Abstract
Among lesions with in-stent restenosis (ISR), the in-stent chronic re-occlusions (ISR-CTO) is a subset with particularly unfavourable features regarding both the repeat procedure success and the prevention of lesion recurrence. A review of the literature and personal databases reveals that the prevalence of complete occlusive ISR represents about 5-10% of all CTO lesions, with little evidence regarding the successful long-term treatment. In fact, these lesions had been excluded from large contemporary trials dealing with the best modality for ISR management, and which showed eventually the superiority of drug-eluting stents (DES) as compared to brachytherapy. Only a limited experience exists with brachytherapy for ISR-CTOs, showing an inferior outcome as compared to non-occlusive ISRs. The lack of large study experience is true also for DES, so that only anecdotal experience in small series of patients is available. In some of the recent studies of DES in CTOs, again, ISR-CTOs were not included. Our own experience shows a slightly lower primary success rate of about 70% in ISR-CTOs as compared to 85% in primary CTOs, with a slightly higher recurrence rate with DES of 25%.
ISR-CTOs are a clinical problem that had not been systematically addressed. However, we hope that this lesion subset may be of less relevance in the future when the use of DES in lesions which are prone for lesion recurrence will lead to less diffuse and occlusive ISR, and leaves rather focal and better manageable recurrent lesions.
Introduction
With the advent of drug-eluting stents (DES) the incidence of in-stent restenosis (ISR) is steadily declining, even in complex coronary lesions such as chronic total coronary occlusions (CTOs), although it is not eliminated. The fear of late stent thrombosis, the individual limitation of extended double antithrombotic regimens as well as economic restraints are currently leading to a DES rate roughly of about 50%, which leaves restenosis of bare metal stents (BMS) as a therapeutic problem. Therapeutic options for in-stent restenosis (ISR) are now primarily the implantation of DES1, but for focal lesion repeat percutaneous coronary intervention (PCI) may still be a valid option2-5. Brachytherapy as an effective treatment option is now abandoned because of its technical challenges and the superiority of DES for this indication6-10. Of course surgery remains an option, especially with multivessel lesions and recurrent ISR, however with a perioperative mortality that is higher than for PCI11.
A subset of ISR is the total chronic re-occlusion within a stent (ISR-CTO), either as the result of a silent late thrombotic stent occlusion, or as the consequence of slow diffuse restenosis. The rate of complete stent occlusions in BMS was reported to be 8%2. These lesions represent a specific problem for reinterventions, as the primary technical success rate in occlusive lesions will be lower than with non-occluded ISR, the treatment with DES will require extensive secondary coverage of the original stented area and beyond12, with a potentially higher lesion recurrence and late stent thrombosis risk.
The best approach to ISR-CTOs is not well understood due to the fact that these lesions are often excluded from randomised trials on ISR such as TAXUS V ISR9 or SIRS10), nor are they included in trials on CTOs, such as PRISON II13 or the upcoming PRISON III (personal communication by Dr. Suttorp). In the case-control PACTO study on CTOs, the number of included ISR-CTOs was not specifically mentioned, but four patients with this lesion characteristic had been included14.
ISR-CTOs in the literature
As mentioned above, totally occluded in-stent restenosis had not been studied in the recent trials of DES versus brachytherapy for ISR treatment. Even though both the Taxus V ISR and the SISR study report a low number of totally occluded arteries in their baseline data description (1% for Taxus, 6% for Cypher)9,10, these lesions had been explicitly mentioned in the exclusion criteria for both studies. Therefore, the nature of these lesions with respect to the definition of a CTO is unknown15, and the results for this lesion subset is not reported.
From the era of brachytherapy there is a report by Nikolsky and co-workers that specifically deals with the subset of ISR-CTOs16. Among 103 ISRs, they had 15 ISR-CTOs (14.5%). This is a slightly higher prevalence than reported by Mehran and co-workers of 8%2. They used a 55 mm gamma radiation source length. Even though they had only clinical follow-up, 10 of 15 patients (67%) treated with ISR-CTOs experienced a major cardiac adverse event as compared to 28% in non-CTO ISRs. In a subanalysis from the RENO registry of brachytherapy using beta-irradiation, 84 lesions of about 1,100 lesions were CTOs, and among these 54 were ISR-CTOs17. Overall, in CTOs, beta-irradiation leads to a 21% target revascularisation rate, a 13% re-occlusion rate, and – above all – a 10% late stent thrombosis rate. The ISR-CTOs seemed to have less severe complications as compared to radiation as primary CTO treatment, but the binary restenosis with 35% and the re-occlusion rate with 11% was still considerable, and definitely higher than we expect in CTOs treated with DES.
Description of the problem
For in-stent re-occlusion the specific problems are a lower primary technical success rate, as it is basically a CTO, and in case of successful crossing, the need for extensive secondary stenting with DES to cover the re-occluded stent with sufficient overlap to prevent an edge recurrence. The fact that, in addition to a large plaque load, there will be at least two stent layers, leads to a higher stent recoil, and high inflation pressures and postdilatation pressures with adequate stent sizes will be required. To counteract the expected higher lesion recurrence, adding both the adverse factors of a CTO and a stent-recurrence, an optimum stent apposition and expansion is required, which could be best achieved by intravascular ultrasound guidance. This may, then, also minimise the potentially higher late stent thrombosis risk resulting from multi-stent layers.
Indication for treating an ISR-CTO
The indication should be based on the same criteria that every CTO attempt is based on, i.e., clinical symptoms clearly related to the lesion, evidence of ischaemia, and viability. In ISR-CTOs, one other aspect is also important from the procedural point of view, which is the remaining stent-free segment distal to the lesion. In some cases, specifically with long stented segments, this could be the result of a worsening bail-out situation where one stent was added to the other with ever extending dissections. If there is only a small territory of normal vessel left distally, it might not be worthwhile trying to open such an ISR-CTO, given the fact that it would be necessary to cover the whole stented segment plus additional extra length at the stent borders (Figure 1).
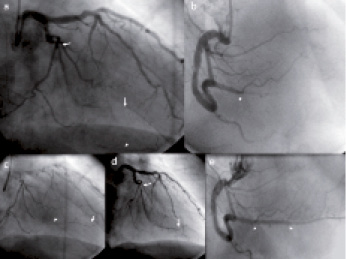
Figure 1. A 74 year old man with stable angina CCS 3 and a previous PCI with multiple stents in a large second obtuse marginal branch. Extensive stenting (panel a: between the 2 arrows) was triggered by extending dissections during the original procedure. Only small distal territory of distal remaining vessel is visible (panel c). The same frames show a distal collateral filling to a large posterior descending branch of the RCA (arrow head in panel a), with the PDA occlusion visible in panel b (arrow head). The occluded stents could be passed with a Miracle 3G (ASAHI Intecc, Aichi, Japan) (arrow) supported by a QuickCross microcatheter (Spectranetics Inc., Colorado Springs, CO, USA ) (arrow head), but with this diffuse stent occlusion and minimal run-off, the result after dilatation is not satisfactory (panel d: between arrows). No additional stenting was done. Instead, the PDA was recanalised and stented (panel e), which relieved the patient’s symptoms.
It is always helpful to have information of the original procedure during which the stent was implanted. A decisive question is in stents implanted for dissections complicating the original procedure, whether there is clear evidence that the distal true vessel lumen had been gained during that procedure, or whether the stents ended up in a false lumen with poor run-off, which was then also the reason of the stent re-occlusion. Such ISR-CTOs are less likely to be retreated successfully, as it would require a re-entry into the distal vessel lumen from a stent that is occluded in the false lumen.
Crossing the ISR-CTO
The defining problem is the passage of the ISR-CTO with a wire. There is the risk of deviation of the wire towards the vessel border which then may slip through the struts and pass along outside of the struts. Even if the wire re-enters, such a situation needs to be recognised before a balloon is advanced in order to avoid deformation of the original stent. Careful assessment of the wire within the stent from bilateral views is needed. If a balloon is then following the wire, but gets stuck within the stent, this might hint at a wire passage through the struts. As the restenotic material within a stent is usually not rigid, the balloon should pass with ease, and any obstruction must raise suspicion.
Therefore it is important to select wires according to the situation one encounters during the procedure. It might be feasible to start with a hydrophilic soft PTFE wire, but these wires are less stearable and may slip outside the stent. In such a case, a typical recanalisation wire, such as a Miracle type wire, should be used. In very old ISR-CTOs, the plaque composition within the CTO may mimic that of a naturally occurring CTO with formation of proximal and distal caps. In such a case, penetration of the cap is required if it becomes fibrotic and hard. As in any other CTO, this is a situation where a Confianza type wire with tapered tip to penetrate is required. The entry point should be selected from bilateral views close to the centre of the vessel. After successful penetration, and following with a microcatheter or OTW balloon, it might be a good idea to exchange then for a PTFE wire to advance further.
As with primary CTOs, there is no general rule of engagement, as lesion characteristics are variable and hardly predictable from the angiographic image, but one important issue applies for all CTO procedures, which is the control of the wire position during all stages of the procedure. That will specifically require contralateral injection for exiting the stent into the true lumen. While we can be sure of the correct general wire position during passage of the ISR-CTOs within the struts because of the radio-opacity of the struts themselves (provided that we know that the stent was indeed implanted in the true lumen), the exit from the stent is the crucial step.
There is no published data on the success of recanalisation in ISR-CTOs as compared to primary CTOs. In personal experience (GSW) between 2005 and 2007, only 5% of all CTOs treated were ISR-CTOs, and crossing success was only 70%, even with the available options of a retrograde approach18,19. On the other hand, the success rate in primary CTOs was 85% during that same time period. A recent presentation of the combined database of the Columbia University Medical Center and the group of Antonio Colombo in Milan, Italy, reported a higher success rate in ISR-CTOs of 76.6% as compared to 65.5% in native CTOs (Roxana Mehran, presented at 6th CTO Summit, New York, USA, February 2009). They made an overview of 149 ISR-CTOs, which made up 10.9% of all of their included CTOs. Data on this subject are scarce and inhomogeneous.
Prevention of lesion recurrence
Based on the concept that an in-stent recurrent lesion contains a large plaque load, ablative therapies such as rotablation or excimer-laser had been tried, but were ultimately not successful20-24, and therefore are currently not advised for ISR-CTOs prior to any definite treatment. Based on the aforementioned trials with DES versus brachytherapy9,10, an additional DES stent implantation is the method of choice (Figure 2).
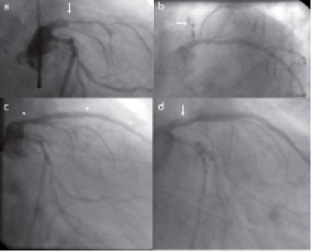
Figure 2. A 65 year old male with proximally occluded LAD stents (2 BMS) with tapering lumen at the entry into the occluded stent (panel a & b: arrows). The recanalisation was achieved with a Miracle 3G (ASAHI Intecc, Aichi, Japan) supported by a QuickCross microcatheter (Spectranetics Inc., Colorado Springs, CO, USA ), and 2 stents (Taxus Liberté; Boston Scientific, Natick, MA, USA) implanted to cover the diffusely occluded stent (panel c: arrow heads). Despite using inflations with 3.5 mm balloons, the distal stent seems not well expanded. At follow-up seven months later, the stent is widely open with a non-significant restenosis at the stent entry. (panel d: arrow).
In the absence of specific data on the outcome in ISR-CTOs from these and other trials, we have had to rely on personal experience and anecdotal evidence. In the PACTO long-term study of 95 patients with a CTO treated with the Taxus Express stent25, eight had a ISR-CTO. One patient with a TIMI 2 flow after the recanalisation procedure had a re-occlusion (12.5%), which is an adverse factor for late patency, irrespective of the initial lesion characteristic. All other vessels with a TIMI 3 flow after PCI remained patent, with only one focal restenosis (12.5%), which occurred in a patient who had been treated for the second recurrent stent re-occlusion. Thus, the overall recurrence rate in this small sample was 25%, about double what is observed in primary CTOs.
Drug-eluting balloons in ISR-CTOs as a future option?
There might be arguments against the use of DES in long-stented diffuse ISR, and ISR-CTO is the worst case scenario based on the fact that an additional layer of metal together with antiproliferative activity may impair subsequent re-endothelialisation and thus render the treated lesion susceptible to future late thrombotic occlusions. There are no long-term data from neither Taxus V ISR nor SISR on that specific risk. On the other hand, several layers of metal may trigger stent strut fractures as a possible cause of recurrent ISR26. Figure 3 shows the problems that may arise with multiple layers of stents, leading, despite obviously antiproliferative activity, to recurrent restenosis most likely due to mechanical problems with repeated “full metal jackets” .
A new concept has evolved of delivering the required antiproliferative agent without additional stenting through a drug-eluting balloon. After the initial experience27,28, a randomised trial of a paclitaxel-eluting balloon with the paclitaxel-eluting drug stent showed encouraging results (PEPCAD II, presented at TCT 2007). Whether it will also be a feasible alternative for ISR-CTOs remains to be demonstrated.
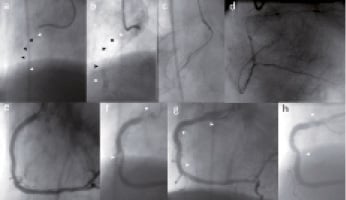
Figure 3. A 66 year old male with initial implantation of 4 stents (BMS) during a complex primary PCI, and 6 months later complete ISR-CTO (arrow heads) from the ostium down to the distal third of the RCA (panel a & b). Despite this unfavourable anatomy, it was possible to advance a Miracle 3G (ASAHI Intecc, Aichi, Japan) supported by a QuickCross microcatheter (Spectranetics Inc., Colorado Springs, CO, USA) (panel c), and confirmed by retrograde injection (panel d). Four stents (Taxus Liberté; Boston Scientific, Natick, MA, USA) were implanted to cover the original stent completely (panel e). After 5 months, two focal recurrent restenosis occurred which were then retreated by balloon dilatation only (not shown). Ten months later, angiography because of recurrent angina revealed a high grade subtotal ostial and a mid RCA ISR (panel f: arrow heads). After re-dilatation, two Xience stents (Abbott Vascular, Redwood City, CA, USA) were implanted (panel g: arrow heads). Four months later the patient was again admitted with chest pain, this time a focal restenosis in the mid RCA at a location of extensive vessel movement was observed (panel h), and a non-significant lesion at the ostium (arrow heads). This time re-dilatation was performed, with option of CABG in case of a fourth recurrence.
Summary
This paper summarises the presently available data on ISR-CTOs, which is very limited given the fact that this lesion subset makes up at least 10% of all in-stent lesion recurrences. On the other hand, this problematic subset may become less important with the widespread use of DES; specifically in those lesions which carry a high likelihood of lesion recurrence such as primary CTOs, and long lesions in diffusely diseased arteries and/or diabetics. The pattern of restenosis in DES seems to be less diffuse and therefore also occlusive lesions will be found less frequently.
Despite the above mentioned foreseeable future development, ISR-CTOs will still be observed in symptomatic patients and have to be dealt with. It appears that the primary success rate of recanalisation is even lower than in primary CTOs, but the prevention of lesion recurrence may be less of a problem than in the era of BMS or brachytherapy with DES. Future developments, such as drug-eluting balloons, could be good options to avoid “double full metal jackets”.
It became obvious during the research for this paper that the published data are very scarce on this subject. We should try to obtain a broader database of these lesions through collaborative efforts from centres which are particularly experienced and have higher volumes of CTOs in their PCI population.