Abstract
Coronary artery bypass grafting (CABG) is the most effective revascularisation treatment for advanced coronary heart disease. Atherosclerotic disease may compromise graft patency in the follow-up. As a result, it is not unusual for patients to present with angina requiring evaluation. When present, graft disease or progression of the disease in native vessels can be treated by means of percutaneous coronary intervention (PCI) or by repeated bypass surgery. The utility of modern helical ultrafast multidetector computed tomography (MDCT) in the evaluation of the patency of arterial or vein coronary grafts and thereby avoiding the need of a coronary angiography (CA) in the majority of patients is well established using 16 or 64-slice scanners. Although the accuracy of MDCT in the study of native coronary vessels in operated patients is more challenging, modern multislice computed tomography technology (64-slice) is especially useful in the non-invasive evaluation of patients with previous CABG with chest pain or equivalent symptoms, but with inconclusive or contradictory results in exercise or pharmacological stress tests. MDCT emerges as an attractive imaging technique, not only in the study of symptomatic patients with previous CABG, but also in the planning of secondary revascularisation procedures, either percutaneous, surgical or hybrid procedures.
Introduction
Coronary artery bypass grafting (CABG) is the most effective revascularisation treatment for advanced coronary heart disease. Nonetheless, atherosclerotic disease may compromise graft patency in the follow-up. Saphenous vein grafts (SVG) have the highest prevalence of significant stenoses. In contrast, 90% of arterial grafts are patent at 10 years and their use has an important impact on survival.1
Soon after surgery, and during follow-up, it is not unusual for patients to present with symptoms, most commonly angina or dyspnoea with effort, which may require evaluation of patency of the grafts. Although tests for detecting ischaemia (i.e. exercise ECG, perfusion or stress echocardiography) may be sufficient for this purpose, it often is necessary to perform a coronary angiography (CA) to demonstrate graft patency or to confirm the presence of severe stenotic injuries, both in grafts and in the native vessels.2,3
When present, graft disease or progression of the disease in native vessels can be treated by means of percutaneous coronary intervention (PCI) or by repeated bypass surgery (REDO) if sufficient harvestable grafts are available. In Europe, around 7% of total CABGs performed are REDO. Mortality and morbidity are increased in REDO when compared to first time CABG in matched patient cohorts. REDO patients also had a significantly higher incidence of incomplete myocardial revascularisation that could explain the worse late outcome.4 Another potential cause of poor outcomes may be damage during re-sternotomy of a patent internal mammary artery (IMA) grafted to the left anterior descending coronary artery (LAD) or to a patent saphenous vein grafts.5
Since the initial application of non-invasive computed tomography (CT) to coronary angiography, the analysis of graft patency has been of great interest due to the difficulties that may be encountered during invasive angiography (difficulty inflating grafts; poor opacity, incomplete imaging of all grafts) and the potential impact on clinical decision making. The utility of modern helical ultrafast multidetector computed tomography (MDCT) in the evaluation of the patency of arterial or vein coronary grafts, thereby avoiding the need of a CA in the majority of patients, is well established using 16 or 64-slice scanners.6-8 A little more limited is the accuracy of MDCT in the study of native coronary vessels in operated patients due to technical limitations and the characteristics of coronary anatomy in CABG patients. In spite of these limitations, MDCT emerges as an attractive imaging technique, not only in the study of symptomatic patients with previous CABG, but also in the planning of secondary revascularisation procedures, either percutaneous, surgical or hybrid procedures.
The multidetector CT protocol in CABG patients
The basic principles and scanning protocols using MDCT in patients with previous CABG is similar to the evaluation of non-operated native coronary arteries.9 Graft visualisation is less affected by motion artifact due to the cardiac cycle than the native vessels. However, heart rate control is crucial to improve spatial and temporal resolution when using the current standard of 64-slice MDCT.10 Therefore, if the pulse rate is above 65 beats per minute, it is recommended the use of beta blocker drugs (i.e. propranolol, atenolol or metoprolol) to decrease it.
New developments, such as dual source MDCT allow performing the scan with hear rates up to 90 bpm, avoiding the need of previous beta blockade.11 Knowledge of the prior surgical procedure is important to define the correct anatomical volume of the scan. For example when LIMA or right internal mammary artery (RIMA) grafts need to be evaluated, the scan field must include their origin from subclavian arteries, whereas if only saphenous vein grafts were used, the scan could start from their origin in the mid-ascending thoracic aorta. Adherence to these recommendations reduces scanning times thereby reducing radiation and increasing patient compliance with prolonged breath-hold, the latter of which can be difficult for patients with CABG as they often are elderly.8 The performance of previous non-contrast scan allows the evaluation of extra-cardiac pathology, for instances pulmonary, pleural or mediastinal diseases but also detecting areas of high attenuation secondary to surgical manipulation which could be misleading as contrast extravasations with iodine acquisition.12 This also increases radiation dose.
The start of the contrast enhanced scan can be triggered by tracking the arrival of contrast in the ascending aorta or is determined by calculating the time delay with a preliminary test bolus of a small volume of contrast agent to measure the transit time. In patients with previous CABG, a longer pre-defined delay is required from the arrival of content in the aorta to the start of the scan when compared to native vessel scan. The additional delay is critical to ensure the complete content opacification of the vein grafts and distal native vessels. For a similar reason, a larger volume of iodated contrast is required in post-CABG examinations due to the slower transit time and longer scan field. Whereas native coronary arteries 64-slice MDCT coronary angiography only uses around 75 ml, in post-CABG patients around 100 to 125 ml of contrast are needed.8
Although the improvement of the temporal resolution with modern 64-slice MDCT has decreased scan times, post-CABG studies require a relatively long-breath hold. The duration of the apnoea required in patients with LIMA grafts is approximately 20 seconds.13 Explanation to the patient and breath-hold training improves image quality. The slice collimation is determined by volume scan and number of slices per rotation. In larger volume scans, e.g. in patients with LIMA grafts, it is necessary to use 0.75 mm slice thickness in 16-slices CT, instead with 64-slices CT the whole course of conduit could be evaluated with 0.5-0.625 mm collimation. The relation between table speed and slice collimation is named “pitch”. Pitch has to remain constant throughout the scan. Pitch in 64-slice CT angiography has an average value of 0.3 and it is dependent of heart rate.14
Retrospective ECG gating is essential to get the necessary accuracy in CT angiography with synchronised imaging reconstruction. Phase reconstruction is adjusted to R-R interval duration in the ECG. Our protocol includes two fixed phases: 40% of the previous RR interval (end-systolic phase) and 75% of the previous RR interval (end-diastolic phase). If present, premature beats are eliminated through editing by the ECG and replacing the suppressed beat for a mirror beat in the sinus rhythm. When artifacts preclude a diagnostic analysis, additional reconstruction from the raw data at 10% steps of the RR interval are performed.
Post-processing techniques allow evaluation of the grafts and coronary native vessels (Figure 1, 2). A first review of the stacked axial images allows identification of vessel narrowings that can be examined further. Multiplanar reformatting (MPR) with maximum intensity projections (MIP) and varying the slice thickness from 0.6 to 2.5 mm improves qualitative evaluation of graft patency and stenosis (Figure 3, 4, 5). LIMA or RIMA and SV left-sided grafts can be explored in modified axial and lateral cut-planes. In contrast, right-sided grafts running in the AV groove, usually require modified coronal and lateral cut-planes. Advanced curved planar reconstruction (CPR) allows the visualisation of the entire graft as a straightened vessel in two orthogonal planes (Figure 6). Advanced post-processing tools offered by the different vendors allow the quantification of the stenosis, both in one-dimensional (lumen diameter) or two-dimensional (cross sectional area) perspectives. The accuracy of advanced quantification, although very promising, has not been clinically validated. This is limited by the spatial resolution of MSCT (0.5 x 0.5 mm). Finally, volume rendered images are three-dimensional reconstructions which could help to assess proximity of bypass grafts to the chest wall, occluded bypass grafts in preoperative evaluation of patients with prior cardiac surgery, with a view to planning REDO CABG.8,14
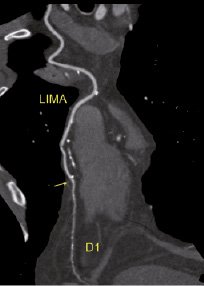
Figure 1. 64-row MDCT acquisition post-processed with curve planar reformatting. Left internal mammary artery is displayed throughout its course in the anterior thorax to its anastomosis with the first diagonal branch. The arterial graft is patent and there are no lesions. The native vessel has a small lumen diameter (1-1.5 mm) and minor injuries with fine calcification.
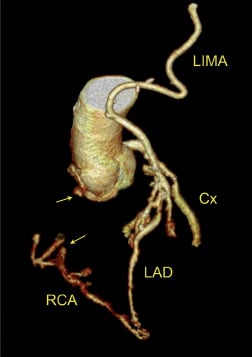
Figure 2. Three-dimensional or volume rendered image acquired with 64-slice MDCT. Coronary lumen is automatically traced using a vendor proprietary algorithm. The lumen of the coronary arteries and grafts are extracted. Note the route of a left mammary artery graft (LIMA) to its anastomosis sequentially to the first diagonal branch and the middle segment of the left anterior descending artery (LAD). There is also an occlusion of the proximal segment of the right coronary artery (RCA). The distal RCA is filled through collateral circulation from the LAD and the posterior descending branch of the right coronary artery. Cx: circumflex coronary artery.
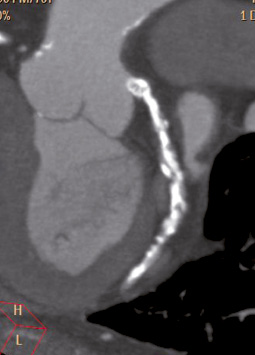
Figure 3. Modified coronal view using Multiplanar reconstruction (MPR) with maximal intensity projection (MIP) of the original axial stack depicting the native left circumflex artery (LCA). The patient had a previous CABG with LIMA to LAD and SVG to OM1, COPD and dyspnoea and chest discomfort with effort. The SVG to the OM1 was occluded. Note the very thin and calcified native LCA.
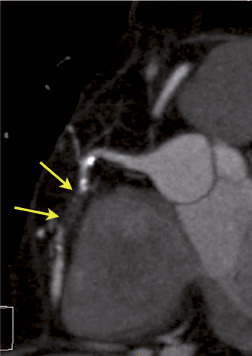
Figure 4. Modified lateral view with MPR and MPI reconstruction of the axial stack acquired with 64-row MDCT. There is an occlusion in the mid-segment of the right coronary artery. The distal replenishment suggests collateral circulation. A marginal branch exists immediately after the end of the occlusion. The length is short and the burden of calcium is low. It is quite straight, without bends. All these features suggest that the occlusion is amenable to percutaneous crossing and potential stent placement, if indicated.
 ,
,
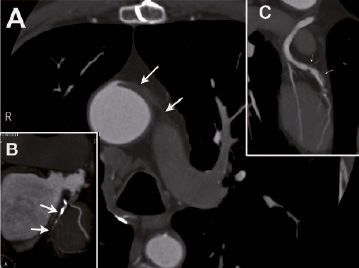
Figure 5. Composition of multiplanar reconstruction (MPR) with maximal intensity projection (MIP) in a patient with refractory angina and previous CABG (fifteen years ago). Central panel discloses an occluded left-sided saphenous vein graft (SVG) to the LAD. Note the LIMA is at its original location in the chest wall. Panel B exhibits left circumflex artery, with marked negative remodelling and calcification, occluded in the mid-segment. There is a patent SVG towards OM2. Finally, panel C discloses a SVG to a diagonal branch with two serial severe stenoses. The native coronary artery parallel running to diagonal branch is an intermedius ramus.
 ,
,
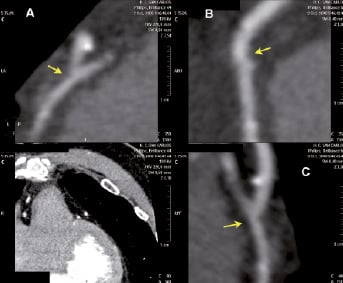
Figure 6. Segmental curved plane reformatting (CPR) at the distal anastomosis of LIMA with mid LAD suspected to have a significant lesion. Panels A, B and C show planar orthogonal views of the segment of interest. The remaining panel shows the reference point. A surgical clip very close to the anastomosis does not affect the lumen evaluation since CPR laterally displaced it. There is mild lesion in the native vessel, immediately after the anastomosis (arrow).
Multidetector CT in current clinical practice
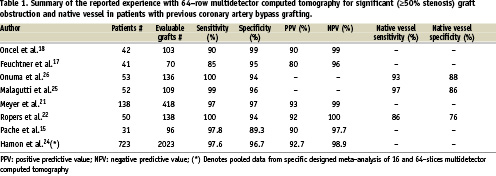
During recent years, several studies have demonstrated the high diagnostic accuracy of MDCT in the evaluation of CABG patients in comparison with the current gold standard: invasive coronary angiography (CA). Limitations of MDCT are that diagnostic images cannot be obtained in a proportion of patients, especially if using 16-slice MDCT, but also for 64-slice MDCT. Overall, MDCT has a sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) very close to 100% for graft patency, whereas accuracy for the detection of graft stenosis varies among different series. Table 1 summarises the published studies using 64-row multidetector computed tomography in patients with previous CABG.15-18
Graft patency is classified as patent with no lesions, occluded or stenosed with either significant stenosis (>50%) or no significant stenosis (<50%). The analysis could be done per patient, per graft or per segment basis. The examination of the grafts early post-surgery (median of 34 days) has an excellent accuracy for graft occlusion secondary to thrombosis, SV graft attrition or arterial spam. NPV achieves a value of 100% in both SVG and LIMA, making of MDCT a valuable technique for ruling out early graft occlusion and avoiding the need of CA.19
In the follow-up studies, almost all examinations were indicated because of complaints of angina or dyspnoea at effort. Although 16-slice MDCT was very promising one month after CABG,20 the advent of 64-slice MDCT is considered as the standard scanning technology for coronary purposes, with high diagnostic accuracy up to a sensitivity of 97.8 -100%, specificity of 89.3-98.7%, PPV of 75-98% and NPV 97.7-100%. The evaluation by two different observers with different experience showed very good kappa values of 0.93 for graft patency and 0.74 for graft stenosis evaluation.14,16,20-22
Nonetheless, we must keep in mind several limitations, both technological and patient dependent, which affect the diagnostic accuracy and constitute a real challenge during the evaluation of patients with previous CABG. The level of accuracy seen in graft evaluation is not achieved when evaluating the distal run in the native vessel, or the evaluation of native coronary vessels to rule out progression of the disease in non-grafted territories. Very poor results were observed with 16 slices scans, because nearly 30% of the native coronary segments could not be evaluated.23 The scenario is more optimistic with the use of 64 slices MDCT,24 because the distal anastomosis is of poor resolution only in 17% of segments due to artifacts, metallic clips or calcification. When segments affected by poor image quality are included in the analysis, the specificity and the positive predictive value decrease only around 5 to 6% compared to when they are excluded. The evaluation of native coronary vessels is reported in only a small number of studies. Native vessels are not evaluable in 9% of cases in a segment based analysis and the distal run-off of vessels in only 7%. The diagnostic accuracy reported for native vessels and distal run-off is as low as 78% and 90% respectively, reflecting the challenging nature of native vessel visualisation in post CABG patients.22,25,26
All imaging specialists, cardiologist or radiologists working with CT coronary angiography agree that negative remodelling with small native vessels and blooming caused by dense calcification in the coronaries as the most important impediments regarding diagnostic accuracy of MDCT in post CABG evaluation.27
Secondary revascularisation: the role of multislice CT
The number of patients previously revascularised requiring secondary revascularisation, either PCI or REDO, is increasing. In Europe, around 8-12% of patients admitted for PCI have had previous CABG. These patients will require PCI on SV grafts in 4% and PCI in protected stem left coronary arteries in 1.5%.28 MDCT may facilitate management in these patients. For example, patients with angina and severe left ventricular dysfunction are at high risk of pulmonary oedema or acute renal insufficiency as consequence of large amount of iodine contrast. MSCT derived data may facilitate planning and anticipation of potential difficulties of secondary PCI which may help to reduce these risks.29
Several groups have reported on the value of MDCT in planning redo surgical procedures, in particular by identifying pre-operation those cases with a very short distance between the right ventricle and the sternum or with a surgical conduit crossing the sternal midline. In such patients, alternative surgical approaches could be considered, including initiating cardiopulmonary bypass before sternotomy or the performance of non-midline sternotomy. The adoption of such preventive surgical strategies, triggered by MDCT-derived information, may significantly reduce the number of complications and the risks of complex REDO.30,31
Re-operative CABG is effective in alleviating symptoms, but has an increased operative mortality and morbidity.32 In order to minimise these risks, minimally invasive surgery could be considered, but, overall, PCI has emerged as the preferred revascularisation strategy.33,34 PCI is used more often than REDO. Nowadays, drug eluting stent (DES) implantation offers comparable long-term mortality and major adverse coronary and cardiac events (MACCE) rates to CABG patients.29 SVG PCI with stents and adjunctive pharmacotherapies is associated with favourable outcomes. PCI of IMA grafts can be performed safely with high procedural success and excellent short- and long- term results. However, stenting at the anastomotic site of arterial conduits is associated with poor results.35,36
Atherosclerotic disease progression occurred more often than failed revascularisation in CABG-treated patients with jeopardised myocardium and angina recurrence.3 An example of the benefits of secondary revascularisation in CABG patients is the treatment of chronic total occlusions (CTO). A large proportion of patients with CTOs treated with PCI have had previous CABG. Successful revascularisation of a CTO by PCI may be associated with increased survival.28,37 However, despite improvements in techniques and materials, the CTO recanalisation success rate is still suboptimal and has not improved over time in the stent era.37 The final decision as to the optimal revascularisation method in patients with CTO and previous CABG is dictated by anatomical considerations more than by clinical variables.38 For example, the retrograde approach to the percutaneous treatment of CTO may significantly increase the success rates. However, retrograde PCI via a bypass graft or epicardial collaterals can potentially result in severe complications.39 MDCT can facilitate planning and evaluation of appropriateness of the percutaneous approach by anticipation of potential difficulties and visualisation of the features associated with reduced success. This may include the visualisation and quality of the distal vessel, the type of entry point to the occlusion, tortuosity and total length of the occlusion and burden of calcium at the occlusion and neighbouring segments. Good quality collateral supply through septal branches can be depicted using MDCT, facilitating the planning of a retrograde approach.40,39
The increasing use of primary PCI with stenting as the treatment of choice in acute coronary syndromes has increased the use of the hybrid approach. The hybrid approach consists of minimally invasive coronary artery bypass grafting with a single internal mammary artery and with the remaining coronaries revascularised percutaneously with one or more bare metal or drug eluting stents.41 As a result, when symptoms occur in such cases, not only grafts must be evaluated, but also the stent or stents. The improvement of MDCT technology (64 slices, dual source, z-spot movement, etc.) and stent design have allowed improved visualisation and evaluation of the coronary in-stent lumen. Nonetheless, diagnostic accuracy is sufficiently flawed (i.e. sensitivity 89%, negative predictive value of 90% in selected population) as to discourage the use of MDCT exclusively for this purpose.42 Further developments, mainly fine cell detector (0.3 mm collimation) and whole heart scanning with 256 and 320 slices MDCT may overcome these limitations for stent evaluation.
Limitations
Almost all MDCT studies have been criticised due to selection bias. Recent published prospective and well designed trials have confirmed the very promising future of MDCT in the diagnosis or exclusion of coronary disease in unselected patients. However, invasive coronary angiography by MDCT cannot be replaced.43,44 Studies of patients with previous CABG are more limited, and are likely to be affected by selection bias which may overestimate diagnostic accuracy. As expected, all the series excluded patients with contrast allergy, unstable haemodynamic situations or severe renal insufficiency. Arrhythmia, mainly atrial fibrillation, but also premature beats, are an important limitation to perform high quality and efficient scans. The long lasting course of coronary heart disease in patients with CABG, along with the very frequent presence of left ventricular systolic dysfunction, increases the prevalence of arrhythmia and often precludes the use of MDCT. In a similar way, in patients in sinus rhythm, the best spatial resolution demands an optimum heart rate control (≤ 65 bpm). This is usually achieved by using beta blockers, but these drugs are sometimes contraindicated. Ongoing developments (i.e. the use of ionic current inhibitors such as ivabradine) would overcome these limitation.
Some limitations are inherent in MDCT. For instance, MDCT is not able to establish retrograde or competitive flow due to lack of selective arterial enhancement.14,16 But, probably, the most important disadvantage in evaluation of patients with previous coronary artery bypass grafts are caused by the CT effect of partial volume artifact. Partial volume artifacts occurs when high attenuation material (calcium, metallic surgical clips or stents) is included in the image and as a result of excessive blooming way above the lumen. Time consuming post-processing (multiplanar or curved reconstruction) may allow evaluation of the lumen, but sometimes is really impossible.
Conclusion
Modern multislice computed tomography technology (64-slice) has demonstrated a high diagnostic accuracy in assessment of venous and arterial grafts, with a negative predictive value near 100%, both in the early and late postoperative period. MDCT is especially useful in the non-invasive evaluation of patients with previous CABG and chest pain or equivalent symptoms, but with inconclusive or contradictory results in exercise or pharmacological stress tests.45 The constant increase in secondary revascularisation for both PCI and cardiac surgery makes MDCT a very promising imaging for planning as well as anticipating potential difficulties in PCI. This may be especially true in the percutaneous treatment of total chronic occlusion and for planning minimally invasive surgical procedures by depicting anatomic relations of chest wall with patent grafts and the IMA. In addition, MSCT allows establishing histological characteristics of atherosclerotic plaques (calcified, fatty or fibrous) which could help in preprocedure planning of site of stenting or graft anastomosis.46
The technical evolution of MDCT, with very fine collimation through the use of very small detectors and improvement in temporal resolution (up to 45 ms or less) will strengthen the role of this cardiac imaging technology in the evaluation after CABG and the performing of secondary revascularisation.
Acknowledgement
We are indebted to our colleagues, cardiologists and radiologists, the nurses and technical radiology assistants for their expertise and commitment to working together for an excellent cardiac computed tomography service.

