Abstract
The field of catheter based valve intervention is neither an interventional cardiologist nor a cardiac surgeon’s playground – but rather is a shared space. Optimal clinical outcomes will be obtained by clinicians from both of these backgrounds working collaboratively, not just in planning and decision making but also in the implantation of these devices. This will become even more important as one goes down the spectrum of risk into intermediate or lower risk patient populations.
Introduction
Catheter-based interventions on heart valves have been practised for a long time in the congenital sphere. In the adult acquired population, mitral balloon valvuloplasty is an established technique, particularly in young patients with rheumatic mitral stenosis. There had been a vogue for aortic balloon valvuloplasty but this fell out of favour because of poor mid- to long-term results.
More recently, there has been great renewed interest in catheter-based interventions, particularly to left-sided valves1. Almost all of the associated techniques and technologies require clinicians to learn new skills in terms of valve imaging and assessment, and in implantation of the devices. Conventional training in cardiac surgery and interventional cardiology over the last 20 years or so has not provided any individual group with the complete skill set required. So, should these clinical decisions and interventions be led by clinicians from an interventional cardiology or cardiac surgical background?
Of course, the clear answer is that both should be involved in a collaborative Heart Team approach. I hope to persuade you that both groups of clinicians bring complementary skill sets to enable optimal patient outcomes and the effective and expeditious management of any kind of complication. Such a collaborative approach to decision making (which should also involve other medical and paramedical specialities involved in the care of the patient) is strongly supported in both European and North American guidelines2,3.
Cardiac surgeons have dominated the treatment of aortic and mitral valve pathology over the last 40 years. Their training, therefore, has encompassed great understanding of the pathological anatomy and physiology of these valves and how to deal with these using surgical procedures. Thus, the cardiac surgical community has great experience in decision making regarding the timing of valve intervention and experience in judging the risk involved when any individual patient undergoes conventional surgical treatment of their valve disease.
I will return to concentrate on transcatheter aortic valve implantation (TAVI) but will initially address mitral (and to a lesser extent tricuspid) intervention, which is clearly more complex than simple aortic valve implantation. Various clinical and preclinical technologies are currently emerging, all of which require specific procedural skills. Some (such as Cardioband; Valtech Cardio Ltd, Or Yehuda, Israel) undoubtedly require skills that are probably more compatible with an interventional cardiology background. However, many (such as transcatheter mitral valve implantation4 or transapical neochordal implantation) are probably more appropriately undertaken by clinicians with a cardiac surgical background– particularly since a transapical approach is usually required (and not many interventional cardiologists would be comfortable with that!). Furthermore, a considerable portion of the current clinical activity in the mitral and tricuspid space relates to valve-in-valve or valve-in-ring implantation. Understanding of the original valve and ring, and the technical steps in these procedures is again more commonplace within the cardiac surgical community.
Over the last decade, TAVI has become an accepted standard procedure for the treatment of patients with severe symptomatic aortic stenosis who are at high risk for conventional surgery1. As highlighted above, the decision-making processes leading to the procedure should be undertaken by a collaborative Heart Team. The elephant in the room is – who should perform the implantation procedure?
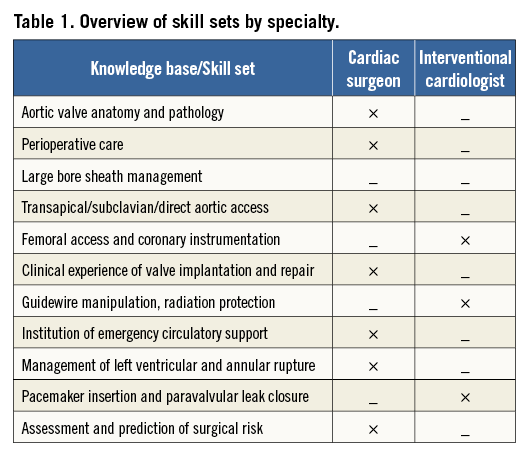
In Table 1, I have highlighted (in a very simplistic way) the skill sets that I believe would be expected in a standard conventionally trained cardiac surgeon and interventional cardiologist (currently from a PCI background). Expertise provided to the implantation process by the cardiac surgeon includes: (i) very detailed understanding of aortic valve anatomy and pathology; (ii) the ability to undertake the procedure via all access routes (femoral, subclavian, direct aortic, transapical and even carotid); and (iii) skill and expertise in dealing with the various complications of TAVI - institution of emergency circulatory support, emergency sternotomy for guidewire-induced left ventricular perforation, annular rupture, etc. The Hamburg group have fairly convincingly demonstrated that the active involvement of a cardiac surgeon (and team) in the implant process facilitates the management of these complications and improves patient outcome5. Conversely, the interventional cardiologist has far greater expertise in femoral arterial access, coronary intervention, pacemaker insertion and emergency pericardiocentesis. However, cardiac surgeons are also familiar with basic guidewire techniques to allow surgical or percutaneous access to the femoral artery for the institution of peripheral circulatory support or intra-aortic balloon pump insertion (although these are clearly not as well developed as in the interventional cardiology community).
Moreover, many of the skills and techniques required for successful TAVI are generic and need to be learnt specifically – CT sizing and procedural planning, management of large bore sheaths and closure devices, and the specific art of safe device delivery into an optimal position. These skills can be effectively learnt by either an interventional cardiologist or a cardiac surgeon – if they are prepared to dedicate time to do so.
The other facet of aortic valve intervention where cardiac surgeons can contribute greatly is during valve-in-valve TAVI procedures. These require very detailed understanding of the design of individual bioprostheses (stented and stentless), the implantation technique for stentless and homograft valves, and a clear understanding of the appropriate sizing and target landing zone6. This knowledge can of course be acquired by the interventional cardiologist but is already held innately by the cardiac surgical community.
To conclude, the field of transcatheter valve intervention is a playground for neither the interventional cardiologist nor the cardiac surgeon in isolation – but rather is a shared space. There is no doubt in my mind that optimal clinical outcomes will continue to be obtained by clinicians from both of these backgrounds working together - not just in planning and decision making but also in device implantation. This consideration will be even more important as we progress the spectrum of risk into intermediate- or low-risk categories where procedural complications will need to be dealt with effectively and expeditiously to produce optimal outcomes. Specific skills need to be acquired by clinicians in both training pathways, and it is essential that professional societies and associations in both cardiology and cardiac surgery come together to define training programmes for individuals who wish to specialise in the structural heart field and catheter-based interventions.
Finally, it is actually great fun and very rewarding to work as a team. There are undoubtedly aspects of knowledge and skill sets that both communities bring to the table – if harnessed together in a collaborative way these undoubtedly lead to the best patient outcomes.
Acknowledgements
To my colleagues in the Heart Team at the Royal Brompton Hospital and specifically to Professor Christophe Nienaber for his input and editing of this manuscript.
Conflict of interest statement
N. Moat is a consultant to Medtronic and Tendyne.

