MSCT misadventures
My last misadventure with multislice computed tomography (MSCT) was in a delightful 83 years old man. He was supposed to have a 50-70% stenosis of the proximal RCA in a MSCT done five days before, and here I am faced with a bad chronic total occlusion (CTO) at the wrong time of day in a setting where I do not have available the usual armamentarium of CTO recanalisation: dual injection, dedicated wires, microcatheters, 7-8 Fr guiding catheters. After an angry phone call to the radiologist, who reported the test, I received the maximum intensity linear reconstruction showing dense calcification in the proximal segment of the RCA and no contrast visible for 3 cm. The second segment was diseased, but had no calcium and an obvious patent lumen. With angiography I was unable to follow the collateral flow beyond the third segment of the RCA. The MSCT was poorly interpreted, but the images were incredibly helpful, giving me the confidence for planning a second recanalisation procedure.
Every cardiologist can tell similar or worse stories about MSCT, especially a few years ago when the resolution was lower and the motion artefacts more prominent. Still, in this case, the technique offered information my best angiogram was unable to provide –and they were provided non-invasively– prompting an angiography and angioplasty procedure which was effectively needed and was facilitated in its planning by MSCT.
MSCT technique: a truly exponential growth
Two or three years ago we were more reluctant to have a large added radiation burden when there was a high likelihood a PTCA was needed, and we were forced to exclude many patients with tachycardia; difficult to control pharmacologically or unable to have a good breath-hold. The recent technical progress of MSCT has been amazingly fast, with improved temporal and spatial resolution coming together with a much lower radiation burden of 1-5 mSv. Thanks to improved gantry rotation times, larger detector arrays (i.e., shorter scan times), improved detector technology and more sophisticated reconstruction algorithms (e.g., iterative reconstruction), cardiovascular MSCT is no longer a developmental research tool, but has become a clinically robust diagnostic modality instead1. Techniques such as ECG-tube current modulation in low pitch spiral scanning, sequential scanning and high pitch spiral scanning (a technique in which data are acquired by gating a single diastolic interval), allow consistent reductions in x-ray radiation exposure. Customised scan parameters (e.g., decreased kilovoltage) permit to further decrease exposure in patients with low body mass index, without compromising image quality and diagnostic yield. New technical developments, currently under investigation, include dual energy scan modes that may enable dose-efficient myocardial tissue characterisation (e.g., scar imaging) and first-pass and dynamic perfusion imaging.
How to promote widespread application of MSCT
Why is MSCT not picking up as much as it should, and why is it sometimes more popular among GPs and surgeons than cardiologists? Few people dare speaking about it, but the answer is clear: ownership. Every cardiologist is familiar with echocardiography, confident that the test will be performed by colleagues or dedicated technicians aware and respectful of the needs of critically ill cardiac patients, and will be able to directly review all images in their PC and easily discuss results, if needed. Most often, cardiac MSCT scanners are located and controlled in radiology departments with a prevalent low risk outpatient population. Here, the MSCT is carried out by personnel not used to dealing with patients with severe coronary artery disease and rarely interpreted by dedicated cardiac imaging specialists well aware of the specific needs of the clinicians referring the patients they study. Nuclear cardiology was also in a similar situation, and this prevented, for a long time, its wider utilisation. The worst move, from interventional cardiologists, would be to oppose the natural expansion of a technique which is able to offer, non-invasively, direct information on the coronary anatomy. Don’t forget our history: interventional cardiology grew –and continues to flourish– out of the desire of patients to receive a less or minimally invasive treatment compared with surgery. Patients and their referring physicians need certainties, and the negative predictive value of a truly normal coronary angiogram with MSCT (no calcium, arteries well followed up to the distal branches with no artefacts) is unbeatable by any other non-invasive provocative test. Calcium was, and remains, the cause of most of the mistakes in interpretation, most often overestimating the severity of moderate calcific lesions. At the same time, the exquisite sensitivity in calcium detection is a strength, allowing the technique to be used (calcium score, without angiography) as an effective screening method, as well as to detect angiographically invisible calcium which can predict the response to angioplasty, be a key predictor of success and help planning of CTO recanalisation procedures.
The worst mistake from radiologists would be to fail to engage cardiologists in the common review and interpretation of non-invasive coronary angiography with MSCT. Radiologists can learn the objective difficulties posed by poor acquisition or excessive calcium load, helping cardiologists to better select and prepare the patients referred. They can understand the degree of confidence with which the diagnosis of presence or absence of significant lesions can be given, helping cardiologists to decide the next steps based on the full picture which includes patients’ symptoms and history and the results of other tests: straight to angiography, additional non-invasive tests, pharmacological treatment or full reassurance and no treatment. It is difficult to envisage a radiologist proficiently adding cardiovascular MSCT to the already wide array of applications of conventional radiology, ultrasound, invasive arteriography, magnetic resonance and MSCT in all other body districts. This is not the direction we have successfully moved in cardiology, where sub-specialisation has become a standard in training: we should expect the same attention to the complexities and subtleties of cardiovascular imaging from our radiology colleagues. My co-author for this paper, a trained radiologist, spent four years working exclusively in cardiac MSCT in the radiology department of the Erasmus Medical Center at Rotterdam, maintaining close links with the cardiology division, with a tradition of radiology and cardiology specialists and trainees working together to foster research and extract the maximal clinical information.
Training in cardiac MSCT: clear guidelines in the united states, variable practices in Europe
The cardiovascular MSCT study is an operator-dependent procedure in which it is possible to introduce confounding artifacts or omit data of diagnostic importance. Operator’s skills and experience are of paramount importance during both phases of image acquisition and image interpretation. Accurate patient preparation and instruction, choice of contrast injection protocol and optimisation of the scan technique are mandatory requisites to obtain optimal image quality and minimise patient’s radiation exposure. The PROTECTION I study2, a multicentre observational trial of 50 sites performing cardiac MSCT, showed that increasing operator experience was associated with significant reduction in patient’s x-ray radiation exposure (1% decrease in exposure per each year of experience). The operator’s knowledge of tomographic anatomy, his/her ability to distinguish between reliable and unreliable data (e.g., recognition of breath-holding, gating, arrhythmias as sources of artefacts) and to manipulate planar views into a three-dimensional framework will maximise the diagnostic yield of the study.
In the United States, the Society of Coronary Angiography and Interventions in conjunction with the American College of Cardiology Foundation and the American Heart Association, the American Society of Nuclear Cardiology, the Society of Atherosclerosis Imaging and Prevention and the Society of Cardiovascular Computed Tomography have promoted the preparation of a consensus document3 to define standards for training, accepting the principle that no medical professionals may have all the background needed for the interpretation. The original document was updated a few years later4 to specify recommendations for trainees and fellows. Trainees and fellows are expected to get comprehensive exposure to both acquisition and interpretation of cardiac MSCT throughout their training, and should master the relationship between the results of the MSCT examination and findings of other cardiovascular tests, such as catheterisation, nuclear cardiology, cardiovascular magnetic resonance imaging and echocardiography (when appropriate). In order to achieve this, minimum numbers of cases to be performed and interpreted under supervision and time intervals of training are given as guidelines. Three different levels of expertise are defined (Table 1), and it is suggested that that all fellows should attain at least the first level of training4.
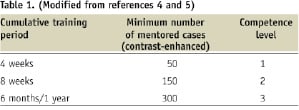
Although this level does not qualify a trainee to perform and interpret MSCT independently, it entails understanding the basic principles, indications, applications, technical limitations of MSCT and the interrelation with other diagnostic tests, which are essential for the appropriate use of cardiovascular MSCT clinical practice. It should be emphasised, that although number of studies and time intervals of training are given as guidelines, these numbers are less important than the depth of understanding and quality of the clinical experience. Recommendations on a number of studies should be taken as “minimum” requirements. It has been shown that case loads and time intervals of training similar to those described in the guidelines may be insufficient to attain highest expertise5. Moreover, although the focus of cardiac MSCT is the detection of cardiac disease, education and training in the recognition of significant non-cardiac findings (e.g., aortic disease, pulmonary emboli, non-benign lung nodules) should be undertaken to ensure the best quality of care.
Trainee evaluation and accreditation
For trainees and fellows enrolled in formal training programs, assessment of technical knowledge and evaluation of overall competence in MSCT are probably best done by direct oversight during interpretation of procedures by the program director and/or expert personnel of the MSCT unit4. It should be recognised how difficult it is to recreate the breadth and intensity of a training fellowship once a physician has assumed full-time responsibilities of a practice setting. Professionals in practice, however, may receive training in their practice settings: there are indeed a number of ways in which physicians can substantiate expertise and competence in MSCT3. In these cases, there are opportunities for accreditation with the American College of Radiologists (Cardiac CT Certificate of Advanced Proficiency)6 and the Certification Board of Cardiovascular Computed Tomography (CBCCT)7. CBCCT candidates are administered multiple-choice electronic tests to be completed on a PC covering clinical indications and limitations of MSCT, scan technique and post-processing, principles of x-ray radiation physics and radiation protection. Albeit comprehensive in terms of background knowledge, these tests do not evaluate some practical abilities involved in cardiovascular MSCT, such as patient preparation and instruction, choice of the most appropriate scan technique, optimisation of contrast injection protocol and scan parameters, manipulation of the three-dimensional MSCT dataset on a workstation to judge the reliability of the data, and, importantly, the reporting of the study. For these reasons, when possible, workplace-based assessment may reflect better the trainee’s acquired competence.
Situation for accreditation in Europe
The European Society of Cardiology encourages the accreditation with the CBCCT8. This probably reflects the relative paucity of training schemes across Europe offering comprehensive multimodality training in cardiac imaging (including cardiac MSCT), so that trainees have to look for training at different facilities when the primary program cannot accommodate them. The European Society of Radiology has identified cardiovascular multimodality cross-sectional imaging as a subspecialty, and has made available a number of training and exchange fellowships to overcome the existing limitations and disparities in the availability of multimodality cardiovascular imaging facilities across Europe9. Some national societies, for instance the British Society of Cardiovascular Imaging, which has members from different backgrounds (but mainly radiology and cardiology), have endorsed training guidelines similar to those published in the United States and also offer opportunities for curriculum-based accreditation10.
How can we develop common European standards?
Our young Association should look with interest at the achievements of our colleagues on the other side of the Atlantic and work in the same direction, involving radiologists, but also the entire cardiology community. If we want to succeed in leaving a door open for interventionalists willing to report MSCT examinations, we have to honestly admit our present limitations. Not only do we represent less than 1/10 of the practising interventional cardiologists in Europe, but few of them are actively involved in running a cardiac/coronary MSCT program. Most of the cardiologists actively publishing and lecturing in this field are not interventional cardiologists, but non-invasive imaging specialists. We must seek their cooperation and support, ensuring an active representation in the Council of Cardiovascular Imaging which currently includes the Echocardiography Association and the Working Groups of Nuclear Cardiology and Magnetic Resonance. A survey of the situation in Europe in order to understand how many MSCT examinations are done, by whom and for which indications, will be an important first step to identify the needs. The second step can be the organisation of dedicated training courses. There are too many repetitive interventional courses or live transmissions performed all over Europe. There are too few occasions of practical training at affordable cost and targeted to interventionalists, with less attention to the already known cardiac anatomy and clinical indications, and more attention to the technicalities of proper acquisition, processing and reconstruction of images. I would personally encourage all young interventionalists to take time off the cathlab routine in order to become proficient in reading MSCT images. As listed above, the current requirements are not taxing and the obstacles are more in the nature of the relationship between radiology and cardiology, with the difficulty of continuing a regular workload of cases under proper expert supervision when the initial training is completed. Young interventionalists should be encouraged to do it, not only because there will be a growing need and this skill can become a powerful addition in their CV to boost chances of achieving high level posts. Involvement in a MSCT programme is also promoting direct contact with patients and referring physicians - helpful to building a practice. Finally, the full knowledge of the complementary information MSCT offers on wall pathology of coronary and peripheral vessels, as well as its precise measurement of cardiac and vascular structural changes, improves their ability to deliver high quality interventional treatment in coronary, peripheral and structural heart disease. If only for this last reason, cardiologists who choose not to formally train in MSCT –probably the majority of the practising cardiologists and interventionalists at present– need to develop the skills necessary for understanding the basics of MSCT and its potential traps. Their knowledge will improve naturally if they can have full remote access to all MSCT images, with regular sessions for common discussion of cases offering the possibility of confront MSCT images and selective coronary angiography, a necessary step to promote cooperation and common growth.
To whom does cardiac MSCT belong?
Not to the cardiologist, not to the radiologist, but to the patient who has the right to have his tests reviewed and interpreted by specialists with complementary skills. We interventional cardiologists should all start to individually promote this cooperation in our clinical practice. We interventional cardiologists should lobby as National, as well as European Associations, to promote meaningful programs of training and revalidation that promote competency in medical professionals of various backgrounds. Ring fencing a new technique will never promote penetration and acceptance of MSCT: in this as well as in most medical fields, teamwork, and not exclusivity, is the key to success.

