Abstract
Aims: Magnetic guidewire assisted percutaneous coronary interventions (MPCI) could have certain advantages in coronary bifurcation lesions. We aimed to report the angiographic characteristics of the bifurcation lesions, as well as the procedural and clinical outcomes of the MPCI patients.
Methods and results: The lesion characteristics and the treatment effect were assessed by performing diagnostic and quantitative coronary angiography with dedicated bifurcation software. A total of 76 patients (age 65 years, 78% male) were assigned to undergo MPCI, in which two-thirds of the lesions were located in LAD/D1. Fifty-seven out of 78 lesions (73%) had a diseased side branch and complex stenting techniques were used in the majority of the lesions (64%). All 59/78 (76%) fenestration attempts were successfully performed and only 13 dedicated bifurcation stents were implanted. The average acute gain in minimal luminal diameter was 1.08±0.81mm, 0.80±0.70 mm and 0.59±0.56 mm for the proximal, distal and side branch, respectively. The procedural success was 69% with a procedure time of 107±43 minutes, fluoroscopy time of 34±24 minutes and contrast use of 338±136 ml. At a mean of 1.8-years follow-up, 15 patients (20%) had a cardiac event.
Conclusions: MPCI is associated with good angiographic, fenestration and procedural success rates in the treatment of coronary bifurcation lesions.
Abbreviations
CI: confidence interval
HR: hazard ratio
MACE: major adverse cardiac events
MI: myocardial infarction
MNS: magnetic navigation system
MPCI: magnetic percutaneous coronary intervention
QCA: quantitative coronary angiography
TVR: target vessel revascularisation
Introduction
Nearly 20% of all percutaneous coronary interventions (PCI) performed worldwide are because of coronary artery bifurcation lesions1. Throughout the years, several single stenting and double stenting strategies have been explored to overcome the worse procedural and clinical success rates of the treatment of bifurcation lesions compared to non-bifurcation lesions2,3. Although some bifurcation treatment strategies such as the “crush” technique were developed to ensure scaffolding of the side branch ostium, it proved in certain cases to be technically demanding to enter the side branch for the desired kissing balloon dilatation post-stent implantation4,5. The complexity of these techniques could result in a longer fluoroscopy time and more contrast use, eventually to the detriment of both the patient and the operator. Additionally, some coronary bifurcation lesions are difficult to reach due to the associated angulations. Because of these shortcomings, there has been a lot of interest in developing dedicated bifurcation stents and implementing novel systems in daily PCI-practice6-9.
Magnetic navigation system assisted percutaneous coronary intervention (MPCI) appeared to be not only safe and applicable in chronic total occlusions and tortuous vessels, but also significantly reduced procedural time, contrast use and fluoroscopy time in distal and/or complex coronary lesions compared to conventional PCI10-12. Even in the treatment of a coronary bifurcation lesion that could not be completed conventionally, MPCI showed to be successful13.
To date there are no studies reporting the treatment of coronary bifurcations lesions with MPCI. The aim of the present study was to describe the angiographic characteristics of the coronary bifurcation lesions, as well as to assess the acute procedural and clinical outcomes of MPCI in the treatment of coronary bifurcation lesions.
Methods
Patient population
From August 2005 until April 2009, a total of 76 patients with coronary bifurcation lesions were treated in our centre due to stable angina, unstable angina or acute myocardial infarction with the magnetic navigation system (MNS)14. Haemodynamic instability or any contraindication for the MNS, such as having a pacemaker, resulted in a non-magnetic approach. Each patient was pre-treated with aspirin and ≥300 mg clopidogrel and all procedures were performed according to standard clinical guidelines by MNS trained interventional cardiologists, who had unrestricted access to both magnetic tipped and conventional guidewires. The utilised stenting technique was dependent on the strategy of the operating interventional cardiologist.
Between March 2007 and October 2007 patients were treated exclusively with everolimus-eluting stents in the context of the Xience-Stent Evaluated At Rotterdam Cardiology Hospital (X-SEARCH) registry. Outside this timeframe, the implantation of the type of stent, drug-eluting or non drug-eluting stent and dedicated or non-dedicated bifurcation stent, was the choice of the operator.
The post-PCI antiplatelet regimen consisted of at least ≥80 mg aspirin lifelong and ≥75 mg clopidogrel for one month if bare metal stents were used and ≥6 months if drug-eluting stents were used. During this time period, the policy changed into the usage of clopidogrel for at least 12 months if drug-eluting stents were used.
The procedural flow sheets were used to collect angiographic and procedural data including the used materials, contrast media (ml) and procedure time (min).
Definitions
Clinical data were collected with the use of our electronic database. All patients using antidiabetic medication were categorised as having diabetes. A blood pressure of ≥140/90 mHg or the usage of antihypertensive medication was defined as hypertension, regardless of the prevalence of diabetes. Hypercholesterolaemia was defined as the usage of lipid lowering drugs or a fasting total cholesterol ≥6.2 cmmol/l.
Angiographic success was defined as a residual stenosis <30% in the main branch and side branch in the presence of Thrombolysis in Myocardial Infarction (TIMI) 3 flow grade. Procedural success was defined as angiographic success without the occurrence of events (death, acute stent thrombosis, myocardial infarction (MI), target-vessel revascularisation [TVR] and stroke) within two days post-intervention. Procedural time (min) was measured by calculating the elapsed time between the femoral sheath was inserted and the patient left the operating room. The contrast media (ml) used during the whole procedure was measured. The fluoroscopy time (min) during the whole MPCI-procedure was automatically recorded by the digital angiography system (AXIOM Artis dCF; Siemens, Forchheim, Germany).
Major adverse cardiac event (MACE) was defined as a composite of death, MI or TVR during follow-up. MI was diagnosed by recurrent symptoms, the development of ST-segment elevation or left bundle branch block on electrocardiography with a CK-MB rise of ≥3 times the upper limit of normal and/or troponin levels of ≥3 times the upper limit of normal in the laboratory values. TVR was defined as a repeat PCI procedure in the same index vessel.
Magnetic navigation system and guidewires
The MNS (Niobe® II MNS; Stereotaxis, St Louis, MO, USA) is a fully independent operating system that cooperates with the C-arm single-planar digital angiography system (AXIOM Artis dFC; Siemens, Forchheim, Germany). By using two computer-controlled neodymium-iron-boron magnets located on either side of the fluoroscopy table, a 15-20 cm spherical magnetic field of 0.08 Tesla is created within the patient. The generated magnetic vector can either be controlled by selecting a certain direction on the touch screen of the Navigant™ Work Station (NWS; Stereotaxis, Inc., St. Louis, MO, USA), which in turn redirects the external magnets in all possible positions (rotation, translation, tilt), or by constantly calculating the course of the coronary artery in three real space coordinates using dedicated software and accordingly adjusting the tip (CardiOp-B; Paieon Medical Inc., Rosh Ha’ayin, Israel).
The following magnetic tipped guidewires, which were available in variable sizes and stiffness, were used in the coronary interventions: (1) Titan™ (Stereotaxis, St. Louis, MO, USA) and (2) Cronus™ (Stereotaxis, St Louis, MO, USA). Damaged guidewires could be exchanged for a similar or a different magnetic tipped wire. The selection of the magnetic tipped guidewires depended fully on the availability at that specific time point. The Titan™ guidewires were introduced later than the Cronus™ guidewires and were specifically designed to be more flexible and steerable in vessels with complex anatomy15. If both types were available then the choice depended on the judgement of the interventional cardiologist.
Coronary bifurcations
The lesion was classified as a bifurcation lesion if it the main parent vessel (≥2.5 mm) had a significant diameter stenosis of >50%, with or without involvement of the origin of the side branch (≥2 mm) by visual estimate. The coronary bifurcation lesions included lesions in the left anterior descending coronary artery (LAD) and a diagonal, the left circumflex artery (LCx) and an obtuse marginal (OM), the left main stem and the LAD or LCx and the right coronary artery (RCA) with the posterior descending artery (PDA) or ramus posterolateralis (RPL). The coronary bifurcation lesions were classified according to the Medina numeric classification and American College of Cardiology/American Heart Association ACC/AHA classifications16,17. The bifurcation lesions were treated with one or two stent techniques such as “provisional”, “culotte”, “crush”, “T-stent” and bifurcation lesion dedicated stents (Stentys™, Tryton™ and Nile® Croco). The performance of a final kissing balloon inflation was mandatory if a two stent technique was used. In case of pinching of a large side branch after provisional stenting, additional final kissing balloon inflation was attempted.
Quantitative coronary angiography
All coronary angiograms were analysed online by two independent researchers. Preprocedural and postprocedural quantitative coronary angiography (QCA) was performed by using CAAS 5.5 software (PIE Medical Imaging, Maastricht, The Netherlands). These measurements were performed for reference diameter, minimal luminal diameter and percentage diameter stenosis in three different segments of the coronary bifurcation18. An independent interventional cardiologist was asked for advice in case of a disagreement.
Statistical analysis
Continuous and categorical data were expressed as mean and percentages (±standard deviation), respectively. The Mann-Whitney U test was used to compare between two different groups consisting of continuous variables. All statistical tests were two-tailed (p<0.05 regarded as significant) and performed with SPSS for Windows version 15 (SPSS Inc., Chicago, IL, USA).
Results
Sample characteristics
The baseline characteristics of the MPCI-patients are shown in Table 1.
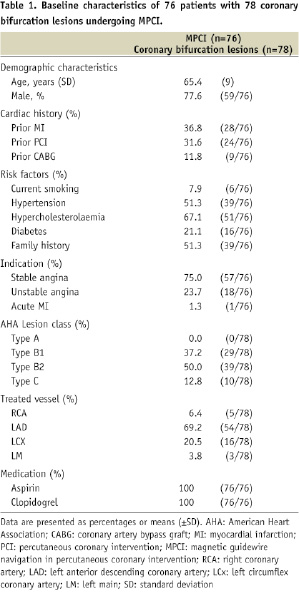
Seventy-six patients had MPCI for the treatment of total 78 coronary artery bifurcation lesions. The median follow-up period was 1.8 years (interquartile range, 1.2 to 2.5 years).
The MPCI-patients were on an average 65 (±SD 9.5) years old and 78% of the population consisted of men. Fifty-seven patients (75%) were treated due to stable angina, 18 patients (24%) due to unstable angina and one patient (1%) was treated due to an acute myocardial infarction.
The majority of the lesions involved the LAD/Diagonal bifurcation (n=54 lesions, 69%), followed by the LCx/OM bifurcation (n=16 lesions, 21%), RCA/PDA or RPL (n=5 lesions, 6%) and left main stem/LAD or LCx (n=3 lesions, 4%).
Procedural and clinical outcomes
The procedural characteristics of the coronary bifurcation lesions are showed in Table 2.
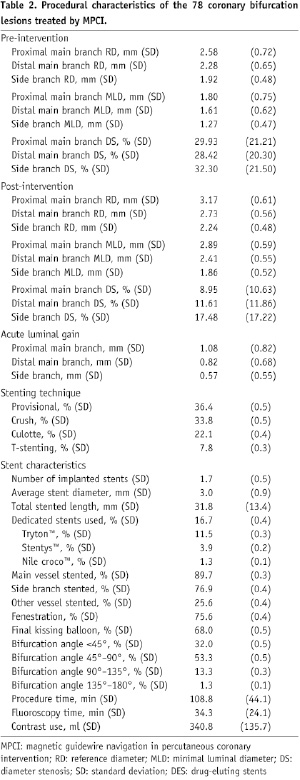
An average of 1.7±0.5 stents were implanted per patient with a total stented length of 31.8±13.4 mm. A Medina class of (1,1,1) was present in 30 bifurcation lesions (38.5%), (1,0,1) in 15 lesions (19.2%), (1,0,0) in nine lesions (11.5%), (1,1,0) in 10 lesions (13.0%), (0,0,1) in six lesions (7.7%), (0,1,0) in two lesions (2.6%) and (0,1,1) in six lesions (7.7%) (Figure 1).
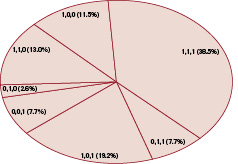
Figure 1. The Medina class of the coronary bifurcation lesions
This resulted in 64 (82%) diseased proximal main vessels, 48 (62%) diseased distal main vessels and 57 (73%) diseased side branches. The XIENCE™ V Everolimus-eluting stent (Abbott Vascular, Santa Clara, CA, USA) was the stent most implanted (42%), followed by the paclitaxel-eluting stent (35%) (TAXUS™, Express2™ or Liberté™; Boston Scientific, Natick, MA, USA). Dedicated stents were used in 13 lesions (16.7%), of which nine were Tryton™ side-branch stents (Tryton Medical, Inc., Newton, MA, USA), three Stentys™ stents (Stentys SAS, Paris, France) and one Minvasys Nile™ Croco stent (Minvasys, Genevilliers, France)). Pre-dilatation and post-dilatation was performed in 45/78 (58%) and 59/78 (76%) lesions, respectively. All 59 fenestration attempts were successfully performed. TIMI 3 flow was obtained in all patients except one, in which the magnetic wire could not successfully cross the lesion. The guidewire was entangled in an aneurysm in the LAD, which was located proximal to the bifurcation lesion. This patient was referred for an urgent coronary artery bypass because of a dissection.
The QCA analysis showed that the acute luminal gain in the proximal main branch, distal main branch and side branch were 1.08±0.82 mm, 0.82±0.68 mm and 0.57±0.55 mm, respectively. The median contrast use was 341±136 ml and the procedural and fluoroscopy times were 109±44 minutes and 34±24 minutes, respectively.
At a median of 1.8-years of follow-up, 15 patients (20%) had a MACE, of which eight postprocedural non-Q-wave myocardial infarctions within the first 48 hours. (Table 3)
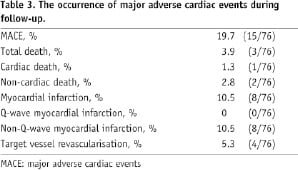
These patients had a mean CK-MB value of 33±11 ugram/litre (upper normal limit=7.5 ugram/litre) and a troponin level of 0.92±0.59 ugram/litre (upper normal limit=0.02 ugram/litre). There were four target-vessel revascularisations and three deaths, of which one cardiac death, during the follow-up period. None of the 76 patients had a stent thrombosis. The procedural time, fluoroscopy time and contrast use of the MPCI-procedures in which fenestration was performed, did not significantly differ from MPCI-procedures without fenestration (113±43 min versus 95±46 min, p=0.25; 34±25 min versus 34±24 min, p=0.95; 341±141 ml versus 341±121 ml, p=0.89, respectively), however it should be noted that other coronary lesions were treated with the same procedure.
Discussion
This study describes the angiographic characteristics of coronary bifurcation lesions and the associated procedural and clinical outcome after MPCI. The main finding of this study is that MPCI has been shown to be feasible in the treatment of coronary bifurcation lesions with good clinical and procedural success rates. All fenestration attempts were successfully performed and only one patient could not be treated due to wire entanglement in a coronary aneurysm. Fenestration was not associated with a longer procedural time, fluoroscopy time or more contrast use than procedures without fenestration, however due to the fact that other lesions beside the bifurcation lesion were also treated by the same procedure it is not possible to draw definite conclusions.
The optimal treatment of bifurcation lesions remains a delicate issue in the interventional cardiology. Stenting of bifurcation lesions are still associated with increased risk of stent thrombosis (acute, subacute and late) and higher MACE rates compared to non-bifurcation lesions19,20. Although the implantation of drug-eluting stents in bifurcation lesions have shown to be more effective in reducing restenosis, bifurcation stenting still have moderate results21-24. We previously described that the implantation of drug-eluting stents in 241 de novo bifurcation lesions with the crush-technique (n=231 patients) resulted in a MACE-free survival of 83.5% at 9-months follow-up3. In a more recent study, the crush-technique could not show superiority to provisional stenting in terms of MACE at 6-months (15.8% vs. 15%; p=NS)25. It is noteworthy that these event rates are already comparable to our study, however both studies have a follow-up period of less than one year. The main factor that ensures a good short and long-term outcome is the performance of a final kissing balloon dilatation regardless of the utilised stenting technique3,5,26,27. The procedural duration, fluoroscopy time and contrast consumption of primary PCI patients, patients with a single discrete stenosis and patients with distal and/or complex lesions treated with MPCI were all considerably lower than the findings of our study10,28,29. An explanation for the less procedure time, fluoroscopy time and the amount of contrast used compared to our study could be due to the fact that 25% of our patient population had another coronary vessel treated in the same procedure. Moreover, some patients had multiple bifurcation lesions treated during the same catheterisation.
We believe that the relatively low MACE rate found in our study could be mainly attributed to primarily using drug-eluting stents, the good postprocedural QCA results and the high degree of kissing balloon dilatation post-stent implantation.
The MNS is already successfully being used in cardiac electrophysiological procedures and has shown to be feasible in a variety of coronary lesions6,28-31. The ability of precisely steering a guidewire through the coronary arteries and (crushed) stents is an innovative approach in the treatment of coronary lesions. The actively three-dimensional controllable magnetic tipped guidewire can especially be useful in difficult vessel angles or in entering the side branch. We have already described the value of the MNS in gaining entry to the side branch through a crushed stent after unsuccessful conventional PCI13. Conventional PCI could not be completed because it was impossible to cross the stent struts of the crushed stent in spite of several different wires and techniques. The patient was treated the next morning with MPCI. After three-dimensional vessel reconstruction, the magnetic tipped guidewire could easily cross the crushed stent. Even in secondary revascularisation procedures of bypass grafts which could not be completed with conventional wires due to the associated difficult angles, it has proven its value31. When used for the treatment of distal complex lesions, MPCI have shown to reduce procedural time, fluoroscopy time and amount of contrast use compared to conventional PCI (29.9±17.6 versus 41.1±21 min, p=0.007; 7.5±7.3 versus 16.1±22.4 min, p=0.02; 122±82 versus 180±147 ml, p=0.02, respectively10.
There remain several shortcomings of the MNS, which limits its widespread use. First of all, the time it takes to get familiar with the MNS, combined with the preparation time of the system, makes it doubtful whether such a system is profitable for the treatment of bifurcation lesions. Secondly, it should be noted that the MNS is not a fully remote system, because forward and backward remote navigation is not possible. Third, in addition (crucial) time can be lost in redirecting the external magnet in the desired positions, in comparison with the fast eye-hand coordination during conventional PCI. Fourth, novel conventional wires have a more even transition of the tip with the shaft in contrast to magnetic tipped wires, which are therefore limited in flexibility. Finally, the high initial costs for the hardware and software of the MNS make it difficult to determine whether such systems are profitable to use only for specific subsets of coronary lesions.
In conclusion, the MNS showed to be feasible in coronary bifurcation lesions. The main benefit of this novel system is the easier crossing of stent struts, resulting in a high likelihood of crossing success. Due to the fact that wire crossing through the stent struts was successful in the first attempt, the fenestration process did not prolong procedure time, fluoroscopy time or contrast use. However, it remains debatable whether the pros of the MNS outweigh the cons in the treatment of bifurcation lesions. Nevertheless, a randomised controlled trial is necessary to reach conclusive results on this subject.
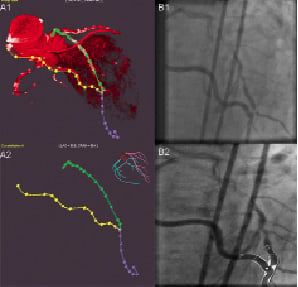

Figure 2. Case example. (A1) Three-dimensional reconstruction with the use of multislice CT. (A2) Multislice CT can be utilised to create a vessel road map. (B1) The LAD showed a significant lesion just proximal to the anastomosis of the RIMA graft (bifurcation lesion (0,0,1) with the ramus diagonalis). (B2) The QCA pre-stent implantation revealed a diameter stenosis of 64% in the side branch (minimal luminal diameter 0.89 mm; reference diameter 2.48 m) Case example. (C) Magnetic vectors are used to steer guidewire. (D) Guidewire through ostial lesion (provisional stenting technique). (E) The QCA post-stent implantation (Xience V, 3x8 mm), showed a 9% diameter stenosis in the side branch (minimal luminal diameter 2.09 mm; reference diameter 2.30 mm)