Abstract
Aims: To assess when and how the microcatheter-facilitated reverse wire technique should be applied to cross the guidewire into side branches in coronary bifurcations.
Methods and results: Three interventional cardiologists with different levels of experience performed in vitro bench testing using an originally developed coronary bifurcation simulator which had six coronary bifurcations. The bifurcation angles were 90, 105, 120, 135, 150 and 165 degrees (°). Experiment 1 was conducted to assess in what coronary bifurcation the reverse wire technique is required. Antegrade guidewire advancement was conducted with two different guidewires: the spring coil guidewire SION blue and the polymer-jacket hydrophilic guidewire Fielder FC. Experiment 2 was conducted to determine what the optimal guidewire selection and the optimal guidewire shape for the reverse wire technique would be. Assessment of the guidewire crossability into the highly angulated side branch was performed, and then the balloon crossability was assessed. A total of four guidewire types were compared in experiment 2. In experiment 1, guidewire crossing was impossible by conventional antegrade wiring when the bifurcation angle became 150° or more. In experiment 2, guidewire crossing of more than 150° of bifurcation angle was achievable independent of the guidewire types and shape. Balloon deliverability was best when using a polymer-jacket hydrophilic guidewire with a round shape 3 cm from the guidewire tip.
Conclusions: Although the guidewire crossing into the side branch was impossible by conventional antegrade methods when the bifurcation angle became 150° or more, the guidewire crossing into such a highly angulated side branch was easily possible using the reverse wire technique. The optimal guidewire selection for the reverse wire technique is the polymer-jacket hydrophilic guidewire with a round shape 3 cm from the guidewire tip.
Introduction
Coronary bifurcation lesions are not rare and still remain one of the considerable challenges of treatment with percutaneous coronary intervention (PCI)1,2. At present, the provisional technique of implanting one stent on the main branch is the default approach in most bifurcation lesions2,3. In this provisional approach, advancement of a guidewire to the side branch is also always recommended for several reasons: it enables predilatation if required and, if the side branch is occluded or dissected, it can be used as a marker of the true lumen4. The complex pattern of bifurcation anatomies and atherosclerotic distribution sometimes makes side branch wiring extremely difficult. Several methods have been proposed to solve the problems including main vessel predilatation and debulking, the Venture® wire control catheter (St. Jude Medical, St. Paul, MN, USA), and the reverse wire technique4,5. The reverse wire technique was first described in 2008 by Kawasaki and colleagues5, and is currently performed with some modifications6. The main differences from the original technique include the facilitation of a microcatheter and the different bending point. Briefly, the reverse guidewire technique requires making a reverse bend in a coronary guidewire about 3 cm from its distal tip. After advancing the guidewire using a Crusade dual port microcatheter (Kaneka, Osaka, Japan) in the distal main vessel, the Crusade microcatheter is pulled back proximally. The guidewire is then manually steered back into the side branch with some rotation. We propose that the microcatheter-facilitated reverse wire technique would be a more appropriate name for the current reverse wire technique. Recently, we have experienced a case of difficult side branch access in which the microcatheter-facilitated reverse wire technique was successfully conducted (Figure 1). The case raised questions as to the proper application of the microcatheter-facilitated reverse wire technique. Several issues are still unclear about the technique. The present study aimed to investigate the following two issues: 1) in what coronary bifurcation is the microcatheter-facilitated reverse wire technique required, and 2) what is the optimal guidewire selection and shape for the technique.
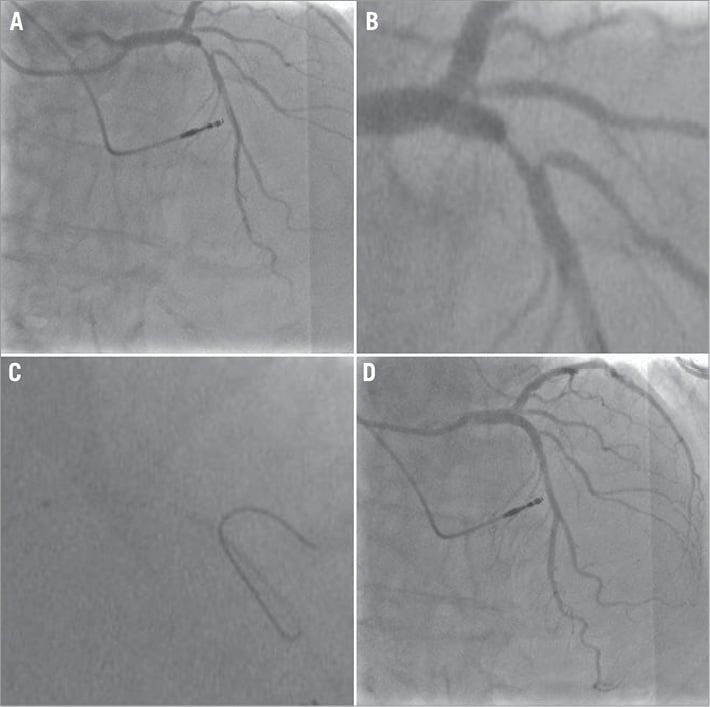
Figure 1. A case of coronary bifurcation lesion with difficult side branch access in a 62-year-old woman. A) Coronary angiography revealed a bifurcation lesion in the middle portion of the left anterior descending artery. B) Magnification of the angiographic image. A complex plaque formation just proximal to the lesion changed the bifurcation angle to wide. Antegrade wiring into the side branch failed repeatedly. C) Magnification of the fluoroscopic image during the reverse wire technique. The reverse wire technique utilising a spring coil guidewire (SION blue; Asahi Intecc, Aichi, Japan) and a dual port microcatheter (Crusade; Kaneka, Osaka, Japan) was successfully conducted. The reverse bend was made 3 cm from its distal tip with a sharp curve. After crossing the guidewire into the side branch, the side branch was dilated with a 2 mm balloon. Then a 3.0 mm drug-eluting stent (XIENCE V; Abbott Vascular, Santa Clara, CA, USA) was deployed in the main branch. D) Final angiography showing satisfactory blood flow in the main and side branch vessels.
Methods
STUDY DESIGN
In vitro bench testing was conducted using an originally developed coronary bifurcation simulator made of polycarbonate and polyoxymethylene (Figure 2). There are six coronary bifurcation lesions in a simulator; bifurcation angles were 90, 105, 120, 135, 150 and 165 degrees. We prepared four simulators; each simulator had a different vessel size. The size of the main branch and side branch in each simulator was 4.0 mm and 3.5 mm, 3.5 and 3.0 mm, 3.0 and 2.5 mm, 2.5 and 2.0 mm, respectively. The simulator was put in a tray filled with 33% glycerol. The viscosity of glycerol is similar to that of blood. All procedures were conducted using a 6 Fr JR 4.0 guide catheter (Brite Tip®; Cordis, Miami, FL, USA) under fluoroscopic guidance (OEC 9800 Plus; General Electric, Fairfield, CT, USA).
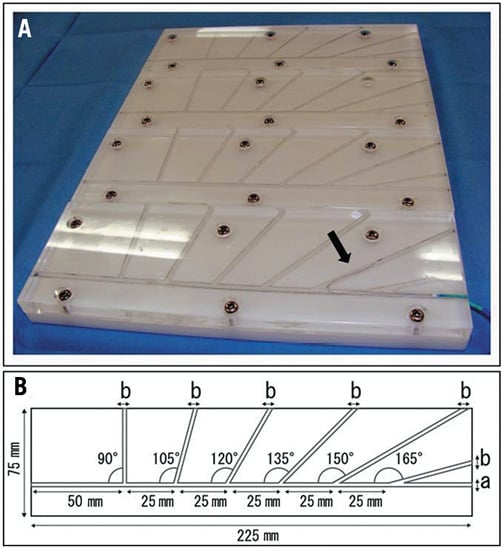
Figure 2. A) Originally developed coronary bifurcation simulators. Six coronary bifurcation lesions exist in each simulator; bifurcation angles are 90, 105, 120, 135, 150 and 165 degrees. The size of the main branch and side branch in each simulator is 4.0 and 3.5 mm, 3.5 and 3.0 mm, 3.0 and 2.5 mm, 2.5 and 2.0 mm, respectively. A guidewire making a reverse bend is inserted into the side branch with a bifurcation angle of 150° in the lowest simulator (arrow). B) Drawing of the bifurcation simulator. “a” indicates the size of the main branch and “b” indicates the size of the side branch.
The procedures were performed with the bifurcation simulator by three independent operators. Operator A has 12 years’ experience in interventional cardiology, operator B has nine years’ experience, and operator C has one year. The success rate and the time required to cross a guidewire into the angulated side branch, and the deliverability of a device through the guidewire, were measured as the primary endpoints. The procedure time was defined as the elapsed time from the insertion of the guidewire or balloon catheter into the bifurcation simulator to cross into the side branch. Any procedures requiring more than three minutes were abandoned and the procedure time was recorded as 180 seconds in these abandoned procedures. A total of two experiments were conducted to assess the aforementioned two study issues. All experiments were performed twice using the same protocol to assess the reproducibility of the study.
EXPERIMENT 1
Experiment 1 was conducted to determine in what coronary bifurcation the microcatheter-facilitated reverse wire technique is required. In the experiment, a guidewire crossing into the angulated side branch using a conventional method was performed. Two types of 0.014 inch guidewires were used: one was a spring coil guidewire (SION blue; Asahi Intecc, Aichi, Japan), and the other was a polymer-jacket hydrophilic guidewire (Fielder FC; Asahi Intecc). Each guidewire was examined in each attempt. Guidewire shape was dependent on the operators. An Excelsior® microcatheter (Boston Scientific, Natick, MA, USA) was used for crossing the guidewire when required. The success rate and the time required to cross the guidewire into each angulated side branch were measured.
EXPERIMENT 2
Experiment 2 was conducted to determine what were the optimal guidewire selection and the optimal guidewire shape for the microcatheter-facilitated reverse wire technique. Experiment 2 was divided into two parts: first, assessment of the guidewire crossability into the highly angulated side branch using the microcatheter-facilitated reverse wire technique was performed, and then an assessment of the balloon crossability was performed. In both parts, two different guidewire shapes for two different guidewires were examined. One type of guidewire shape was to make a sharp curve as the reverse bend 3 cm from the guidewire tip. The second was to make a round curve as the reverse bend instead. The two guidewire types applied in experiment 2 were the same as in experiment 1. A total of four different groups were compared in experiment 2 (Figure 3): SION blue with a sharp curve (SBSC), SION blue with a round curve (SBRC), Fielder FC with a sharp curve (FFSC) and Fielder FC with a round curve (FFRC). The Crusade dual port microcatheter was employed when using the microcatheter-facilitated reverse wire technique. The Crusade microcatheter has a short monorail rapid exchange port which exits at the distal tip of the catheter, and an over-the-wire port which exits proximally at the side of the catheter (Figure 3E). The guidewire with a reverse bend was inserted in the over-the-wire port. The device deliverability test was conducted using a small semi-compliant coronary balloon catheter (Ikazuchi Revolution; Kaneka, Osaka, Japan). The balloon diameter was 1.2 mm and the balloon length was 6 mm. The success rate and the time required to cross the guidewire or the balloon catheter into each angulated side branch were measured.
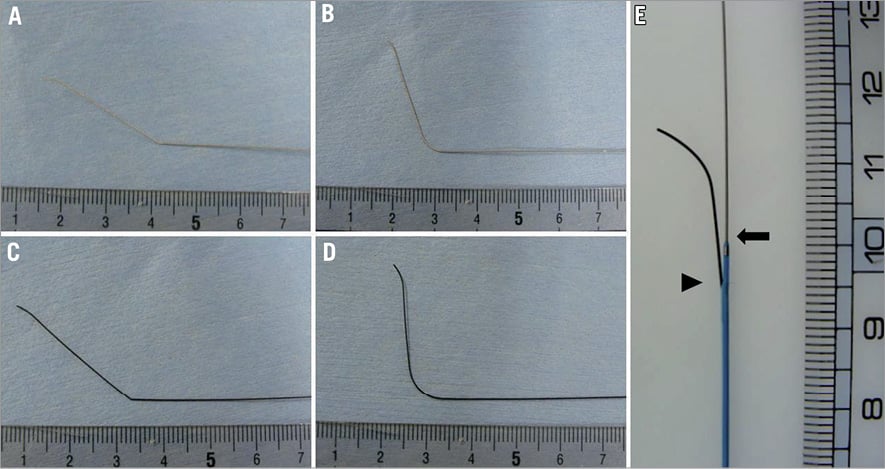
Figure 3. The four types of guidewire and the Crusade dual port microcatheter used in the study. A) SION blue with a sharp curve at a point 3 cm from the guidewire tip. B) SION blue with a round curve. C) Fielder FC with a sharp curve. D) Fielder FC with a round curve. E) The Crusade dual port microcatheter. The catheter has a short monorail rapid exchange port which exits at the distal tip of the catheter (arrow), and an over-the-wire port which exits proximally at the side of the catheter (arrow head).
Statistical analysis
All numeric values are expressed as mean±standard deviation. The success rate in each group was compared by a chi-square test followed by a Ryan’s multiple comparison test for proportions. The parametric data were compared using one-way analysis of variance (ANOVA) followed by a Tukey-Kramer multiple comparison test. All data were handled using JMP version 9.0 (SAS Institute, Cary, NC, USA). A value of p<0.05 was considered to be statistically significant in all analyses.
Results
EXPERIMENT 1
The Excelsior microcatheter was employed in all cases. The guidewire tip shapes depended on the operators, but the shapes were almost identical. A wide smooth bend or a double bend was applied in most cases. The success rate of guidewire crossing into the angulated side branch decreased as the bifurcation angle became higher. The success rate was 100% at 90° and 105°, 97.9% at 120°, 56.3% at 135°, and 0% at both 150° and 160° (Figure 4A, p<0.0001, chi-square test). The success rate at 150° and 160° was significantly lower compared to the other bifurcation angles (Figure 4A, p<0.0001, chi-square test and Ryan’s multiple range test). The procedure time also became longer as the bifurcation angle became higher: 5±2 seconds at 90°, 6±4 seconds at 105°, 17±40 seconds at 120°, 103±73 seconds at 135°, and 180±0 seconds at 150° and 165° (p<0.0001, ANOVA). The procedure times at 150° and 165° were significantly higher when compared to the other bifurcation angles (Figure 4B, p<0.0001, ANOVA followed by a Tukey-Kramer multiple comparison test). The results showed no difference between the two types of guidewire: the overall success rate and procedure time were 57.6% and 85±84 seconds when using the spring coil wire and 60.4% and 79±83 seconds when using the polymer-jacket hydrophilic guidewire (p=not significant, chi-square test and ANOVA). Most importantly, the guidewires crossing into the side branch with 150° or more all resulted in failure independent of the guidewire selection. The results indicated that the guidewire crossing into the side branch was impossible by conventional antegrade wiring when the bifurcation angle became 150° or more.
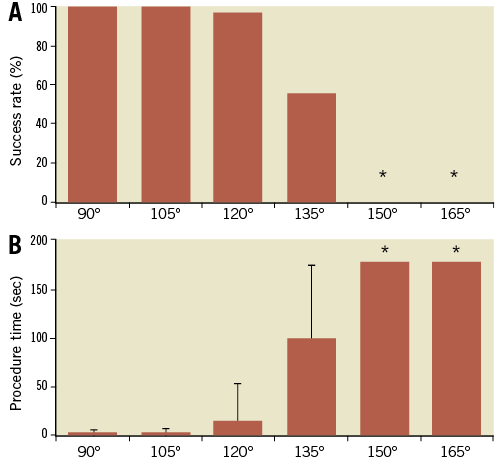
Figure 4. Results of the guidewire crossing into the angulated side branch using a conventional method. A) The success rate of the guidewire crossing into the side branch in each bifurcation. The success rates were 100% in 90° and 105°, 97.9% in 120°, 56.3% in 135° and 0% in 150° and 160°. *The success rate in 150° and 160° is significantly lower compared to the other bifurcation angles (p<0.0001, chi-square test and Ryan’s multiple range test). B) The procedure time for the guidewire crossing into the angulated side branch using a conventional method. The procedure times were 5±2 seconds in 90°, 6±4 seconds in 105°, 17±40 seconds in 120°, 103±73 seconds in 135° and 180±0 seconds in 150° and 165°. *The procedure times in 150° and 165° were significantly higher compared to the other bifurcation angles (p<0.0001, ANOVA followed by a Tukey-Kramer multiple comparison test).
EXPERIMENT 2
Reviewing the results of experiment 1, the guidewire crossing into the side branch of the bifurcation angle of 150° and 165° was performed using the microcatheter-facilitated reverse wire technique. The four previously mentioned guidewire types were employed in experiment 2: SBSC, SBRC, FFSC, and FFRC. The success rate was 100% in both angles (Figure 5A). The procedure time was 13±26 seconds at 150°, and 19±20 seconds at 165° (Figure 5B). There were no significant differences between the four guidewire groups in terms of the success rate and procedure times (Figure 5C and Figure 5D, p=0.08 in ANOVA). The results indicated that the guidewire crossing into the extremely angulated side branch using the microcatheter-facilitated reverse wire technique was achievable independent of the guidewire types and shape.
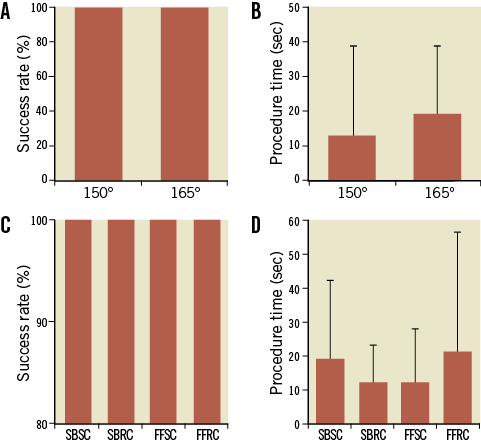
Figure 5. Results of the guidewire crossing into the angulated side branch using the reverse wire technique. A) The success rate was 100% in both angles (p=n.s.). B) The procedure time was 13±26 seconds in 150°, and 19±20 seconds in 165° (p=n.s.). C) The success rate was 100% in all guidewire groups (p=n.s.). D) The procedure time was 19±23 seconds in SBSC, 12±11 seconds in SBRC, 12±16 seconds in FFSC, and 21±35 seconds in FFRC (p=n.s.).
After insertion of the guidewire in the side branch, the balloon deliverability was compared in the four guidewire types. The success rate of the balloon delivery was 25.0% with SBSC, 22.9% with SBRC, 75.0% with FFSC, and 100% with FFRC (Figure 6A, p<0.0001 in chi-square test). The balloon became stuck at the bending point and caused prolapse of the guidewire in the failed case. The success rate of FFRC was significantly higher compared to the other groups (p<0.0001, chi-square test and Ryan’s multiple comparison test). The procedure time required for the balloon delivery was 143±66 seconds in SBSC, 149±62 seconds in SBRC, 70±67 seconds in FFSC, and 20±16 seconds in FFRC (p<0.0001, ANOVA), Figure 6B. When using FFRC, the procedure time was significantly shorter compared to the other guidewire groups (p<0.0001, Tukey-Kramer multiple comparison test). The results indicated that the device deliverability was best when using the FFRC (polymer-jacket hydrophilic guidewire with a round curve 3 cm from the guidewire tip).
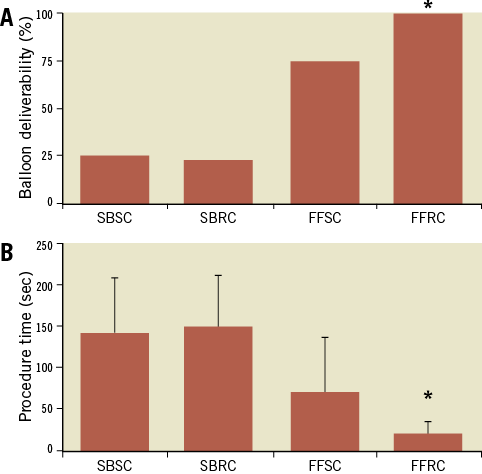
Figure 6. Results of the balloon deliverability in the 4 guidewire types. A) The success rate of the balloon delivery was 25.0% with SBSC, 22.9% with SBRC, 75.0% with FFSC, and 100% with FFRC. *The success rate of FFRC was significantly higher compared to the other groups (p<0.0001, chi-square test and Ryan’s multiple comparison test). B) The procedure time required for the balloon delivery was 143±66 seconds in SBSC, 149±62 seconds in SBRC, 70±67 seconds in FFSC, and 20±16 seconds in FFRC. *When using FFRC, the procedure time was significantly shorter compared to the other guidewire groups (p<0.0001, ANOVA followed by Tukey-Kramer multiple comparison test).
Discussion
The aim of the present study was to investigate when and how the microcatheter-facilitated reverse wire technique should be applied. The main findings of the present study were as follows. 1) The guidewire crossing into the side branch was impossible by conventional antegrade wiring when the bifurcation angle became 150° or more. However, using the microcatheter-facilitated reverse wire technique, the guidewire crossing into such a highly angulated side branch was easily possible, independent of the guidewire selection and shape. 2) After crossing the guidewire with the microcatheter-facilitated reverse wire technique, the device deliverability was best when using a polymer-jacket hydrophilic guidewire with a round curve 3 cm from the guidewire tip. This was considered the optimal guidewire selection and shape for the microcatheter-facilitated reverse wire technique.
Coronary bifurcation lesions are not rare, being present in as many as 15 to 20% of lesions undergoing PCI1,2. The high frequency of coronary bifurcation lesions is explained by the tendency for atherosclerosis to develop at bifurcation points due to turbulence and high shear stress7. Despite the high frequency rate, PCI for bifurcation lesions is still considered challenging and is associated with lower procedural success and higher adverse event rates than observed in non-bifurcation lesions1,2. Although several techniques and strategies have been proposed for the treatment of coronary bifurcation lesions, advancement of a guidewire to the side branch is mandatory4. The complex patterns of bifurcation anatomies and plaque distribution occasionally make the side branch wiring extremely difficult4,5. Several methods have been proposed to solve the difficult side branch access. Antegrade wiring with a change of guidewire to a stiffer or hydrophilic polymer-coated wire, making a single wide bend or double bend shape, and application of the microcatheter or multifunction catheter, are usually the first performed, and result in success in most cases. When these antegrade methods do not work, the pullback wire technique or the reverse wire technique should be considered4,5. Another option to solve difficult side branch access is the use of a Venture wire control catheter, which enables the guidewire to be directed towards the side branch after deflection of the catheter tip8,9. When all the other techniques have failed, a main branch balloon predilatation or debulking can be considered for guidewire advancement to the side branch. However, these strategies carry the risk of causing plaque shift, finally resulting in side branch occlusion4,10.
The reverse wire technique was first published in 2008 by Kawasaki and colleagues5, and is currently performed with several modifications6. The main differences include the use of a Crusade dual port microcatheter and the making of the reverse bend. In the original paper the reverse bend was recommended to be made at a point 5 cm from the guidewire tip. After the report of guidewire disjunction, the reverse bend is currently recommended to be made at a point 3 cm from the guidewire tip6. The present study revealed that a polymer-jacket hydrophilic guidewire with a round shape 3 cm from the guidewire tip is the optimal guidewire selection and shape for the microcatheter-facilitated reverse wire technique. A possible explanation why the polymer-jacket hydrophilic guidewire is more suitable for the microcatheter-facilitated reverse wire technique is that the surface hydrophilic coating facilitates device deliverability. Figure 7 shows electron micrographs of the guidewire used in the study, in which the smooth surfaces of the hydrophilic coated guidewires were observed. We consider that the present study results provide additional information towards the correct application of the microcatheter-facilitated reverse wire technique. The technique is not required in most bifurcation lesions, but should be considered as a last resort to cross the guidewire into a highly angulated side branch. Figure 8 depicts the schematic procedure of the microcatheter-facilitated reverse wire technique that we propose.
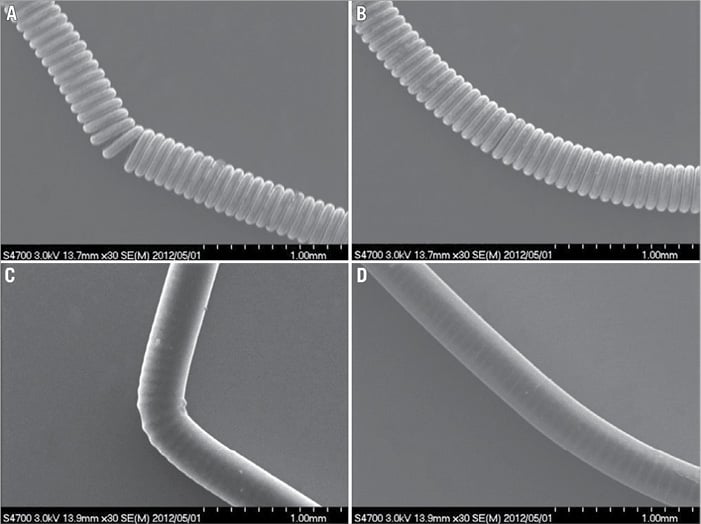
Figure 7. Electron micrographs of the 4 types of guidewire used in the study. A) SION blue with a sharp curve at a point 3 cm from the guidewire tip. B) SION blue with a round curve. C) Fielder FC with a sharp curve. D) Fielder FC with a round curve.
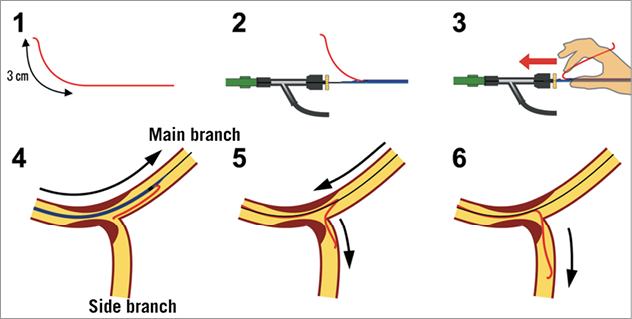
Figure 8. Diagrammatic representation of the various steps of the reverse wire technique. 1) Making a reverse bend at a point 3 cm from the guidewire tip. The guidewire should be a polymer-jacket hydrophilic guidewire. The reverse bend should be a smooth round curve. 2) The guidewire is inserted into the second port of the Crusade dual port microcatheter. 3) The reverse wire system is advanced into the Y connector by softly folding the guidewire. 4) The reverse wire system is advanced beyond the bifurcation lesion through the guidewire placed in the main branch. 5) After pulling back the Crusade catheter proximal to the bifurcation lesion, the guidewire is carefully pulled back and steered into the side branch. Some rotations may be required for advancing the tip of the guidewire to the side branch. 6) The guidewire is advanced into the angulated side branch by slowly pulling back the guidewire.
Limitations
There are several limitations to the present study. Most importantly, the study was conducted in an artificially made bifurcation simulator. The potential complications of the technique cannot be assessed in the simulator. The simulator also lacks diversity of human cardiovascular disease. There seems to be a large difference between the experimental model and human coronary bifurcation lesions. The model is not representative of the dynamic eccentric plaque that is usually opposite to the carina, which is an important factor of the bifurcation lesion11. The model also lacks other factors such as calcification, vessel tortuosity and severity of narrowing. Reproducing all these factors in a bench top simulator is difficult and might obscure the study purpose. The present study focused on the bifurcation angle. We consider that the bifurcation model used in the present study extracted the essence of a human bifurcation lesion required to assess when and how the reverse wire technique should be applied, the primary purpose of the present study.
Secondly, the endpoints are the success rate and procedure time, both dependent on the physician’s abilities. We calculated the inter- and intra-operator correlation coefficient of the procedure time to assess the reproducibility of the study. The inter-operator correlation coefficients of each pair were 0.90 (operator A vs. B), 0.86 (operator B vs. C) and 0.91 (operator A vs. C). The mean intra-operator correlation coefficient was 0.84. The inter- and intra-operator correlation coefficients were larger than 0.8, which indicates that the reproducibility of the study was good.
Finally, one may consider that the procedural time limit of 180 seconds is too short in clinical practice. The present study employed an artificially made coronary bifurcation model which simulates a human coronary bifurcation, mainly focusing on the bifurcation angle. The bifurcation model is morphologically simple compared to real human coronary bifurcation. Thus, judgements can be made earlier than in human coronary bifurcation due to the simplicity of the model.
Conclusions
In conclusion, the guidewire crossing into the side branch was impossible by conventional antegrade methods when the bifurcation angle became 150° or more. However, the guidewire crossing into such highly angulated side branches was easily possible using the microcatheter-facilitated reverse wire technique. The optimal guidewire selection and shape for the microcatheter-facilitated reverse wire technique is the polymer-jacket hydrophilic guidewire with a round shape 3 cm from the guidewire tip.
Acknowledgements
The Crusade dual port catheter and the bifurcation simulator were supplied by Kaneka. The guidewires used in the study were supplied by Asahi Intecc. Thanks to Ms. Rika Sugiura for her secretarial support.
Conflict of interest statement
The authors have no conflicts of interest to declare.

