Abstract
Aims: The aim of this study was to explore the use of prolonged occlusion flow-mediated dilatation (PO-FMD) to dilate the radial artery prior to cannulation to increase cannulation success, reduce puncture attempts and reduce access-site complications in transradial coronary angiography.
Methods and results: A total of 1,156 patients undergoing transradial coronary angiography were randomised into PO-FMD and sham PO-FMD groups. PO-FMD was achieved by a 10-minute inflation of a blood pressure cuff on the arm to above systolic pressure, followed by deflation with resultant radial artery dilation. In the sham PO-FMD group the cuff was not inflated. Operators were blinded to the intervention. Five hundred and eighty (580) patients were randomised to the sham PO-FMD group and 576 to the PO-FMD group. Cannulation failure was reduced with PO-FMD, with cannulation failure rates of 2.7% in the PO-FMD group and 5.8% in the sham PO-FMD group (p=0.01).The number of puncture attempts was reduced with the use of PO-FMD, with a median of one attempt in the PO-FMD group and two in the sham PO-FMD group (p<0.001). Radial artery pulsation loss (RAPL) was reduced with PO-FMD, with 1.4% in the PO-FMD group and 3.8% in the sham PO-FMD group (p=0.02).
Conclusions: PO-FMD reduces cannulation failure rates, decreases puncture attempts, and decreases RAPL during transradial coronary angiography.
Introduction
Access to the coronary arteries has traditionally been obtained via the femoral arteries, the first transfemoral coronary angiogram being performed in 19581. Alternative access sites have since been explored with the first transradial coronary angiogram performed in 19892. Access via the radial artery has now been shown to be superior to femoral access with less major bleeding and fewer vascular complications3,4,5,6,7,8, to be more cost-effective with decreased hospital stay, to improve patient satisfaction3,9,10,11 and reduce all-cause mortality12. Transradial catheterisation has therefore become the accepted standard of practice.
The transradial approach is, however, not without challenges and complications. Cannulation of the radial artery is technically more challenging, with a steep learning curve to become proficient in the procedure and with higher cannulation failure rates compared to the transfemoral approach8,13. Access difficulty may result in complications, with an increase in the number of radial artery puncture attempts being reported to increase the occurrence of radial artery spasm (RAS)14, radial artery pulsation loss (RAPL), radial artery occlusion (RAO), pain and discomfort15.
One strategy to increase access success is to dilate the radial artery prior to cannulation. Various strategies can be used to achieve dilatation including sublingual or subcutaneous nitrates, hand exercises, hand warming, and flow-mediated dilatation (FMD). Flow-mediated dilatation is a physiological process whereby an artery is dilated by increasing the flow through it. This is usually achieved by inflation of a blood pressure cuff above the systolic pressure for a period of time, with subsequent deflation to restore flow and dilate the vessel. Occlusion of the brachial artery for five minutes results in nitric oxide-dependent dilatation of the artery distal to the occlusion during reperfusion16 and is commonly used as a diagnostic tool to assess endothelial function17,18,19. This nitric oxide-dependent dilatation is short-lived and diminished in patients with atherosclerosis. However, prolonged occlusion times prior to restoring blood flow induce nitric oxide-independent FMD, resulting in prolonged vasodilatation even in patients with hypercholesterolaemia16. Compared to other methods available to dilate the radial artery, FMD is cheap, easy to perform, and needs minimal equipment with negligible risk, making it an ideal strategy.
We explored the impact of prolonged occlusion flow-mediated dilatation (PO-FMD) in augmenting radial artery cannulation success. The primary aim was to assess its impact on the transradial cannulation failure rate. Secondary aims were to assess its impact on the number of radial artery puncture attempts and to evaluate its impact on rates of RAS, RAPL and RAO.
Methods
All patients scheduled to undergo transradial coronary angiography at a single tertiary cardiac centre (Tygerberg Hospital), as indicated by their clinical condition, were considered for inclusion. Patients who had consented to coronary angiography were asked to participate in the study and informed consent was obtained from those wishing to participate. Patients undergoing emergency primary percutaneous coronary intervention (PCI), emergency rescue PCI, or who were haemodynamically unstable precluding ultrasound assessment and 10-minute occlusion for PO-FMD were excluded from participation. Recruitment was carried out from April 2017 to July 2018. The Health Research Ethics Committee of Stellenbosch University approved the study protocol and the study was funded by the Research Fund of the Division of Cardiology, Department of Medicine, Stellenbosch University. The CONSORT 2010 checklist was used when reporting the results of the trial (Supplementary Appendix 1).
Baseline demographics were recorded on an anonymised case report form (age, sex, smoking habits, dyslipidaemia, hypertension, diabetes, weight, height and serum creatinine). The indication for coronary angiography and whether or not previous transradial coronary angiography had been performed was recorded. These data were captured by the cardiac technologists involved with the case.
Participants were allocated a study number in numerical order during recruitment and were randomly allocated into two groups, those in whom PO-FMD would be performed and those receiving sham PO-FMD (blood pressure cuff placed over the right brachial artery but the cuff was not inflated). Randomisation was accomplished by a computer-generated randomisation scheme using the participant study numbers. Allocation was recorded on a confidential study log available only to the cardiac technologists, blinding patient and operator to group allocation. The computer-generated randomisation scheme allocated patients to groups in a random manner, minimising bias, but blocked randomisation into groups of 100, with an allocation ratio of 1:1, to ensure balanced numbers throughout the recruitment process.
Participants had an ultrasound of the radial artery to be cannulated performed prior to angiography. All ultrasound assessments were performed using a Logiq E ultrasound machine (General Electric, Boston, MA, USA) with a 22 MHz probe. The radial artery internal diameter was measured 2-5 cm proximal to the styloid process. Cardiology fellows doing the assessments were blinded to group allocation.
In the PO-FMD group, a blood pressure cuff was placed above the antecubital fossa of the arm to be cannulated. It was inflated to 50 mmHg above the patient’s systolic blood pressure for 10 minutes after which the cuff was deflated and cannulation was commenced. In the sham PO-FMD group, a blood pressure cuff was placed above the antecubital fossa of the arm to be cannulated but not inflated. The PO-FMD/sham PO-FMD protocol was performed by the cardiac technologist involved with the case. The interventional cardiologists performing the radial artery puncture and subsequent angiogram were blinded to group allocation.
All study investigators were proficient in transradial coronary angiography. Investigators included cardiology trainees who had completed ≥50 radial cannulations. A palpation-guided transradial cannulation was performed according to a strict protocol (Supplementary Appendix 2). The number of puncture attempts, success or failure of cannulation, time to cannulation and occurrence of RAS were recorded. Number of radial artery puncture attempts was defined as the number of forward movements of the cannula in an attempt to cannulate the radial artery. A “patent haemostasis” protocol was followed after completion of the angiogram (Supplementary Appendix 3).
After achieving haemostasis, and once the TR Band had been removed, the radial artery was assessed again. The radial artery was palpated to determine whether RAPL had occurred (RAPL was defined as the inability to palpate the radial pulse). Ultrasound was then performed and the vessel diameter and the occurrence of RAO were recorded (RAO defined as the loss of radial artery pulsation on Doppler ultrasonography of the artery post procedure). If RAO occurred, the mechanism of the occlusion was determined by ultrasound. The timing of this assessment could not be standardised but needed to occur prior to discharge.
STATISTICAL ANALYSIS
Sample size estimation was based on the assumption of a cannulation failure rate of 10% with a 50% reduction with the use of PO-FMD with beta error set at 20%, power at 80% and a two-sided significance level of 0.05. The estimated sample size under these assumptions was n=864. Our sample size calculation was anticipated to be potentially unreliable. Cannulation failure rates are highly variable between centres with rates of <1% to >10% reported8,20,21,22. The local cannulation failure rate had not previously been studied in our centre but was estimated at 10% based on operator experience. Secondly the impact of PO-FMD could only be speculated on as it had not been used for this purpose previously. An interim analysis was performed to assess the need to adjust sample size. Due to lower than expected failure rates, the sample size was increased after the interim analysis with an assumption of a cannulation failure rate of 6% with a 50% reduction with the use of PO-FMD. Beta error and power were left unchanged. A one-sided 0.05 significance level was used after confirmation of the beneficial direction of the intervention effect following interim analysis. The estimated total sample size under these assumptions was n=1,131 using a Z test with unpooled variance. SPSS, Version 25 (IBM Corp., Armonk, NY, USA) was used to analyse the data. Non-parametric Mann-Whitney tests were used to compare non-normally distributed outcomes between the two treatment groups, while independent samples t-tests were used to compare normally distributed variables between the two treatment groups. Pearson’s chi-square tests were used to compare categorical variables between treatment groups. Spearman’s correlation analysis was used to investigate linear relationships between continuous variables that were not normally distributed.
Results
A total of 1,156 participants were enrolled in the study. Five hundred and seventy-six participants were randomised to the PO-FMD group and 580 to the sham PO-FMD group. Twenty-six patients were excluded from the data analysis, 16 from the PO-FMD group and 10 from the sham PO-FMD group. Analysis was performed on 560 patients in the PO-FMD group and 570 patients in the sham PO-FMD group (Figure 1). Six were excluded due to a lack of clarity on which intervention (PO-FMD or sham PO-FMD) was performed on the patient as there was a discrepancy between the patients’ group allocation according to the randomisation plan and the group recorded on the case report form. Twelve patients had femoral access performed from the start. Two patients were excluded as there was a possible delay between performing PO-FMD and attempting cannulation. Four patients had PO-FMD performed on the right arm but the left arm was cannulated. Two patients’ procedures were cancelled after randomisation.
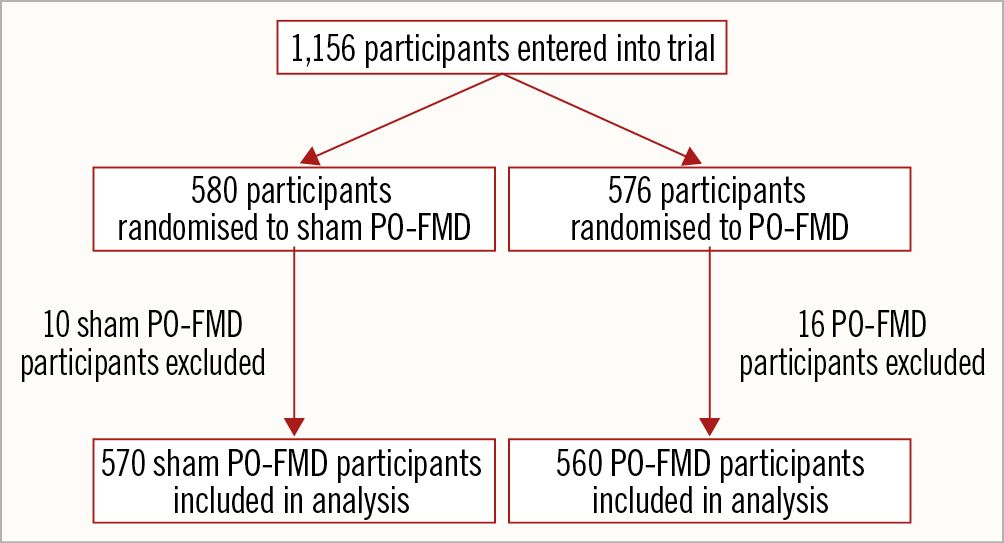
Figure 1. Flow chart illustrating the randomisation and exclusion of participants in the trial.
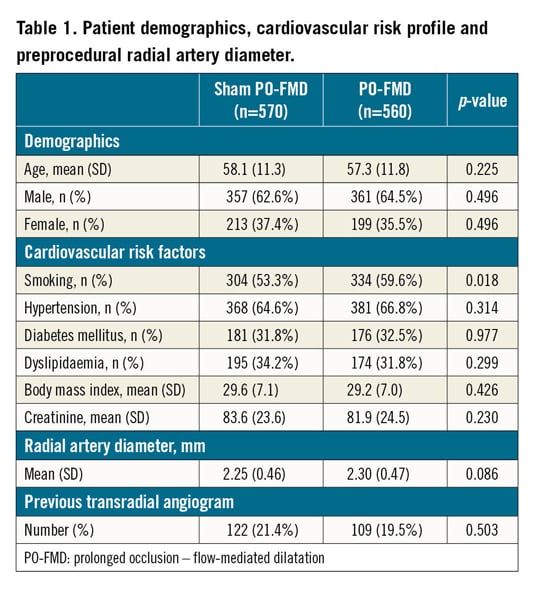
The baseline demographics, cardiovascular risk profiles and preprocedural radial artery diameters were comparable between the sham PO-FMD and PO-FMD groups (Table 1). Higher rates of smoking were noted in the PO-FMD group; otherwise, there were no significant differences between the groups. 6 Fr sheaths were routinely used. 5 Fr sheaths were used in 27 cases, 13 in the PO-FMD group and 14 in the sham PO-FMD group.
CANNULATION FAILURE RATES
A reduction in cannulation failure was demonstrated with the use of PO-FMD, with cannulation failure rates of 2.7% in the PO-FMD group and 5.8% in the sham PO-FMD group (p=0.01) (Figure 2). These patients required crossover to the left radial or femoral approach. Cannulation failures were associated with smaller preprocedural radial artery diameters when compared to those in whom cannulation was successful (p<0.001).
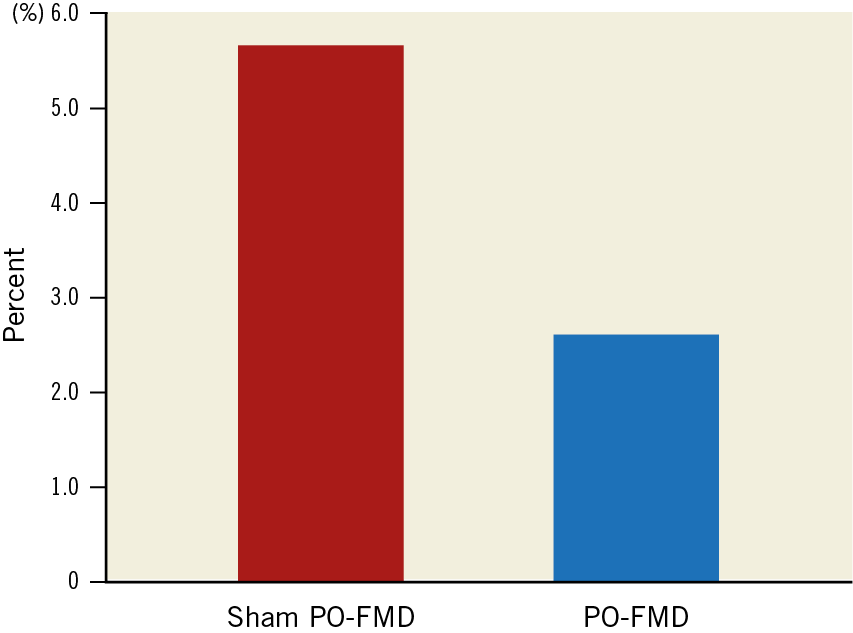
Figure 2. Cannulation failure rates.
NUMBER OF RADIAL ARTERY PUNCTURE ATTEMPTS
With the use of PO-FMD, a reduction in the number of radial artery puncture attempts was demonstrated, with a median number of puncture attempts of one in the PO-FMD group and two in the sham PO-FMD group (p<0.001) (Figure 3).
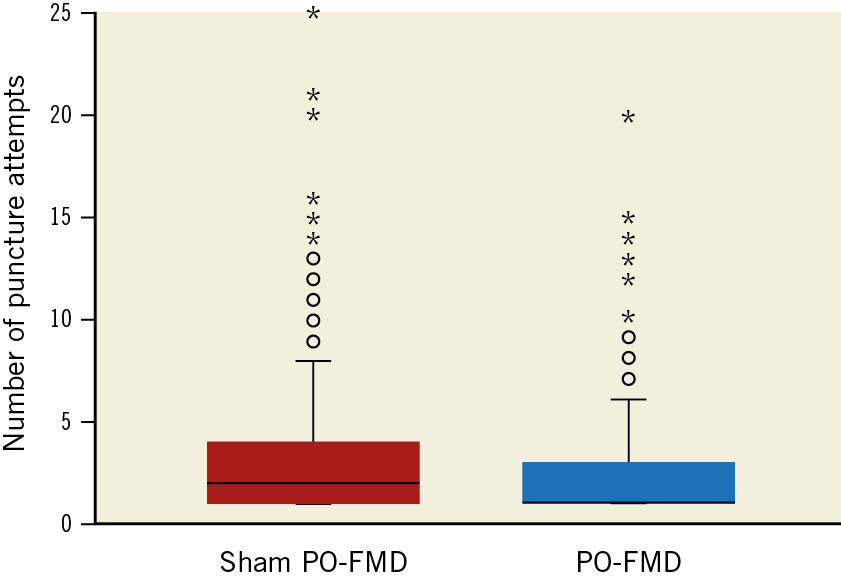
Figure 3. Number of radial artery puncture attempts to cannulate the radial artery.
A weak negative correlation was found between the preprocedural radial artery diameter and the number of puncture attempts needed to cannulate the radial artery (Spearman’s rho −0.173, p<0.001 in the PO-FMD group and Spearman’s rho −0.220, p<0.001 in the sham PO-FMD group) (Figure 4).
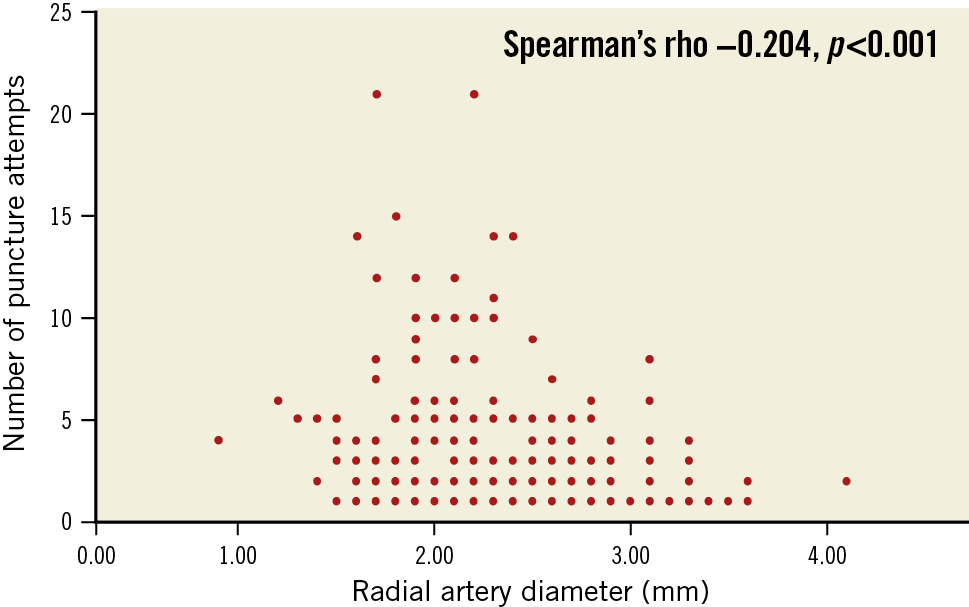
Figure 4. Correlation between the number of radial artery puncture attempts and radial artery diameter.
TIME TO CANNULATION
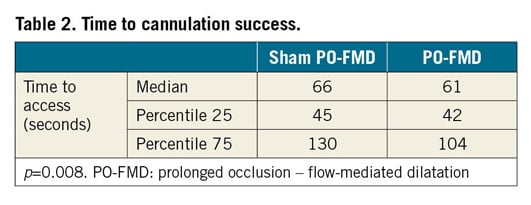
A reduction in cannulation time was demonstrated with the use of PO-FMD, with a median time to cannulation of 61 seconds in the PO-FMD group and 66 seconds in the sham PO-FMD group (p<0.008) (Table 2).
COMPLICATIONS
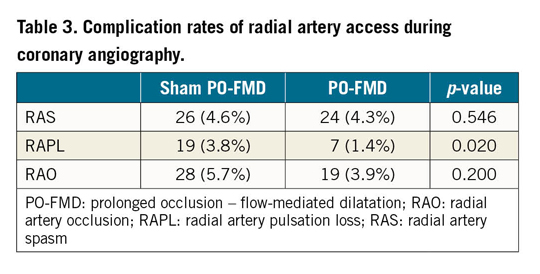
When assessing for complications of radial artery cannulation in terms of RAS, RAPL and RAO, we found that complication rates were low (Table 3). No difference was found in RAS rates in the groups, 4.6% in the PO-FMD group and 4.3% in the sham PO-FMD group (p=0.546). PO-FMD reduced RAPL rates, being 1.4% in the PO-FMD group and 3.8% in the sham PO-FMD group (p=0.02). RAO occurred in 3.9% of patients in the PO-FMD group and 5.7% in the sham PO-FMD group. This did not reach significance (p=0.2). When assessing the mechanism underlying the RAO, all were found to be due to radial artery thrombosis.
ADDITIONAL FACTORS IMPACTING ON RADIAL ARTERY DIAMETER, NUMBER OF PUNCTURE ATTEMPTS AND CANNULATION FAILURES
Females were found to have a significantly smaller radial artery diameter than males, with a mean of 2.05 mm (SD 0.39 mm) in females compared to 2.41 mm (SD 0.46 mm) in males (p<0.001). There were also significantly more radial artery puncture attempts in females compared to males (p=0.001), with the median attempts in females being two compared to one attempt in males (Figure 5), as well as higher cannulation failure rates in females (7.3%) as compared to males (2.6%) (p<0.001) (Figure 6).
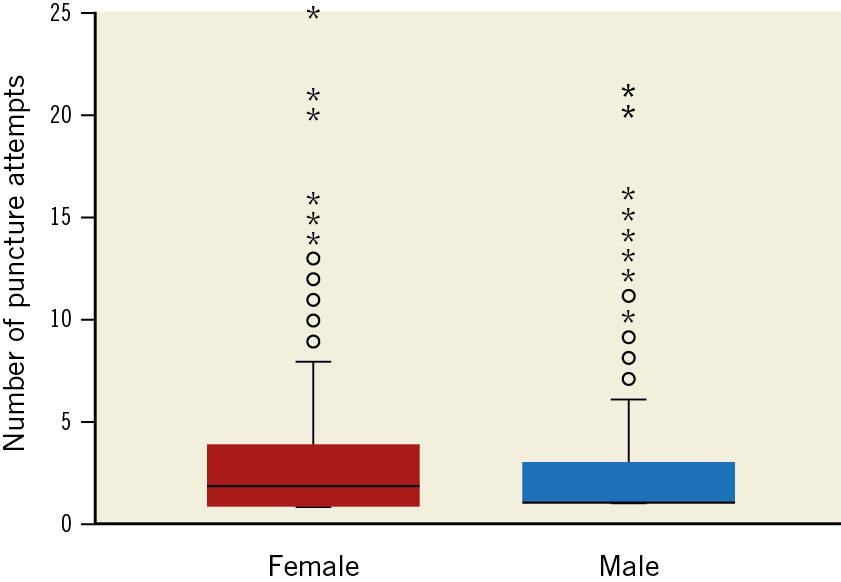
Figure 5. Number of puncture attempts in females and males.
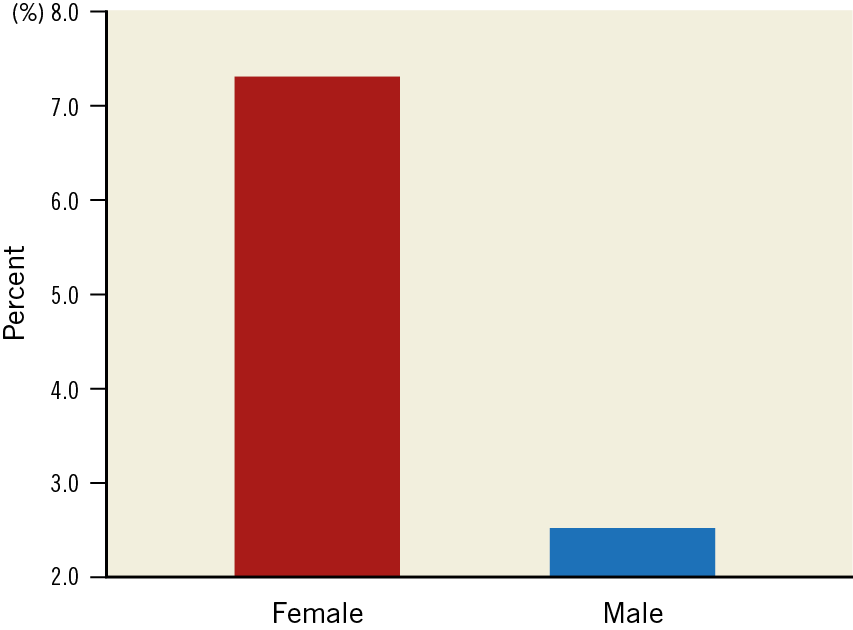
Figure 6. Cannulation failure rates in females and males.
Hypertension had no effect on radial artery diameter or cannulation failure rates. Those with hypertension did, however, have significantly more radial artery puncture attempts than those without hypertension (p=0.047), with the median number of attempts being two in those with hypertension and one in those without hypertension.
Diabetes had no effect on radial artery diameter or cannulation failure rates. Diabetes mellitus was associated with more radial artery puncture attempts (p=0.038).
Dyslipidaemia had no effect on radial artery diameter or cannulation failure rates. Dyslipidaemia was associated with more radial artery puncture attempts, with a median number of attempts of two in those with dyslipidaemia and one in those without dyslipidaemia (p=0.025).
Age, serum creatinine, smoking and body mass index had no effect on radial artery diameter, number of puncture attempts or cannulation failure rates. Twenty-three percent of patients had undergone a previous angiogram. This was not associated with a difference in radial artery diameter, number of puncture attempts or cannulation failure rates.
Discussion
Transradial coronary angiography has become the standard access route in many centres throughout the world. However, gaining access is more challenging than the transfemoral approach.
The use of PO-FMD to dilate the radial artery prior to cannulation has proved to be an easily performed technique that improves access success, with a reduction in the number of radial artery puncture attempts, decreased cannulation failure rates and reduced cannulation times. PO-FMD reduced the local complication of radial artery pulsation loss post cannulation.
The technique is non-invasive and needs no specialised equipment. PO-FMD cuff inflation can be started prior to the patient entering the catheterisation laboratory and released as draping is completed, and need not delay procedural start times, making it a feasible option in a busy cardiac catheterisation laboratory. The use of PO-FMD is therefore an important consideration to augment radial artery access. While we were concerned about patient discomfort due to cuff inflation, PO-FMD was remarkably well tolerated with no patients asking for the cuff to be removed. We do not foresee this being a limiting factor to its use if the technique is explained to patients.
Access success in transradial coronary angiography was high in this study, with failure rates of 2.7% and 5.8% in the PO-FMD and sham PO-FMD groups, respectively. Access failure is, however, highly variable between centres with rates from <1% to >10% reported in different centres8,20,21,22. We foresee PO-FMD’s greatest utility to be in those patients with a high-risk profile for access difficulty and with inexperienced operators, assisting in the steep learning curve of perfecting the technique. The risk factors for access difficulty identified in this trial were female gender, smaller radial arteries, hypertension, diabetes mellitus and dyslipidaemia.
The difficulty in cannulation in females may be related to their smaller radial arteries. Why hypertension, diabetes mellitus and dyslipidaemia lead to more puncture attempts is less clear. A possible explanation may be that the radial arteries of these patients are more sensitive to developing spasm induced by the surrounding tissue trauma or that underlying atherosclerosis makes these vessels more difficult to cannulate.
PO-FMD should also be effective in augmenting radial artery access or puncture in other settings such as arterial line placement for invasive blood pressure monitoring or arterial blood gas sampling but that will need to be investigated in those settings.
PO-FMD did not prevent RAS. This may be due to the fact that spasm mostly occurs not while cannulating the vessel, but after completing cannulation of the vessel when the guidewire is being passed. By the time the guidewire is being passed, the dilatation induced by PO-FMD may have worn off.
A reduction in RAPL was demonstrated. This finding is important in this group of patients where an absent radial pulse or occluded radial artery would prevent future transradial coronary angiograms and may prevent the vessels being used for coronary artery bypass graft (CABG) or fistula creation in the future. None of our patients had any ischaemic complications from the RAPL or RAO.
Although not demonstrated in our data, an association between the number of puncture attempts and RAO and RAPL has been found in another study15.
Local access-site complications were lower than expected from rates reported in the literature8,23,24. RAPL occurred in 1.4% in the PO-FMD group and 3.8% in the sham PO-FMD group. RAO occurred in 3.9% in the PO-FMD group and 5.7% in the sham PO-FMD group. All RAO were caused by thrombus formation. These low rates were probably achieved due to few cannulation attempts, the use of intravenous heparin after cannulation, as well as a strict patent haemostasis protocol.
Study limitations
It is a strength of this study that the cardiologists performing angiography were blinded to the radial artery size measured by ultrasound and to the preprocedural intervention (PO-FMD vs sham PO-FMD) prior to gaining radial artery access. However, patients were aware if the blood pressure cuff was inflated or not prior to radial artery cannulation. It is possible that some of the patients could have made comments during the procedure about the inflation of the blood pressure cuff, alerting the cardiologist to the fact that the patient was in the one group or the other. Patients undergoing coronary angiography in our unit routinely receive pre-medication; none of the investigators could recall a case where the patient provided information that could have unblinded the investigator. The post-procedural assessment of the radial artery for RAPL and RAO was not blinded. To minimise bias, all ultrasound assessments were recorded, and cases of RAO were reviewed and confirmed by a second observer.
The degree of dilatation induced after PO-FMD was not evaluated in this study. This would have delayed the time from dilatation to transradial access and, as the dilatation achieved is transient, this delay could not be accommodated in the protocol. The study was based on the known phenomenon of nitric oxide-independent dilatation of the arteries in the forearm following prolonged occlusion and hence quantifying its presence in this study was not considered essential. This limitation would have been important in a negative trial but, given the beneficial effect of PO-FMD on the number of puncture attempts, cannulation success and RAPL, the concern about this potential limitation has been minimised.
Conclusions
This study demonstrates that, in units proficient in the transradial approach to coronary angiography, access success can be improved with decreased cannulation failures, puncture attempts and complications reduced with less RAPL by a simple and practical measure inducing PO-FMD of the radial artery prior to radial artery puncture. Overall success of transradial coronary angiography is, however, high. We foresee the greatest benefit for the use of PO-FMD in patients at risk of access failure.
|
Impact on daily practice Use of PO-FMD prior to radial artery puncture in patients undergoing transradial coronary angiography can be implemented without prolonging the procedure and will result in fewer cannulation failures, fewer puncture attempts and a reduction in RAPL. Overall success of transradial coronary angiography is, however, high. We foresee the greatest benefit for the use of PO-FMD in patients at risk of access failure. |
Acknowledgements
Tonya Esterhuizen, a consultant at the Biostatistics Unit within the Division of Epidemiology and Biostatistics, Stellenbosch University, assisted with the design and analysis of this study through support from the Faculty of Medicine and Health Science’s Dean’s Fund.
Funding
The study was funded by the Research Fund of the Division of Cardiology, Department of Medicine, Stellenbosch University.
Conflict of interest statement
The authors have no conflicts of interests to declare.
Supplementary data
To read the full content of this article, please download the PDF.