Cardiogenic shock (CS) occurs in up to 10% of all patients with acute myocardial infarction (AMI) and the mortality rate remains high, approaching 50% depending on the risk profile of the cohort. Standard therapy includes optimal fluid management as well as administration of vasopressors and inotropes on top of a causal treatment of the underlying condition. Although catecholamines play an essential role in the supportive care of CS patients, their benefits on haemodynamics appear to be counterbalanced by adverse effects such as increased myocardial oxygen demand, arrhythmogenicity, and compromise of tissue microcirculation which may translate into an increased mortality risk1. Mechanical circulatory support (MCS) is an alternative to increase systemic blood flow while avoiding the possible cardiotoxicity and morbidity of medical therapy. Furthermore, MCS, with multiple devices available (Figure 1), may be the only option to achieve haemodynamic stability in patients with refractory CS2. Consequently, MCS are widely used despite scarce evidence supporting their beneficial impact on clinical outcome. In this issue of EuroIntervention, three papers are included aiming to elucidate further the role of MCS in CS in daily clinical practice.
Ellert and co-workers present a case report highlighting two relatively new indications for Impella® devices (Abiomed, Inc., Danvers, MA, USA)3.
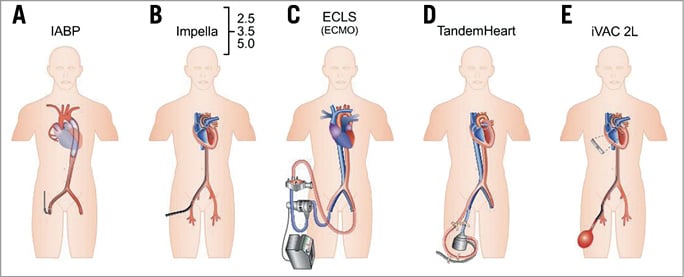
Figure 1. Schematic drawings of current percutaneous mechanical support devices for CS. A) Intra-aortic balloon pump (IABP). B) Impella®. C) Extracorporeal life support (ECLS). D) TandemHeart™. E) iVAC2L (PulseCath b.v., Amsterdam, the Netherlands).
A patient with refractory out-of-hospital cardiac arrest was admitted to the catheterisation laboratory. First, an Impella CP® was implanted under ongoing cardiopulmonary resuscitation leading to a return of spontaneous circulation. Second, despite revascularisation, the patient developed right ventricular heart failure and therefore an additional Impella RP® was used for right ventricular support. Previously, extracorporeal life support (ECLS) was considered the only MCS able to provide adequate support in refractory cardiac arrest as well as biventricular heart failure. Based on small case series as well as on the current case report, Impella CP and Impella RP appear to be potential alternatives to ECLS in these indications.
The study by Overtchouk et al focuses on ECLS with or without IABP support4.
The ACTION study group, acknowledged worldwide for the rigorous performance of clinical trials, presents data from the retrospective Pitié-Salpêtrière Cardiogenic Shock Registry on a cohort of 106 patients in refractory CS due to AMI undergoing ECLS at one single institution between 2007 and 2013. One major finding of the study was that neither percutaneous coronary intervention (PCI) itself nor success of revascularisation was associated with a survival benefit. This is in contrast to the results of the Should We Emergently Revascularize Occluded Coronaries for Cardiogenic Shock (SHOCK) trial which clearly demonstrated the prognostic importance of early revascularisation in CS complicating AMI5. Potential explanations for the diverging results could be the differing risk profiles of the cohorts studied, as a large number of patients enrolled in the current registry may have been in a futile clinical situation, where even the best therapy is not able to change the clinical course. Another reason could be the small sample size resulting in low statistical power. Further, immediate complete revascularisation did not impact on survival. This observation is not fully in line with recent results of the Culprit Lesion Only PCI versus Multivessel PCI in Cardiogenic Shock (CULPRIT-SHOCK) trial which demonstrated a higher risk of death following immediate multivessel PCI as compared to culprit-lesion-only PCI. The similar clinical outcome following an aggressive reperfusion therapy may be indicative of a relative survival benefit in these high-risk patients6. Another very interesting finding was the improved survival observed in patients treated with intra-aortic balloon pump (IABP) in combination with ECLS. The authors interpret this as a result of prevention of left ventricular overload during ECLS therapy achieved by IABP support. While left ventricular unloading by adjunctive use of either IABP, Impella or TandemHeart™ (CardiacAssist Inc., Pittsburgh, PA, USA) on top of ECLS is very appealing, the current findings need to be interpreted in the methodological context of the analysis. It is important to emphasise that ECLS was either inserted immediately, <24 hrs or >24 hrs after coronary angiography, whereas IABP support was always initiated at the time of coronary angiography in approximately two thirds of patients. The authors state that early ECLS implantation was performed in patients at much higher risk with more profound multiple organ failure. Consequently, it is plausible that IABP insertion prior to ECLS is rather an indirect indicator of less severe CS at presentation in this cohort than directly influencing clinical outcome. Finally, the findings of non-randomised observational studies with limited sample size are always vulnerable to influences of multiple confounders and selection bias, especially in small cohorts with limited statistical power. Nevertheless, the hypotheses generated by Overtchouk and colleagues are of great interest and should be tested in larger cohorts and randomised trials.
The third analysis, performed by Strom et al, is based on data of hospitalisations of US adults with a discharge diagnosis of CS from 2004 until 2014 in the National Inpatient Sample (NIS)7.
A total of 183,516 hospitalisations were included of which 47,636 (30%) received MCS. An apparent increase in CS hospitalisations was observed. Unfortunately, a valid explanation for this finding cannot be provided as the results are based on an administrative database. Potential reasons could be a more liberal definition of CS or a more frequent diagnosis due either to early recognition, as a result of reimbursement issues based on diagnosis-related groups, or in order to improve operator/hospital outcomes as in some US states AMI with CS is excluded from outcome reporting8,9. The most widely used MCS was IABP, with declining rates in recent years, which could be attributable to the publication of the Intraaortic Balloon Pump in Cardiogenic Shock II (IABP-SHOCK II) trial and changes in guideline recommendations10. A parallel increase of ECLS and active left ventricular assist devices was observed. Patients with MCS had a lower mortality as compared to patients undergoing standard therapy without MCS. This could be partly explained by the differing baseline profiles of the cohorts, as patients treated with MCS were younger and had a lower prevalence of comorbidities. Further, MCS use was associated with more aggressive treatment including revascularisation procedures. Therefore, it remains unclear whether MCS itself or optimal additional therapy in patients with lower baseline risk explains the beneficial outcome of MCS recipients.
In summary, the three papers clearly demonstrate that MCS is part of our daily clinical practice although multiple open questions remain with respect to appropriate device selection, timing of insertion, patient selection and optimal management of complications. To date, there is no hard evidence clearly demonstrating a mortality reduction by MCS. Further, the benefits on haemodynamics and peripheral perfusion must be weighed against the complications associated with the invasiveness. Adequately powered randomised clinical trials are warranted to address this lack of evidence. Until then, routine use of MCS in all patients is not recommended, although their selected use is an important part of contemporary CS treatment.
Conflict of interest statement
The authors have no conflicts of interest to declare.