication, right-to-left shunt may occur due to dilatation of the RA and increased RA pressures secondary to tricuspid regurgitation. The right-to-left shunt increases the risk of chronic hypoxia and polycythaemia, paradoxical embolisation and sudden death. In the current era and in experienced hands, transcatheter ASD closure can be performed safely and successfully, even in very young children2. Right-to-left shunt at atrial level has also been described in patients with no other cardiac anomalies and normal right sided pressures, causing hypoxaemia, which can be treated with device occlusion3. However there are only a few cases described in the literature of closure of atrial shunts in patients with EA and right-to-left shunt.
The purpose of this study was to evaluate safety and efficacy of percutaneous treatment in patients with EA and atrial right-to-left shunt.
We studied, retrospectively, the clinical data of patients with EA and atrial right-to-left shunt treated percutaneously at our institution between January 2002 and June 2010.
Population and methods
We included nine patients with a diagnosis of EA and atrial right-to-left shunt with a mean age of 33.7 years (six to 67 years). All patients had mild to moderate forms of EA.
Right-to-left shunt occurred through an ASD in five patients and through a PFO in four. At the time of the procedure all patients had O2 saturation levels ranging from 75 to 90%. All had clinical evidence of cyanosis and effort intolerance. Haematocrit levels were on the upper limit of normal or elevated, with three patients having haematocrit levels >63% (cases 1, 2 and 5). Two of these were on regular therapeutic phlebotomy programs (cases 1 and 2). Threee had a history of multiple cerebrovascular accidents (cases 1, 2 and 4; Table 1). No patient had evidence of significant systemic venous congestion. Only one patient had a complex congenital cardiac defect namely pulmonary atresia with intact ventricular septum, submitted during infancy to a right modified Blalock-Taussig shunt with a 4 mm GORE-TEX® stretch vascular graft (W.L. Gore & Associates, Inc., Flagstaff, Arizona, USA) and pulmonary valvotomy. One patient had a small apical muscular ventricular septal defect and an additional small ASD. Three patients had a history of arrhythmia: two had paroxysmal supraventricular tachycardia, one having had ablation of anomalous pathways, and one patient had sick sinus syndrome with a previous pacemaker implantation (Table 1).
Six procedures were performed under general anaesthesia, guided by transesophageal echocardiography. Three were performed with sedation and intracardiac echocardiography.
Closure of ASD and PFO was performed with a standard technique, as described widely in the literature. Intravenous heparin (50-100 UI/kg; maximum of 5,000 UI) and prophylactic antibiotics were given. A balloon catheter was used in all procedures for test occlusion and sizing of the device.
Baseline pressures in the RA, RV, pulmonary artery (PA), left atrium and aorta were measured and registered in all patients. Balloon test occlusion of the ASD/PFO was used to evaluate the stretched diameter of the defect. The balloon was maintained inflated for 15 minutes to evaluate haemodynamic and oxygen saturation response to shunt closure. If RA pressures remained ≤18 mmHg and there were no signs of low cardiac output, the septal defect was closed percutaneously. Evaluation of immediate residual leak was performed with transesophageal (TEE) or intracardiac echocardiography (ICE). After the procedure, all patients were treated with aspirin (3-5 mg/kg; maximum 100 mg daily) and antibiotic prophylaxis for six months. Patients over 30 kg received a loading dose of clopidogrel (300 mg) followed by 75 mg daily for one month.
Single-tailed paired t-test was used to compare both PA and RA pressures and O2 saturation levels before and after treatment. Again, a single-tailed paired t-test was used to compare the haematocrit of the three patients with high haematocrit before and after treatment. In all cases, a p-value<0.05 was considered statistically significant.
Results
Baseline mean arterial pressures in PA and RA were less then ≤25 mmHg and ≤18 mmHg, respectively, in all patients (Table 2).
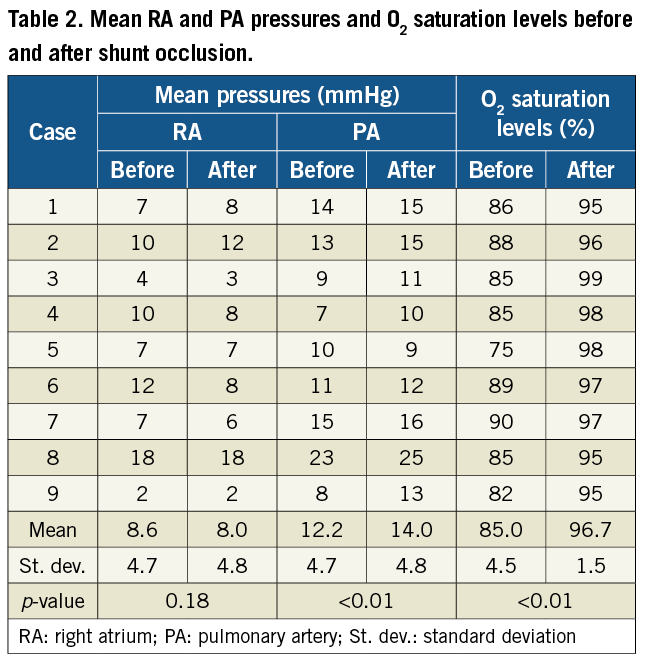
Balloon test occlusion was performed in all cases, with an immediate rise in O2 saturation levels in all patients. There was no statistical difference between mean RA pressures before and after treatment (p=0.18) and mean RA pressures remained ≤18 mmHg in all patients. Although there was a statistically significant rise in mean PA pressures before and after treatment (p<0.01), mean PA remained ≤25 mmHg in all patients. Devices used for percutaneous closure included the GORE®HELEX® septal occluder (1) (W.L. Gore & Associates, Inc., Flagstaff, Arizona, USA), SeerCare®Cera ASD (1) (Lifetech Scientific [Shenzhen] Co., Ltd, Shenzhen, China), Amplatzer®ASD occluder (4), Amplatzer®PFO occluder (3) (both St. Jude Medical, St. Paul, MN, USA) (Table 3). One patient had an atrial fibrillation episode with a fast ventricular rate, which was converted promptly to sinus rhythm. There were no other events during the procedures. There was a significant rise in O2 saturation levels from 85.0±4.5% to 96.7±1.5% (mean±standard deviation) (p<0.01) (Table 2). In all patients, an echocardiogram was performed at the end of the procedure by TEE or ICE, showing no residual flow.
Mean follow-up was 5.2 years, ranging from one to eight years. No patient had residual right-to-left shunt on transthoracic echocardiographic evaluation performed six months after the procedure. Patients with previous cerebrovascular accidents (cases 1, 2 and 4; Table 1) underwent TEE, which revealed no residual shunt at atrial level, including with Valsalva manoeuvre.
Only one patient (case 6) developed signs of moderate systemic venous congestion, requiring diuretics for three months. Three patients who had very high haematocrit levels had a significant decrease from 62.9±2.8% to 45.5±3.9% (p-value<0.01) (Figure 1). Therapeutic phlebotomy programs were discontinued in patients 1 and 2. There were no neurologic events.
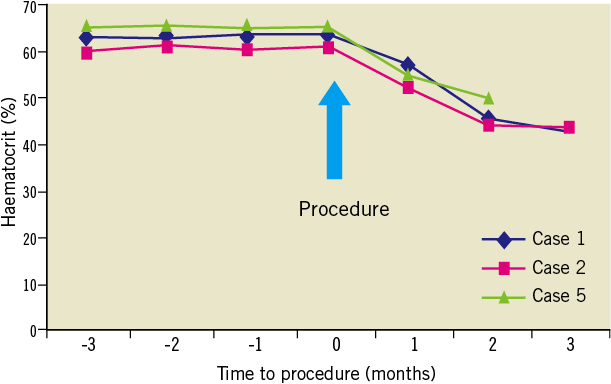
Figure 1. Evolution of haematocrit levels of the three patients with severe polycythaemia, two of whom were on therapeutic phlebotomies before the procedure. The remaining patients had normal haematocrits.
During follow-up there were no other episodes of significant arrhythmias and the degree of tricuspid regurgitation assessed echocardiographically did not change significantly in any patient. All patients reported marked improvement in effort tolerance: there was a change in functional class in all, from functional class III (three patients) to class I (one patient) or II (two patients), and from functional class II (six patients) to class I (six patients). Mean O2 saturation levels at late follow-up was 95%, and above 93% in all patients.
Discussion
An interatrial communication (ASD or PFO) is present in 80%-94% of patients with EA1. Right-to-left shunt may occur leading to chronic hypoxia and polycythaemia, paradoxical embolisation and sudden death.
Patients with cyanosis on exercise who have an ASD or PFO but only mild to moderate tricuspid regurgitation have been reported to benefit from device closure to alleviate cyanosis and prevent paradoxical emboli1.
The risk of closing a right-to-left shunt in these patients is to increase right ventricular overload, with a potential increase in the degree of tricuspid regurgitation, systemic congestion and, in more severe cases, low cardiac output. Balloon test occlusion is important in order to determine immediate individual response to shunt occlusion in patients with EA of the tricuspid valve. Accurate patient selection is of paramount importance and difficult cases should be discussed with an experienced congenital cardiac surgeon. Patients with severe tricuspid regurgitation, pulmonary hypertension or systemic congestion should be excluded from this approach, as right-to-left shunt occlusion can be detrimental in this subset of patients.
During a mean follow-up of five years, our patients did not have significant complications, namely arrhythmias or increase in tricuspid regurgitation. Only one patient developed mild systemic congestion, which was treated with diuretics. Interestingly, this patient had mean RA pressure of 14 mmHg at the end of the procedure, but he had pulmonary atresia and intact ventricular septum treated in the neonatal period by pulmonary valvotomy and modified Blalock-Taussig shunt.
In the current era and in experienced hands, transcatheter ASD closure can be performed safely and successfully, even in very young children2. Closure of right-to-left shunt at atrial level has been reported in the literature as an approach to different problems. Hsu et al4 described in 1995 transcutaneous closure of right-to-left shunt in eight Fontan patients as a technically feasible and effective procedure. Godart et al3 reported percutaneous closure of atrial right-to-left shunt in a population of 11 patients with cyanosis and without other cardiac anomalies, with good results. Calderón et al5 described in 2005 percutaneous closure of atrial communications in two patients, one with EA, in the context of cerebrovascular accident. Apart from some rare case reports6-8, there are only two other papers in the literature reporting series of patients with EA and right-to-left shunt at atrial level treated by device closure. The first is by Agnoletti et al who reported percutaneous closure of right-to-left shunt in four patients with EA, also with good results, but no long-term follow-up data was available.9 The second paper is by Jategaonkar et al10. They described percutaneous closure of right-to-left shunt in nine adult patients with EA, but again no long-term follow-up data was available. Until now no large series with long-term follow-up has been reported on these patients.
Our experience with nine patients confirms that closure of right-to-left shunt in selected patients with EA has good immediate and late results, and no complications reported at a mean follow-up of five years (ranging from one to eight years).
Conclusions
Percutaneous closure of atrial right-to-left shunt in selected patients with Ebstein’s anomaly appears to be safe and offers significant long-term improvement, abolishing hypoxaemia, hyperviscosity and preventing paradoxical embolisation. This form of treatment should be considered more often in this group of patients.
Conflict of interest statement
The authors have no conflict of interest to declare.

