Abstract
Background: Endovascular therapy is the first-line strategy for femoropopliteal obstructive disease. However, for lesions involving the common femoral artery (CFA) surgical endarterectomy is still the gold standard.
Aims: The aim of this study was to evaluate the safety and efficacy of directional atherectomy (DA) for the treatment of CFA lesions.
Methods: A retrospective analysis of patients who underwent DA of the CFA between March 2009 and June 2017 was performed. The primary efficacy endpoint was the incidence of clinically driven target lesion revascularisation (cdTLR). Secondary endpoints included the overall procedural complication rate at 30 days, change in ankle-brachial index (ABI), and Rutherford-Becker class (RBC) during follow-up.
Results: This analysis included 250 patients. The mean follow-up period was 31.03±21.56 months (range 1-88, median follow-up period 25 months). The procedural complication rate including access-site complications, target lesion perforation, and outflow embolisation was 10.4% (n=26). All but one complication could be treated conservatively or endovascularly. One surgical revision was necessary. Freedom from major adverse events (death, cdTLR, myocardial infarction and major target limb amputation) at 30 days was 99.6%. The rate of cdTLR during follow-up was 13.6% (n=34). A significant improvement of the mean ABI and the RBC was observed. Multivariate logistic regression analysis revealed residual target lesion stenosis >30% (p=0.005), and heavy calcification of the target lesion (p=0.033) to be independent predictors for cdTLR.
Conclusions: The use of DA for the treatment of CFA lesions leads to promising midterm results with an acceptable complication rate.
Introduction
In 2010, the worldwide prevalence of peripheral artery disease (PAD) was estimated at 202 million people. Between 2000 and 2010 the incidence increased by 28.7% in countries with low and middle incomes and by 13.1% in high-income countries1.
Endovascular therapy is the first-line strategy for femoropopliteal obstructive disease2. However, for lesions involving the common femoral artery (CFA), surgical endarterectomy is still the gold standard3. Although satisfactory long-term results can be achieved with surgery, the procedure is associated with noteworthy major complications including redo procedures, wound infections, and nerve damage in up to 13.8% of patients4,5,6.
Several studies have evaluated the technical and clinical outcomes of endovascular procedures for the treatment of CFA lesions7,8,9,10,11. However, sufficient evidence to support endovascular techniques as an equivalent alternative to open surgery is lacking. Directional atherectomy (DA) is an established endovascular procedure for the treatment of femoropopliteal and infrapopliteal lesions12,13,14,15,16,17. Subgroup analyses and a small prospective study revealed promising acute and midterm results of CFA-DA7,18,19. In addition, the reported stenting rates following DA are low, ranging from 3% to 6.5%12,13,17.
The aim of this study was to investigate the safety and the technical and clinical outcome of consecutive patients with atherosclerotic CFA lesions treated by DA with or without additional plain old balloon angioplasty (POBA) or drug-coated balloon (DCB) angioplasty.
Methods
PATIENT POPULATION
A consecutively collected and retrospectively evaluated study was established to register patients who received DA of atherosclerotic lesions of the CFA. Between March 2009 and June 2017, medical records, duplex ultrasound measurements, angiographies and endovascular procedures were examined. This trial was approved by the local ethics committee. Patients with PAD Rutherford-Becker class (RBC) 2 to 5 with a de novo CFA stenosis ≥70% (estimated by duplex ultrasound with a peak systolic velocity ratio of >3.5 and visually on angiography) were eligible for this analysis.
Major exclusion criteria included thrombus within the target lesion, acute critical limb ischaemia, lesions not caused by atherosclerotic disease, PAD RBC 0, 1 and 6, and restenosis or re-occlusion after an endovascular or surgical index procedure.
STUDY ENDPOINTS
The primary effectiveness endpoint was the clinically driven target lesion revascularisation (cdTLR)-free survival rate by Kaplan-Meier analysis. The primary safety endpoint was freedom from major adverse events (MAE) at 30 days including death, myocardial infarction, cdTLR, and major target limb amputation.
Secondary endpoints included the overall procedural complication rate, changes in RBC and ankle-brachial index (ABI). The procedural complication rate included access-site complications, target lesion perforation, and outflow embolisation. The time to TLR and the type of revascularisation (surgery or endovascular procedure) were documented.
STUDY PROCEDURES
DIRECTIONAL ATHERECTOMY DEVICES
The SilverHawk™, the TurboHawk™ and the HawkOne™ directional atherectomy catheters (Medtronic/Covidien, Mansfield, MA, USA) were evaluated for treatment of the CFA. These atherectomy catheters are licensed for commercial use by the Food and Drug Administration and the European Union.
ENDOVASCULAR PROCEDURE
The following index procedure-related criteria were documented: sheath size, type of atherectomy catheter, use of an embolic protection device, additional target lesion procedures (POBA, DCB angioplasty, stenting), and inflow and outflow non-target lesion procedures. Target lesions were evaluated in terms of extent (Supplementary Table 1), degree of calcification by visual estimation (Supplementary Table 2), and residual stenosis post procedure. The degree of calcification was estimated visually and divided into three levels according to our own classification (Supplementary Table 2). The lesion required placement of a 0.014-inch guidewire. Target lesion predilatation, use of an embolic protection device, the number of lesion passes with the atherectomy device as well as potential additional treatments were left to the discretion of the operator. An angiographic residual stenosis below 30% reference vessel diameter was assumed to be a successful target lesion intervention.
The interventions were performed by experienced interventionalists. To detect peripheral embolisation following atherectomy, the pre- and post-interventional angiographies of the outflow were compared by two endovascular specialists (A. Rastan, P-C. Flügel).
FOLLOW-UP
According to department standard, a follow-up protocol was advised after the index procedure on an outpatient basis. Follow-up visits including physical examination, estimation of the RBC, ABI measurements and duplex ultrasound were scheduled for 6, 12, and 24 months post procedure.
STATISTICAL ANALYSIS
Continuous data are presented as means±standard deviation; categorical data are given as counts (percentages). Categorical variables were compared with Fisher’s exact test, and continuous data were compared with the Student’s t-test.
Binary logistic regression analysis was performed by means of a stepwise forward variable selection procedure to investigate the predictive value of confounding variables: age, gender, body mass index, smoking status, hypertension, dyslipidaemia, diabetes mellitus, initial lesion grade (stenosis versus occlusion), initial RBC, lesion length, lesion calcification, reference vessel diameter, DCB use, and post-procedural residual stenosis. Outcomes of the regression analysis are given as odds ratio with 95% confidence intervals.
Event-free survival (freedom from cdTLR, and MAE) was evaluated using Kaplan-Meier analysis; the survival curves were compared using the Mantel-Cox log-rank test. Multivariate logistic regression analysis was performed to detect predictors of cdTLR.
All hypothesis testing was two-tailed for comparison of pre- and post-interventional measurements; p<0.05 was considered to indicate significance. Analyses were performed using SPSS software, Version 23.0 (IBM Corp., Armonk, NY, USA).
Results
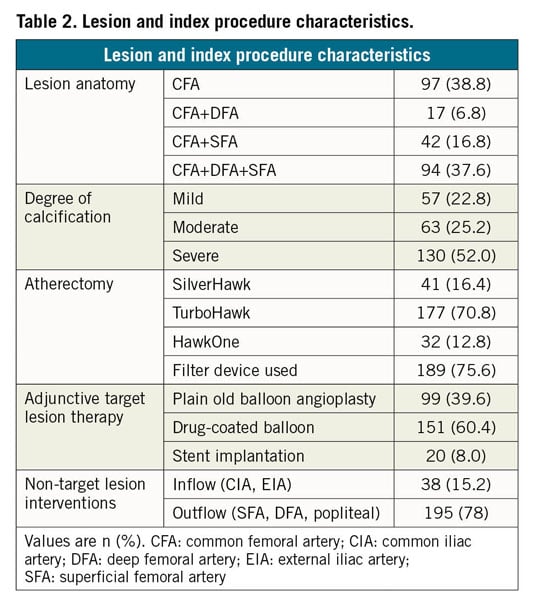
Between March 2009 and June 2017, 2,197 patients with arteriosclerotic lesions of the CFA were treated by an endovascular approach. Of these patients, 250 received DA and were included in this analysis. Baseline characteristics are shown in Table 1. Two hundred and eighteen patients (87.2%) suffered from intermittent claudication (IC; RBC 2 and 3), and 32 patients (12.8%) had critical limb ischaemia (CLI; RBC 4 and 5) (Table 1, Supplementary Figure 1-Supplementary Figure 4). There were 153 CFA-bifurcation lesions (61.2%), and 97 isolated CFA lesions (38.8%). Following suspected intraluminal lesion crossing, eight CFA occlusions (3.2%) were included in this analysis.
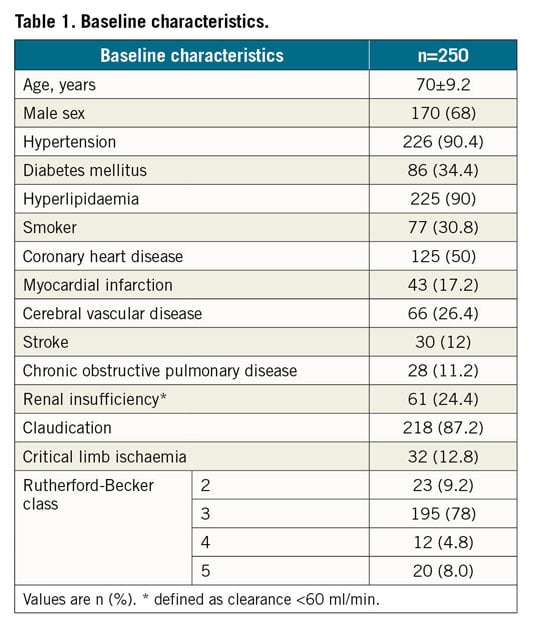
The DA procedure was performed with either the SilverHawk device (in 16.4%; n=41), the TurboHawk device (in 70.8%; n=177) or the HawkOne device (in 12.8%; n=32). In 75.6% (n=189), a distal protection device was used to avoid distal debris embolisation.
Adjunctive angioplasty following DA was performed in all cases, POBA in 39.6% (n=99), and DCB in 60.4% (n=151). Bail-out stenting was performed in 8.0% (n=20), and endoprosthesis placement was necessary in 1.2% (n=3) (Table 2). The types of DCB and stent used are shown in Supplementary Table 3.
ACUTE AND 30-DAY OUTCOMES
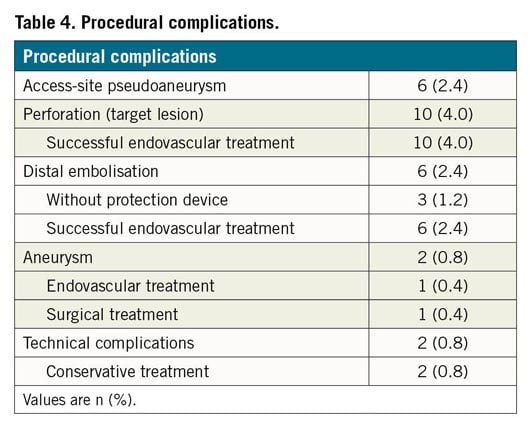
The technical success rate was 92.4% (n=231) (Table 3). Twenty-six procedure-related adverse events (10.4%) were documented. Perforations of the target lesion following atherectomy in 10 (4.0%) patients were treated by prolonged POBA (n=2, 0.8%), nitinol stenting (n=5, 2.0%) or stent graft implantation (n=3, 1.2%) during the index procedure. In six patients (2.4%) an outflow embolisation was documented. Three of these embolisations (1.2%) occurred in procedures without the use of a distal protection device. All embolisation events were treated successfully by catheter aspiration. Six patients (2.4%) with post-interventional access-site pseudoaneurysms underwent ultrasound-guided compression or local thrombin injection.
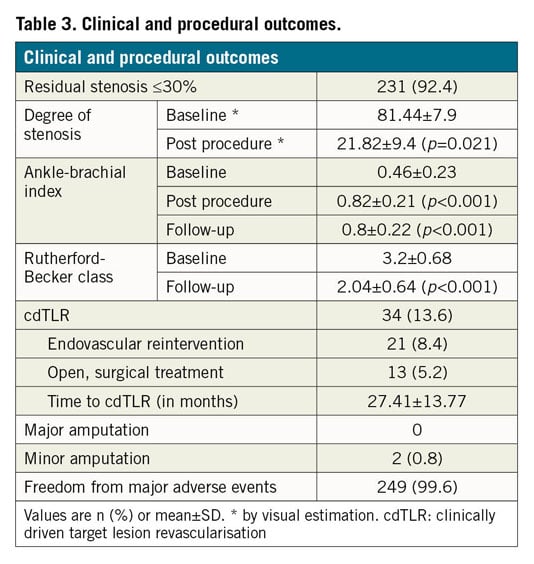
Two patients (0.8%) developed a target lesion aneurysm; one was covered with an endoprosthesis during the index procedure. The second aneurysm became noticeable by ultrasound 51 days post procedure and was treated by open repair. All but one complication could therefore be treated conservatively or endovascularly.
The all-cause 30-day mortality rate was 0.4% (n=1) (Table 4). This one patient died 28 days post procedure of unknown cause.
The mean pre-interventional ABI was 0.46±0.23. This increased significantly to 0.82±0.21 (p<0.001) at discharge (Table 3).
The primary safety endpoint, freedom from MAE at 30 days, was 99.6%.
MIDTERM OUTCOMES
During mean follow-up of 31.03±21.56 months (range 1-88, median follow-up period 25 months), 34 patients (13.6%) had to undergo a cdTLR, resulting in a cdTLR-free survival rate of 86.4% (Figure 1A).
Of note, 8 (42.1%) out of 19 patients with a >30% residual target lesion stenosis had a cdTLR.
During follow-up there was no significant difference concerning TLR-free survival either between patients with CLI and IC (91.7% vs 84.2%, p=0.277) at baseline, or between patients with additional POBA or DCB angioplasty following DA (87.2% vs 83.9% p=0.44), respectively (Figure 1B). In patients with additional stenting of the target lesion (n=20), the cdTLR-free survival rate was 88.9%.
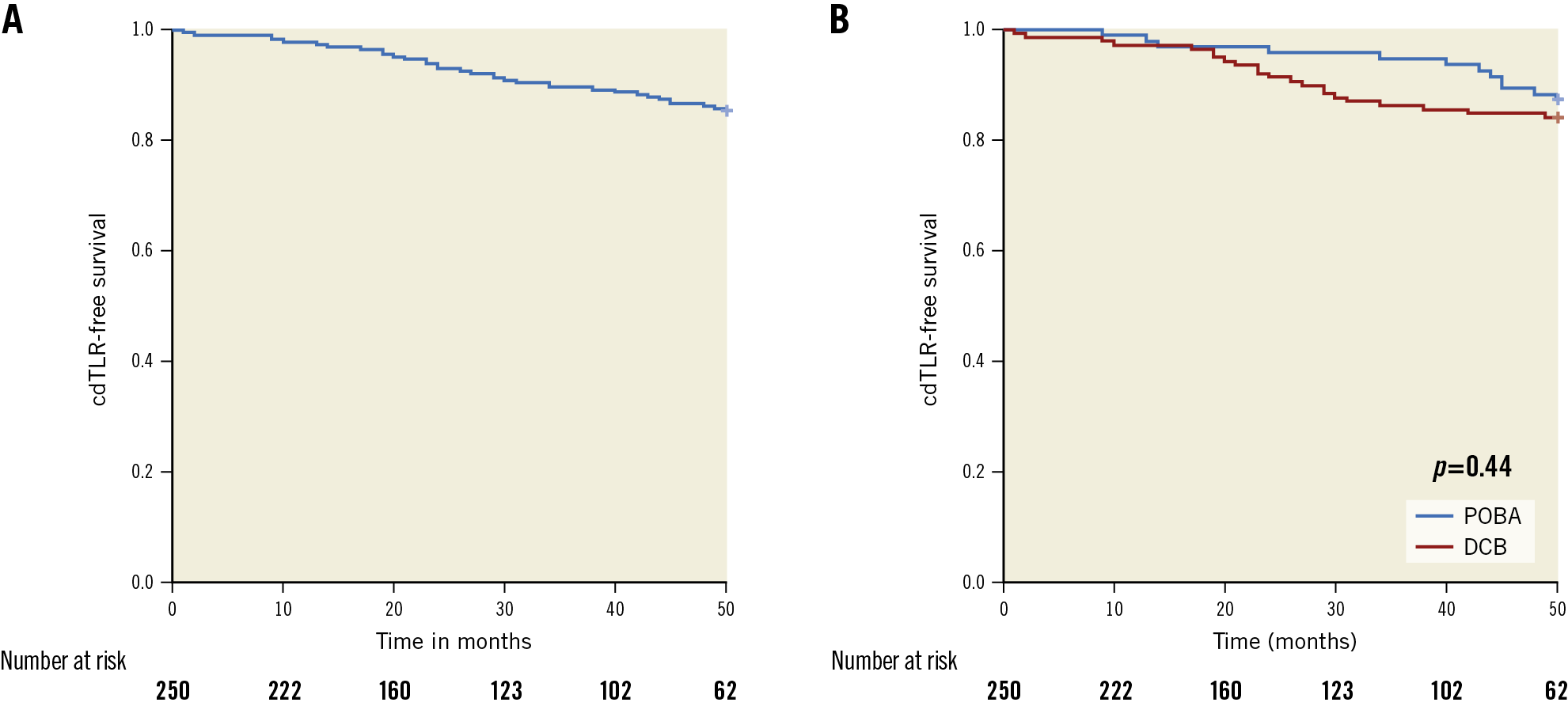
Figure 1. Freedom from cdTLR. A) Kaplan-Meier plot of cdTLR-free survival in the entire cohort. B) Kaplan-Meier analysis of cdTLR-free survival for patients treated with POBA and DCB following directional atherectomy. cdTLR: clinically driven target lesion revascularisation; DCB: drug-coated balloon; POBA: plain old balloon angioplasty
Multivariate logistic regression analysis revealed residual target lesion stenosis >30% (p=0.005), and heavy calcification of the target lesion (p=0.033) as independent predictors for TLR. Of note, for mild, moderate, and severely calcified lesions the cdTLR-free survival was 94%, 87.9% and 80.6% (p=0.02), respectively (Figure 2).
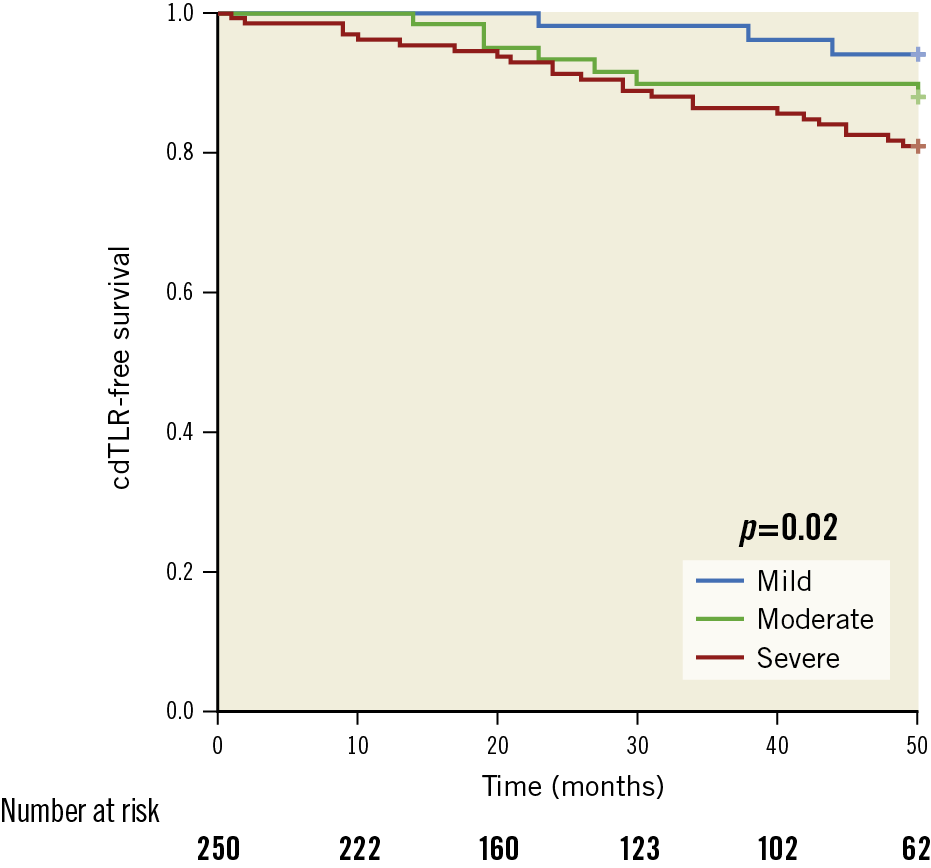
Figure 2. Freedom from cdTLR depending on the degree of calcification. Kaplan-Meier analysis of cdTLR-free survival depending on the degree of calcification. cdTLR: clinically driven target lesion revascularisation
A significant improvement of the mean ABI and mean RBC values from 0.46±0.23 and 3.2±0.68 to 0.8±0.20 and 2.0±0.64 (p<0.001) was observed during mean follow-up. The freedom from MAE rate and limb salvage during follow-up was 71.6%, and 100%, respectively (Figure 3, Table 3).
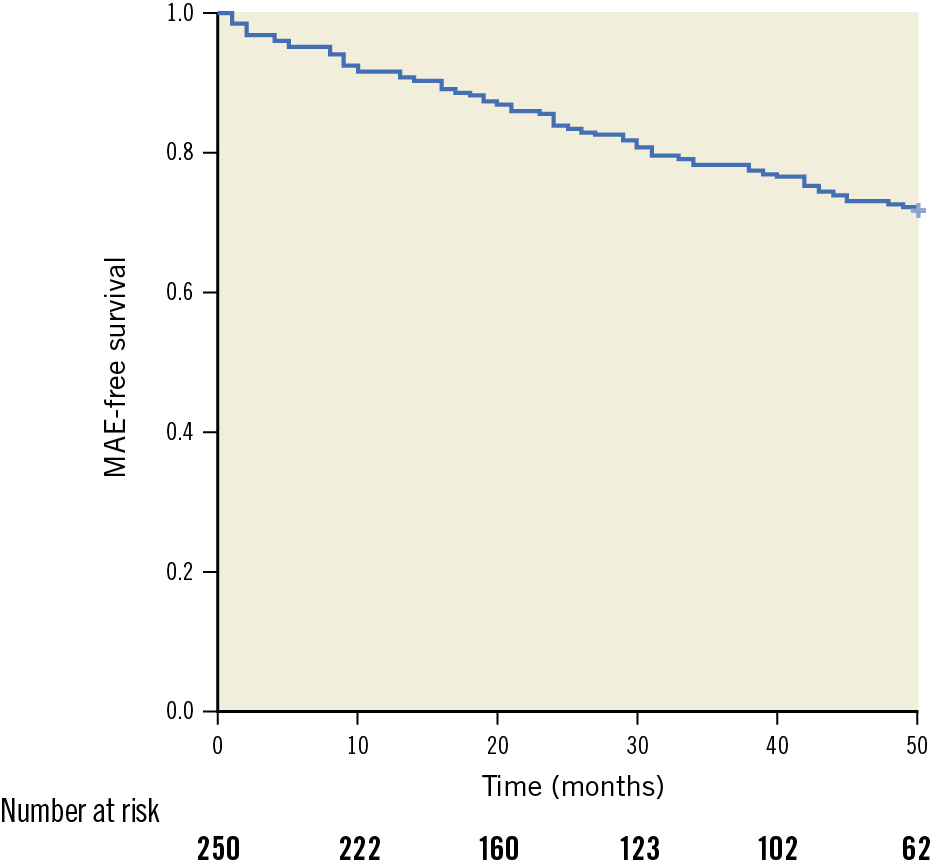
Figure 3. Freedom from MAE. Kaplan-Meier analysis of MAE-free survival. MAE: major adverse events (including death, myocardial infarction, TLR, and major target limb amputation)
Discussion
Atherectomy, and DA in particular, is an established treatment option for atherosclerotic femoropopliteal and infrapopliteal artery lesions12,13,14,15,16,17. However, only a few studies have supported the applicability of DA for the treatment of arteriosclerotic CFA lesions7,18,19. The present analysis represents the largest study evaluating the safety, the technical, and the clinical outcomes of patients with CFA lesions treated with DA.
The primary effectiveness endpoint, freedom from cdTLR, was 86.4% during a mean follow-up of 31±21.6 months. The cdTLR rate (13.6%) is comparable to the results of previous studies which ranged from 14.1% and 23% using POBA with provisional stenting or primary stenting for CFA treatment7,8,19,20. In the TECCO trial, a prospective, randomised, multicentre study comparing primary stent placement and open surgical reconstruction for CFA treatment, comparable TLR rates at two-year follow-up (stent cohort 14.4±5.1%, surgical cohort 15.2±5.0%) were documented11.
In the last decade, the use of DCBs led to impressive results after femoropopliteal interventions. Although there is no class effect, most DCBs showed significantly lower TLR rates at midterm follow-up in comparison to POBA21,22,23. In the present study, predictors of TLR were residual target lesion stenosis ≥30% and severe target lesion calcification. This corresponds to the results of the DEFINITIVE AR study investigating the effect of DA prior to DCB angioplasty in femoropopliteal lesions13. The use of DCBs following DA of the CFA did not reduce the TLR rate in comparison to POBA.
A small prospective, single-centre study including 30 patients showed an impressive one-year TLR rate of only 3.3% for DA plus DCB for CFA treatment18. A possible explanation for the lack of DCB impact on cdTLR in the present study could be the degree of target lesion calcification, which might prevent sufficient drug uptake and may result in subacute vessel recoil. Two studies found the degree of target vessel calcification to be a predictor of reduced effectiveness of DCBs in femoropopliteal artery lesions, displaying an inverse relationship between primary patency, late lumen loss and the grade of calcification24,25,26. Another reason for the lack of superiority of DCBs in this CFA cohort might be the mismatch between vessel size and DCB diameter available, leading to an insufficient vessel apposition. In fact, after evaluation of the angiographies and the procedure reports, a mismatch between a target lesion reference diameter of up to 10 mm and a DCB diameter of a maximum of 7 mm was found in a considerable number of interventions.
The same limitation may be true for the use of vascular lithotripsy, another CFA treatment strategy under clinical evaluation for avoiding stent placement. Lithotripsy has been shown to achieve acute luminal gain comparable to nitinol stent placement in calcified femoropopliteal lesions27. However, lithotripsy balloon diameters are also limited to 7 mm. An international prospective observational registry study is ongoing evaluating the potential benefit of lithotripsy in CFA interventions besides other indications.
Regarding clinical outcomes, a significant improvement in ABI and RBC was achieved in the vast majority of the patients (84.8%). The limb salvage rate was 100%. These findings are roughly equivalent to other trials dealing with endovascular therapy of the CFA and the femoropopliteal arteries8,14,28.
In the present study the procedural complication rate was 10.4%. The target lesion perforation rate was 4.0% (n=10), and comparable to previous femoropopliteal studies (2.3-4.4%)13,14,15. All perforations were treated within the index procedure either by prolonged balloon dilatation or by implantation of bare nitinol stents or covered stents. There was no periprocedural open surgical revision. The overall incidence of target lesion aneurysm formation was low (n=2; 0.8%). Outflow embolisation is a dreaded complication of DA29,30,31. Depending on the use of distal embolic protection devices, the reported rates range from 2.3% to 5.3%12,13,14. In this study, distal embolisation was observed in 2.4% (n=6) of the patients. By performing catheter aspiration, all emboli could be removed during the index procedure. The 30-day freedom from MAE rate was 99.6%.
There is growing evidence that endovascular procedures have the potential to replace open surgery as the gold standard for CFA treatment. The TECCO trial showed comparable technical results during two-year follow-up including freedom from TLR and primary patency. However, the perioperative morbidity rate that caused or prolonged hospitalisation and/or reintervention was significantly higher (26% vs 12.5%, p=0.05) and the time to discharge was significantly longer in the surgical group (6.3±3.0 days vs 3.2±2.9 days, p<0.001)11. Moreover, in a study by Nguyen et al including 1,846 patients with open endarterectomy of the CFA, redo surgery procedures at 30 days (due to, e.g., acute target lesion occlusions, bleeding, infections) were necessary in 10.2% of the patients5. These results were confirmed by reports from other studies, showing wound infections, nerve injuries, haematoma and lymphatic fistulas in up to 13.6% of cases in patients treated with open endarterectomy4,6,32.
The number of patients included in the TECCO trial was too small to draw meaningful conclusions concerning the primary patency rates and TLR presented between the treatment groups (stenting vs open endarterectomy). Although confirmed by smaller studies and subgroup analyses7,8,9,10,11, long-term results of CFA stenting are lacking. Moreover, stenting of an access artery might lead to limitations concerning future endovascular procedures. In the present study, the rate of CFA stenting was low (8%) and the overall rate of freedom from cdTLR was comparable to the results reported for stent placement. Therefore, DA offers a “leave-no-metal-behind” strategy in order to preserve the native artery. The small cohort of patients with CFA stenting in this study (n=20) showed a noticeably low TLR rate of 10% during a mean follow-up period of two years.
Open endarterectomy of CFA lesions is associated with a 30-day mortality rate of 1.5 to 3.4%5,31, whereas the mortality rate in the present study was 0.4%. The ongoing prospective, randomised, multicentre PESTO trial (Percutaneous Intervention Versus Surgery in the Treatment of Common Femoral Artery Lesions) will add evidence to the question whether DA followed by DCB angioplasty has the potential to compete with endarterectomy as the gold standard for CFA treatment33.
Limitations
Even if derived from a prospective database, the study represents a retrospective single-arm analysis without a control group. Moreover, the assumable mismatch of the target lesion reference diameter and the diameter of the DCBs used following DA potentially has an impact on the performance of the DCB cohort.
Conclusions
In experienced hands, DA of atherosclerotic CFA lesions provides promising results with a low cdTLR rate at midterm follow-up. DA complication rates are acceptable. Severely calcified lesions and a residual stenosis >30% are predictors of cdTLR. Randomised prospective studies are required to clarify the potential role of this endovascular procedure in CFA treatment compared to open surgical reconstruction.
|
Impact on daily practice DA of atherosclerotic CFA lesions provides promising results. Even if further investigations are necessary, DA should be considered as an alternative therapy option for the treatment of arteriosclerotic CFA lesions. |
Conflict of interest statement
E. Noory has received honoraria from Boston Scientific, Abbott, and Medtronic. T. Zeller has received honoraria from Abbott Vascular, Veryan, Biotronik, Boston Scientific, Cook Medical, Gore & Associates, Medtronic, Philips-Spectranetics, and Shockwave, has consulted for Boston Scientific, Gore & Associates, Medtronic, Veryan, Intact Vascular, Shockwave, Bayer, and Vesper Medical, has received research clinical trial, or drug study funds to his institution from 480 biomedical, Bard Peripheral Vascular, Veryan, Biotronik, Cook Medical, Gore & Associates, Medtronic, Philips, Terumo, TriReme, Shockwave, Med Alliance, Intact Vascular, and B. Braun, and has common stock with QT Medical. A. Rastan has received honoraria from Abbott, Terumo, and Medtronic. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.