The importance of multimodality imaging for structural heart disease interventions was demonstrated during the first decade of transcatheter aortic valve implantation (TAVI) and transcatheter edge-to-edge mitral valve repair (2002-2012)1,2. While cardiac computed tomography (CT) has been critical for patient and device selection, as well as for providing optimal fluoroscopic projections for TAVI, protocolisation of echocardiography was instrumental in providing reproducible results during and after transcatheter edge-to-edge mitral valve repair. Nowadays, cardiac CT and echocardiography play a vital role across a spectrum of structural heart disease interventions (e.g., paravalvular leak closure, ventricular septal defect closure, transcatheter mitral valve replacement, and combined transcatheter valve interventions).
Unlike cardiac surgeons who achieve a direct visualisation of the cardiac structures, interventional cardiologists rely on cardiovascular imaging to guide procedures. Structural heart disease interventions require an integrative approach to cardiovascular imaging by merging data from fluoroscopy, echocardiography and multislice CT. Consequently, structural heart disease interventionalists need to acquire the skill sets of an “interventional imaging specialist” for proper patient and device selection, procedural guidance and device assessment. In fact, lack of proper knowledge of structural imaging or, alternatively, failure to recognise its key role in procedural planning may have detrimental effects on structural interventions and training. Meanwhile, most interventional structural heart disease training programmes remain focused on the technical aspects of procedures while “imaging” is learnt or understood on a case-by-case basis through “osmosis”3. In addition, supervisors themselves often lack competence as structural imaging teachers.
The required knowledge and skill sets span the spectrum of image acquisition, analysis, interpretation and application. Furthermore, understanding the correlation between different imaging modalities is key in accessing the so-called “complexity” of cardiovascular imaging. Accordingly, realising that the left and right heart can be appreciated in one-, two-, three- and four-chamber views, irrespective of imaging modality, might markedly simplify the process of identifying and correlating anatomical structures across imaging modalities4,5 (Figure 1). For example, a three-chamber view of the left heart will have the aortic and mitral valve (and their components) in the same relative orientation regardless of imaging modality (i.e., fluoroscopy, echocardiography, multislice computed tomography, magnetic resonance imaging). In fact, the appearance of heart structures on imaging depends on angle projection rather than on specific imaging modalities.
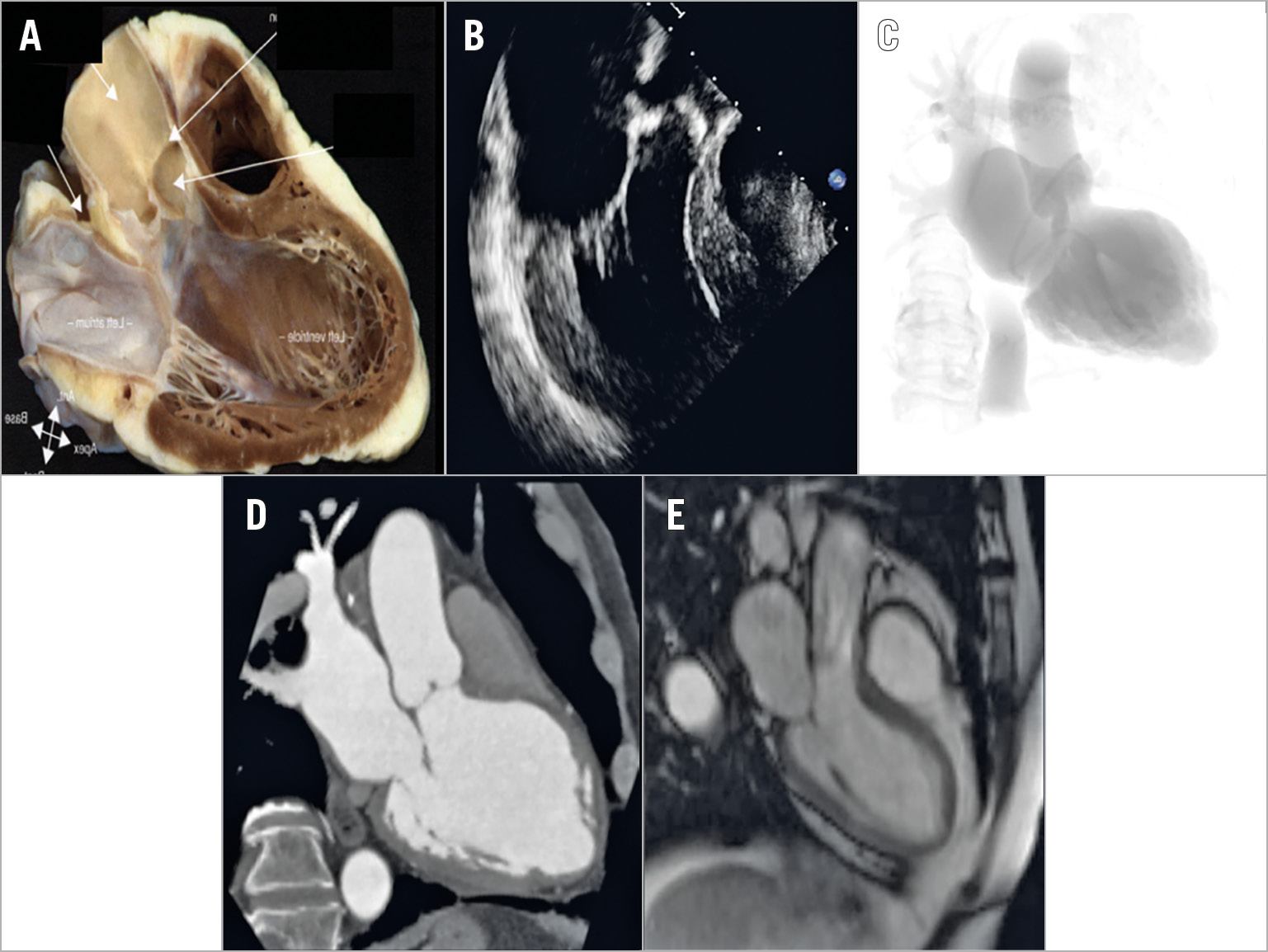
Figure 1. A three-chamber view is demonstrated with a heart specimen, echocardiography, fluoroscopy, computed tomography and cardiac magnetic resonance imaging. How the heart appears is only a matter of viewing angle and not imaging modality.
Developing a common language between the interventionalist and non-invasive imager is imperative, yet challenging6. While localisation of cardiac structures on CT scan and fluoroscopy relies on attitudinal descriptors (i.e., superior/inferior, anterior/posterior, right/left), echocardiography incorporates more relative terms such as medial, lateral and septal that can confuse the interventionalist while navigating catheters and devices according to fluoroscopic images7. The attitudinal description of the heart can be assumed across imaging modalities and can simplify communication between disciplines. Both papillary muscles, for example, can be identified as posterior structures oriented in a superior and inferior orientation, respectively.
A thorough understanding of the attitudinal description of heart structures is necessary for comprehension of structural imaging7. Cardiac structures can subsequently be identified and localised according to chamber views through different imaging modalities. Interestingly, cardiac CT provides a 3D data set of the heart that can be reconstructed in multiple planes and provides an excellent framework to understand the attitudinal orientation of cardiac structures. Cardiac CT can act as the seminal tool to understand fluoroscopic imaging and transoesophageal echocardiography better, the former by performing multiplanar reconstructions from transverse and sagittal projections and the latter by performing multiplanar reconstructions from the viewpoint of the oesophagus.
Despite the increasing interest in interventional cardiovascular imaging, many unknowns remain. By what criteria do we define an interventional imaging specialist? Should there be a joint learning programme between the interventional and the non-invasive structural imaging specialist? Do interventional cardiology fellows undergoing training in structural heart disease require a period (e.g., six months or 12 months) of focused learning in multimodality imaging and/or should there be a minimum number of cardiac CT or echocardiograms to be analysed? Who will be qualified to teach? Will qualified training centres require certification? Should there be certified mediums through which imaging is taught (e.g., seminars, conferences, on-line course)?
Finally, the current editorial focuses on the awareness and knowledge gaps of the interventional imaging specialist. The “eyes” of the Heart Team cannot be complete without those of the non-invasive imaging specialist… two pairs of eyes are better than one!
Conflict of interest statement
N. Piazza is a consultant for Medtronic, Circle Cardiovascular Imaging 42, HighLife, and MicroPort. V. Delgado reports receiving speaker fees from Abbott Vascular and Medtronic, and grants to the institution from Medtronic, Boston Scientific, Biotronik, Edwards Lifesciences, GE Healthcare and Abbott Vascular. C. Hamm is a member of the Medtronic Advisory Board. D. Mylotte has no conflicts of interest to declare.