Abstract
Aims: This study aims primarily to assess the extent of the collateral circulation of the hand in a combined population of healthy individuals and patients who underwent transradial catheterisation, using both the Nexfin system and laser Doppler perfusion imaging.
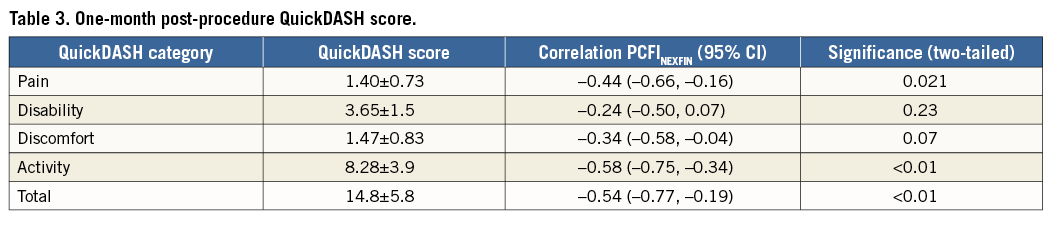
Methods and results: In total, 85 adults were included in the study (18 healthy volunteers; 67 patients who underwent transradial catheterisation). The perfusion of the thumb was assessed prior to and during complete radial artery compression using laser Doppler perfusion imaging (LDPI) and the Nexfin system. The palmar collateral flow index (PCFI) was compared between both devices and PCFINEXFIN was related to hand angiography and the upper limb function, using the QuickDASH questionnaire. Mean PCFILDPI was 0.77±0.15 and mean PCFINEXFIN was 0.88±0.08. Both were significantly related (Pearson correlation=0.49, 95% CI: 0.31–0.64, p<0.001, agreement –0.11±0.13). PCFINEXFIN correlated with the maximal diameter of the superficial palmar arch (R=0.49, p=0.04) and total minimal arch diameter (R=0.51, p<0.02). High PCFINEXFIN, measured at baseline, was correlated with a lower QuickDASH score for pain, activity and total at one month post transradial catheterisation (p=0.02, p<0.01, p<0.01), but not with discomfort or disability.
Conclusions: The Nexfin monitoring system is comparable with laser Doppler perfusion imaging in the quantification of the collateral perfusion in the hand. In patients, the Nexfin-derived collateral flow index measured at baseline is associated with clinical outcome at 30 days post transradial catheterisation.
Abbreviations
CAD: coronary artery disease
CFI: collateral flow index
DASH: disabilities of the arm, shoulder and hand
DPA: deep palmar arch
LDPI: laser Doppler perfusion imaging
PCFI: palmar collateral flow index
PCFILDPI: laser Doppler-derived PCFI
PCFINEXFIN: Nexfin-derived PCFI
Poccl: pressure during radial artery occlusion
Prest: pressure during baseline
QuickDASH: shortened version of the DASH questionnaire
RA: radial artery
RAO: radial artery occlusion
ROI: region of interest
SPA: superficial palmar arch
UA: ulnar artery
Introduction
Collateral anastomoses provide blood flow to tissues or vessels when arterial patency is compromised and can already be found in the early stages of life and throughout the body. The vasculature of the hand also contains anastomoses. Typically, two main arteries, the ulnar and the radial artery (and in some cases the interosseous artery), provide blood flow to the palmar circulation and form two major end-arterial collateral connections, the superficial palmar arch (SPA) and the deep palmar arch (DPA). The SPA is typically the dominant artery in the hand, mainly supplying blood flow to the digits1. These arches can compensate perfusion in case arterial supply is partly halted, pathogenically or iatrogenically. Palmar arch anatomy can be broadly divided into complete and incomplete2, but multiple subtypes can be identified3,4, all affecting collateral responsiveness.
Nowadays, for cardiac catheterisation a transradial approach is favoured due to fewer access-site complications5,6, better quality of life and lower costs7. However, during this procedure the radial artery is (almost) completely blocked by an intra-arterial sheath, whereby hand perfusion is dependent on perfusion by the ulnar artery or interosseous artery and collateral anastomoses. Generally, transradial catheterisation does not influence upper limb function and hand perfusion is maintained8-10. However, in up to 40% of patients collateral perfusion falls short and symptoms may occur, especially after complete radial artery occlusion (RAO)2,11,12. In some cases, recanalisation is warranted to relieve ischaemic symptoms13. For these patients the transradial approach may not be optimally suited or “slender” techniques with small-size sheaths should preferably be used14.
Investigation of palmar arch patency is typically carried out with the (modified) Allen test, which is easy to perform but liable to misinterpretation15, is not always performed prior to catheterisation16 and has limited prognostic value in relation to clinical effect9. Palmar circulation can be examined more objectively with other non-invasive tests15,17,18, of which only laser Doppler perfusion imaging (LDPI) provides quantitative blood flow17,19. The Nexfin® monitoring system (Bmeye B.V., Amsterdam, The Netherlands) is a relatively new system that measures finger arterial pressure waveforms. Additionally, these measurements can be used for the quantification of the palmar circulation. Currently the Nexfin system has been well validated for blood pressure measurements, even when blood pressure is low20,21.
Quantitative measurements allow the calculation of the palmar collateral flow index (PCFI), which is determined by assessing perfusion before and after complete radial compression. We hypothesised that the Nexfin monitoring system is capable of adequately measuring the palmar collateral circulation. This study aims primarily to assess the extent of the collateral circulation of the hand in a combined population of healthy individuals and patients who underwent transradial catheterisation, using both the Nexfin system and laser Doppler perfusion imaging. Secondly, this study analyses the correlation of the non-invasively measured palmar collateral circulation with the angiographic palmar arch anatomy. Finally, we determined whether the extent of the palmar collateral circulation was related to hand function after transradial cardiac procedures.
Methods
STUDY DESIGN AND POPULATION
In total, 85 adults were enrolled in this study, consisting of 18 healthy volunteers and 67 patients with suspected coronary artery disease who underwent transradial coronary angiography, as part of the ACRA study (Assessment of disability after Coronary procedures using Radial Access)8. All study participants provided informed consent.
MONITORING DEVICES
Palmar blood flow was measured with two non-invasive monitoring devices: 1) laser Doppler perfusion imager (LDPI) (moorLDI2-IR; Moor Instruments Ltd, Axminster, United Kingdom), and 2) the ccNexfin monitoring device. In the patient group, LDPI and Nexfin measurements were conducted prior to catheterisation.
For the LDPI measurements, patients were asked to place their hands dorsal side facing up. The distance between the thumbs and the LDPI camera was consistently 40 cm. If present, nail polish was removed prior to measurement. All measurements were performed in a quiet and low stimulus room and at a controlled ambient temperature of between 20° and 22° C.
After choosing the appropriate size, the Nexfin finger cuff was carefully positioned on the thumb and connected to the wristband connection module, according to the manufacturer’s instructions.
RADIAL ARTERY COMPRESSION
Complete radial artery occlusion was established with a TR-Band® radial artery compression device (Terumo Medical Corp., Tokyo, Japan). The radial artery was located with manual palpation, after which the TR-Band was placed according to the manufacturer’s instructions. After baseline measurements, radial artery occlusion was established by inflating the balloon with ≥18 mL air, according to the manufacturer’s instructions. Complete radial occlusion was checked with a BT-200 Vascular Doppler (Bistos Co. Ltd, Gyeonggi-do, South Korea).
MEASUREMENTS
Both thumbs were scanned with LDPI using infrared and normal photography (Figure 1). Subsequently, the right hand was attached to the Nexfin system, as described above, and baseline data were recorded for five minutes. After this period, but without stopping the continuous Nexfin measurement, the radial artery was occluded. Again, data were recorded for five minutes (Figure 2), after which the Nexfin system was detached. With the TR-Band still inflated, a second LDPI scan was made. Finally, the radial artery occlusion was removed. In patients, all measurements were carried out prior to catheterisation.
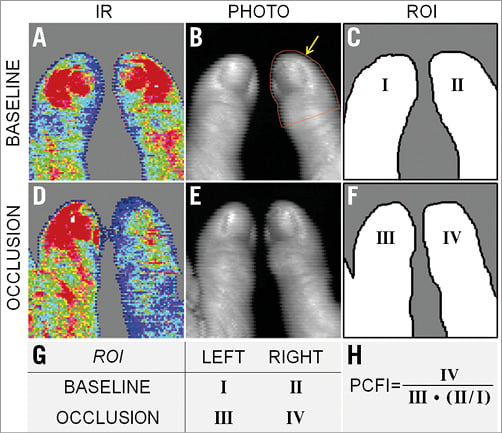
Figure 1. Laser Doppler perfusion imaging (LDPI) measurements. Top row represents measurements at baseline, middle row represents measurements during radial artery (RA) occlusion. Panels A and D depict the infrared (IR) LDPI images. High perfusion is displayed in red, intermediate perfusion in green and low perfusion in blue. Panels B and E are normal light photography images, which are taken simultaneously with A and D, respectively. In panel B a region of interest (ROI) is drawn which is indicated by the yellow arrow. A clear loss of IR LDPI signal can be seen after RA occlusion (D), as compared to baseline (A). Panels C and F show a graphic overview of ROIs of thumbs in panels A, B, D & E. Panel G gives a schematic overview of the different ROIs. Panel H shows the formula for PCFILDPI in which a corrected signal of the left thumb is used to approximate simultaneous measurement of proximal and distal pressure.
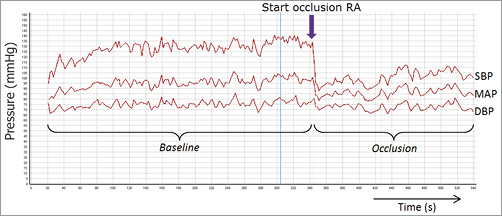
Figure 2. Nexfin measurements. Typical example of Nexfin measurement, showing blood pressure as a function of time. Top line represents systolic blood pressure, middle line mean arterial pressure and bottom line is diastolic pressure. After occlusion of the radial artery (arrow), a clear drop in pressure can be seen.
PALMAR COLLATERAL FLOW INDEX
Calculation of the palmar collateral flow index (PCFI) was based on the coronary collateral flow index in which a wedge pressure is measured during total occlusion22. In the coronary setting, collateral flow index (CFI) has been well validated and has strong prognostic value23,24. For the calculation of the PCFI, measurements of the thumb were used, based on the fact that the thumb is normally predominantly perfused “antegradely” by the radial artery25. After full radial artery compression the perfusion of the thumb relies completely on collateral blood supply.
LASER DOPPLER-DERIVED PCFI
Based on the photographic images, a region of interest (ROI) was drawn manually from the tip of the thumb to just below the nailbed (Figure 1). This was carried out bilaterally, on both baseline and occlusion images, using the LDPI v6 PC software (Moor Instruments). For perfusion quantification, infrared (IR) data were used. Average perfusion per ROI was used for the calculation of the PCFILDPI (Figure 1). During radial artery occlusion, the right-hand thumb perfusion was used for Poccl and the left-hand thumb perfusion was used for Prest, which was corrected by the ratio between LDPI of both thumbs at baseline (Figure 1). PCFILDPI was calculated as: PCFI=Poccl/Prest.
NEXFIN-DERIVED PCFI
For the Nexfin-derived PCFI (PCFINEXFIN), the average uncorrected systolic blood pressures of the right-hand thumb prior to and during radial artery occlusion were used, using the Nexfin@PC 2.0 and FrameInspector V2.3.0.2 software (both Bmeye, now Edwards Lifesciences). PCFI was calculated as follows: PCFI=Poccl/Prest, in which Poccl stands for the average perfusion of the thumb during radial artery occlusion and Prest is the perfusion of the thumb prior to occlusion.
MODIFIED ALLEN TEST AND BARBEAU TEST
In all patients, the modified Allen test was performed. In short, patients were asked to clench their fist, after which the radial and ulnar arteries were compressed. Subsequently, patients opened their hand, revealing a blanched palm. The ulnar artery was then released and the time needed for maximal blushing of the hand was assessed. A blushing time >10 seconds was considered abnormal4. For the Barbeau test, a pulse oximeter was placed on the thumb and oxygen saturation recorded. After that, the radial artery was compressed, and the change in the saturation pattern was noted. The results were divided into four types as previously described26. We considered the (reverse) Barbeau test to be abnormal in case of type C and D, representing suboptimal (collateral) or no blood supply to the thumb.
ANATOMY PALMAR ARCH
The vascular anatomy of the hand was visualised in patients during the coronary angiogram procedure. In short, after introduction of the radial sheath, but prior to the introduction of the guiding catheter, a bolus of contrast medium was administered via the introducer sheath to visualise the palmar vasculature. These images were analysed for palmar arch anatomy variations according to classification of palmar artery dimensions3,4. Furthermore, the diameters of the SPA and DPA were measured.
CLINICAL OUTCOMES
For the assessment of the symptoms and functionality of the intervened arm one month after transradial access, patients were asked to answer the shortened version of the Disabilities of the Arm, Shoulder and Hand (QuickDASH) questionnaire at one-month follow-up. The QuickDASH questionnaire consists of multiple categories (pain, disability, discomfort, activity), and the score represents the severity of the symptoms and disabilities of the patient27.
STATISTICAL ANALYSIS
The normality of continuous variables was tested by means of the Kolmogorov-Smirnov test. All normally distributed variables are summarised as mean±standard deviation. Agreement between the LDPI and the Nexfin devices was quantified using bivariate analyses. Bias and limits of agreement (LOA) (bias [2.0 SD]) were calculated according to the Bland-Altman statistical method. Means were compared between groups using an independent t-test or ANOVA in the case of three groups or more. Statistical analysis was performed with Statistical Package for Social Sciences, Version 20.0 software (IBM Corp., Armonk, NY, USA).
Results
STUDY POPULATION
In total, 85 adults were enrolled in this study, of whom 18 were healthy individuals (21%) and 67 had suspected coronary artery disease (79%). All study participants underwent Nexfin and LDPI measurements (Table 1).
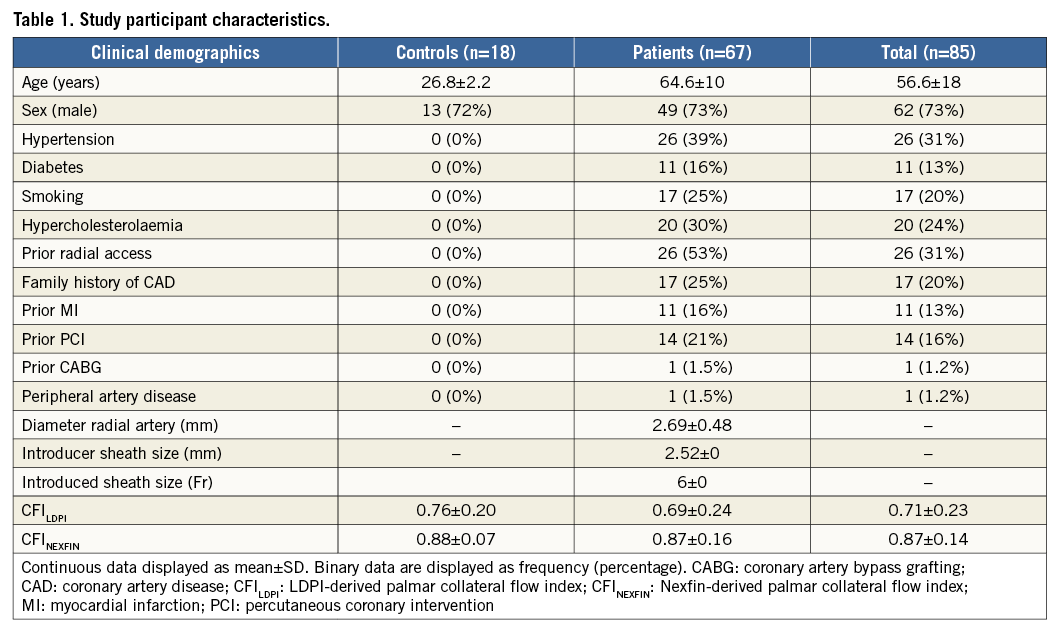
NEXFIN VERSUS LDPI
In all patients, the radial artery occlusion was complete, as checked by vascular Doppler. Mean PCFILDPI was 0.77±0.15, with an upper and lower limit of 0.39 and 1.0, respectively. Mean PCFINEXFIN was 0.88±0.082, with upper and lower limits of 0.63 and 1.0, respectively (Figure 3). Both parameters were significantly associated (Pearson correlation R=0.484, p<0.001). The bias was estimated as –0.11, with limits of agreement being –0.37 and 0.15 (Figure 4).
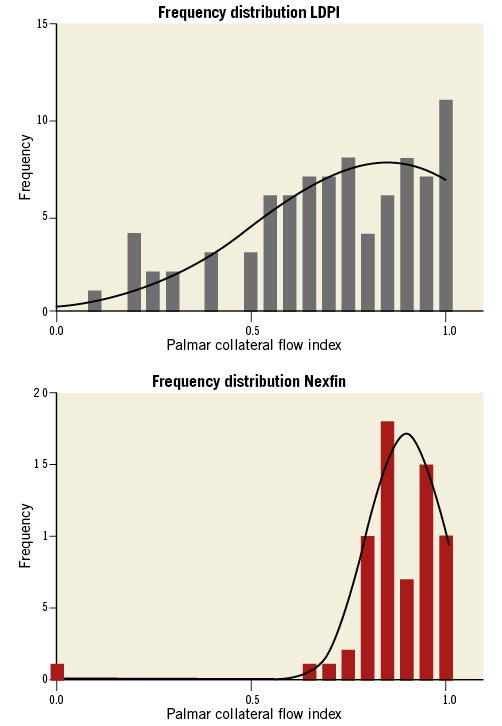
Figure 3. Distribution PCFI. Frequency histogram of PCFI measurements of both the laser Doppler perfusion imaging (LDPI), top panel, and the Nexfin system, lower panel.
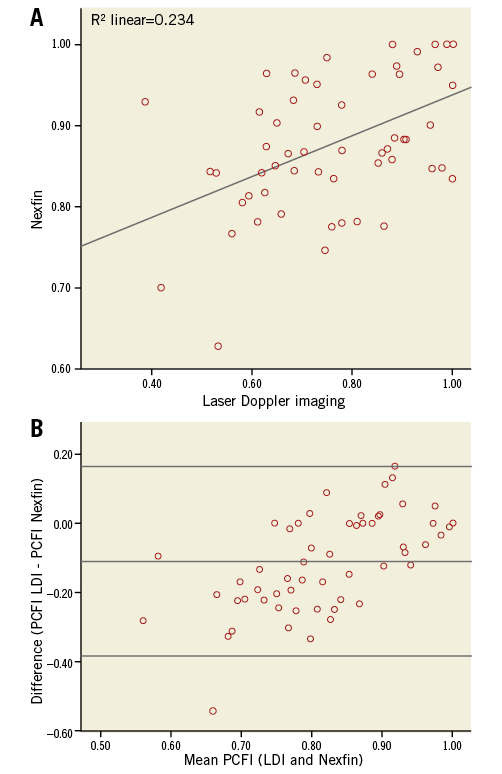
Figure 4. Scatter plot and Bland-Altman plot. A) Scatter plot of PCFI values. PCFILDPI is represented on the x-axis, and PCFINEXFIN is represented on the y-axis. B) Bland-Altman plot of PCFILDPI and PCFINEXFIN. The x-axis shows the mean of both measurement techniques. The y-axis shows the absolute difference between PCFILDPI and PCFINEXFIN. The middle horizontal line represents the mean difference. The upper and lower horizontal lines stand for 95% confidence intervals of the difference.
NEXFIN AND LDPI IN RELATION TO OTHER NON-INVASIVE TESTS
Patients with an abnormal modified Allen test showed a trend towards a lower mean PCFINEXFIN more than patients with a normal Allen test (0.76±0.29 vs. 0.89±0.07, p=0.059). PCFINEXFIN was similar in patients both with and without an abnormal Allen test (0.68±0.025 vs. 0.65±0.26, p=0.93). Mean PCFINEXFIN was found to differ between groups classified on the basis of Barbeau’s test (p<0.01). Interestingly, the only patient with Barbeau type 4 (complete loss of oxygen saturation after RA compression) also showed complete loss of perfusion on the Nexfin.
VASCULAR ANATOMY
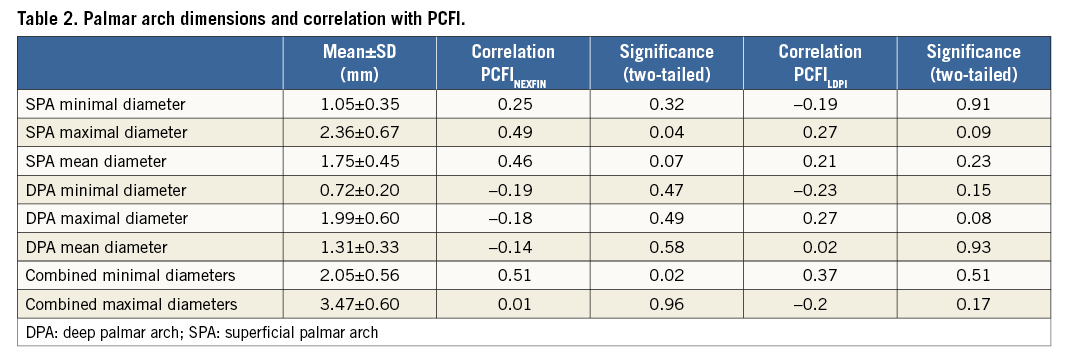
During catheterisation, contrast images of the hand were obtained (Figure 5) and palmar arch anatomy was characterised. In all patients at least one of the arches was complete. The DPA was complete in 82% of patients, and the SPA was complete in 52%. The mean PCFINEXFIN did not differ between groups with different anatomy types (Coleman classification3, p=0.73, Ruengsakulrach classification4, p=0.75). The SPA showed a larger mean diameter than the DPA (1.75 and 1.31 mm, p<0.01). The maximal diameter of SPA was positively correlated with the PCFINEXFIN (Pearson’s correlation: R=0.49, p=0.04). The dimensions of the DPA did not correlate with PCFINEXFIN. When the minimal diameters of both arches were combined, which reflects the total collateral system in the hand, a significant correlation with PCFINEXFIN was found (Pearson’s correlation: R=0.51, p<0.02). When the PCFILDPI was compared with the vascular anatomy, none of the correlations reached statistical significance (Table 2).
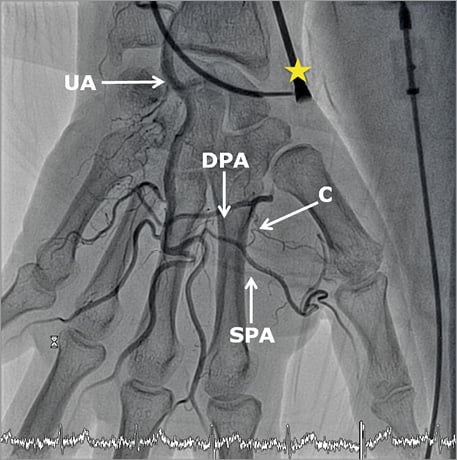
Figure 5. Anatomy of palmar vasculature. An X-ray image of the hand with arterial contrast medium, showing the vascular anatomy. An arterial sheath is visible in the radial artery (yellow star). Contrast medium enters the palmar vasculature via the ulnar artery (UA), which continues as the deep palmar arch (DPA) and the superficial palmar arch (SPA). Between major arteries several smaller collateral connections can be seen (C).
CLINICAL OUTCOMES
One month after the procedure, 60 patients completed the QuickDASH questionnaire which consists of four subcategories (pain, disability, discomfort, activity). In total, seven patients did not complete the questionnaire due to a switch to transfemoral catheterisation (n=4) or were lost to follow-up (n=3).
PCFINEXFIN was negatively correlated with the QuickDASH score in the categories of pain, activity and total (p=0.021, p<0.01, and p<0.01, respectively). Correlation with disability (p=0.23) and discomfort (p=0.07) did not reach statistical significance (Table 3).
Discussion
Laser Doppler perfusion imaging (LDPI) is the only non-invasive way to assess perfusion in the hand quantitatively and is considered the gold standard17. However, due to costs and portability, it is not suitable for daily clinical practice. This study shows that the Nexfin system shows a reasonable correlation with LDPI for the measurement of collateral perfusion in the hand and is related to functional outcome as assessed by the QuickDASH score.
Collateral perfusion in the hand has been studied for several decades, primarily within the scope of radial artery harvesting18,28. The introduction of transradial percutaneous coronary interventions has led to a renewed interest in the collateral circulation of the hand. In the case of a typical palmar arch, the perfusion of the hand and its digits can be maintained to an adequate level when one of the donor vessels is occluded. When the palmar arches are both incomplete, radial artery occlusion may induce ischaemia of the hand29,30 and the transradial approach should be avoided31. Even when radial artery occlusion is not diagnosed, patients can develop symptoms after transradial catheterisation. These symptoms are often viewed as procedural effects, and could be attributed to the limited palmar perfusion during transradial sheath placement. Identifying patients at risk remains a challenge. Typically, palmar collateral circulation is investigated with the (modified) Allen test, in which skin colour is used to objectify collateral perfusion. This simple test, which can be executed without any tools or devices, does have some disadvantages and its place in current practice is questionable32. Therefore, other tests and imaging modalities have been proposed to assess palmar perfusion of the hand more objectively15,17,18. Although these techniques aim to quantify perfusion, they are based on a broad range of derivatives, such as haemoglobin concentration, echo Doppler and ultrasonography. As one might expect, these methods all have some advantages and limitations28. LDPI is one of the few methods which can provide quantitative blood flow and is therefore considered the gold standard17. For clinical practice, however, the immobility of the device and its costs limit its practical use. The Nexfin system was recently validated against invasive blood pressure monitoring33,34, but has not yet been tested for its use in quantifying collateral perfusion during radial artery occlusion. Here, we show for the first time that the Nexfin system can also be used for the quantification of the collateral perfusion in the hand.
A potential shortcoming of the Nexfin system for assessment of the extent of the palmar collateral circulation is the fact that it is pressure based as opposed to LDPI which is based on erythrocyte flux. It should be noted, however, that coronary collateral perfusion is also quantified with the pressure-based collateral flow index (CFIp), which is well validated and has strong prognostic value23,24. Furthermore, the Nexfin system is most probably less susceptible to environmental influences such as temperature and ambient light, as compared to the LDPI. This could be one explanation for the difference in distribution between the two methods.
Both in healthy adults and in patients with chronic total obstructions, a great variance is observed in CFIp35-37. This implies a strong congenital basis for the anatomy of pre-existing arterial anastomoses as well as the arteriogenic response upon arterial obstruction. Here we show a similar variance in the extent of the palmar collateral circulation as measured by PCFINEXFIN. PCFINEXFIN was related to the maximal diameter of the hands’ dominant vessel, as well as the total minimal diameter. This implies that, in patients with a good collateral response, palmar vasculature is enlarged, facilitating a higher blood flow. This enlargement could be due to larger basal diameters or to well-functioning endothelial vasodilatation, or both. Arterial size itself is related to endothelially mediated vasodilatation38. Endothelially mediated vasodilation is typically measured in response to an increase in shear stress during post-occlusive hyperaemia. For example, the radial artery diameter increases by 5% after temporary occlusion (i.e., transradial catheterisation)39. In most cases, radial artery compression does not cause hypoxia26, which might suggest that endothelially mediated vasodilation did not contribute largely to our findings. Furthermore, we show that none of the included clinical parameters is significantly associated with the PCFINEXFIN. Some of these parameters are associated with (impaired) collateral vessel growth36. This might suggest that palmar collateral perfusion during temporary radial artery occlusion is based on pre-existing anatomical differences, rather than collateral artery growth.
Interestingly, PCFINEXFIN, measured prior to transradial catheterisation, is related to an improved clinical outcome in terms of post-procedural hand function. Patients with a high PCFINEXFIN were shown to have overall lower QuickDASH scores, as compared to patients with a low PCFINEXFIN, one month after catheterisation. This suggests that, in patients with low collateral perfusion in the hand, the effects of transradial access can persist for weeks after the procedure. From a clinical standpoint, the Nexfin system might help operators in the future in their choice of access route and the use of “slender” techniques40,41.
Limitations
There are some limitations to this study. Radial artery status was investigated by angiography at the end of the initial transradial angiography, but was not analysed in a standard fashion after 30 days. Furthermore, a low PCFINEXFIN was significantly associated with the occurrence of pain, but not with discomfort. This could be explained by the relatively broad definition of discomfort, which results in a greater variation among patients.
Conclusion
Here we show for the first time that the collateral perfusion in the hand can be assessed non-invasively by both LDPI and the Nexfin system. In patients, a larger extent of the collateral circulation of the hand is associated with improved clinical outcome at 30 days post transradial catheterisation.
| Impact on daily practice Assessment of the collateral circulation of the hand, using the Nexfin monitoring system, could be used as a screening tool in selected patients prior to cardiac catheterisation and might help operators in the future in their choice of access route and the use of “slender” techniques. |
Conflict of interest statement
The authors have no conflicts of interest to declare.