Aortic stenosis (AS) haemodynamic severity is typically quantified using aortic valve area (AVA) and the transvalvular mean gradient (MG)1. The 2012 European Society of Cardiology/European Association of Cardiothoracic Surgery guideline consensus document defines severe AS as an MG >40 mmHg and an AVA <1.0 cm2 in the presence of a normal cardiac output1. However, because MG is directly proportional to the square of transvalvular flow, even small reductions in stroke volume can result in significant reductions in the pressure gradient (Figure 1). Furthermore, stroke volume reductions can occur even in the presence of apparently normal left ventricular ejection fraction (LVEF)2. Consequently, severe AS (AVA <1.0 cm2) may coexist with a low MG (<40 mmHg) among patients even with preserved LVEF, leading to guideline discordant haemodynamic parameters of AS severity2. The 2014 American Heart Association/American College of Cardiology guidelines on valvular heart disease therefore recognise three subtypes of severe AS, i.e., high-gradient AS (HGAS), low-flow, low-gradient AS with reduced LVEF (LEF-LG), and paradoxical low-flow severe AS (PLF-LG)3.
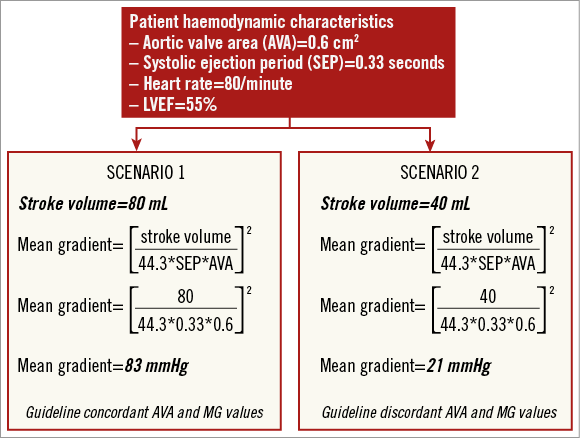
Figure 1. Relationship between stroke volume and mean gradient. A hypothetical patient with preserved left ventricular ejection fraction (LVEF) and severe AS due to a valve area of 0.6 cm2, a systolic ejection period (SEP) of 0.33 seconds and a heart rate of 80/min will have a calculated mean gradient (MG) of 83 mmHg assuming a normal cardiac output of 6.4 L/min (![]() ) according to Gorlin’s formula. However, the same patient would end up with a calculated MG of 21 mmHg were the cardiac output to fall to 3.2 L/min, assuming the AVA, heart rate and SEP remained constant. The patient still has severe AS even though the MG and AVA are now discordant with the guidelines criteria.
) according to Gorlin’s formula. However, the same patient would end up with a calculated MG of 21 mmHg were the cardiac output to fall to 3.2 L/min, assuming the AVA, heart rate and SEP remained constant. The patient still has severe AS even though the MG and AVA are now discordant with the guidelines criteria.
Patients with “classic” LEF-LG severe AS have long been recognised as being among the highest risk patients to undergo conventional surgical aortic valve replacement (SAVR) because of a high associated perioperative mortality4-6. Alternatively, LEF-LG patients assigned to medical therapy have a dismal prognosis6. However, LEF-LG patients surviving the perioperative period have good clinical outcomes with significant improvements in LVEF occurring even in the absence of preoperative flow reserve5. As compared with conventional SAVR, transcatheter aortic valve implantation (TAVI) may offer a unique solution for patients with LEF-LG severe AS (who by definition are high-risk patients) owing to its less invasive character7-9.
In this issue of EuroIntervention, Lauten et al and Amabile et al present the largest series to date of TAVI among patients with different subtypes of AS enrolled in the German (GARY) and French (FRANCE2) national TAVI registries, respectively10,11. Lauten et al analysed the outcomes of 3,908 patients with severe AS undergoing TAVI for different subtypes of severe AS using data from the GARY registry10. The primary endpoint was all-cause mortality at hospital discharge and one year. Distinct gender differences were observed between groups: LEF-LG patients were predominantly male (66.3%), whereas PLF-LG and HGAS patients were mostly female (57.8% and 60.7%, respectively)10. LEF-LG patients were higher risk and had a higher prevalence of comorbidities, including pulmonary hypertension, coronary artery disease and moderate/severe mitral regurgitation. As compared with HGAS, LEF-LG patients had both higher in-hospital (4.9% vs. 7.8%, p=0.029) and 12-month mortality rates (19.8% vs. 32.3%, p<0.001). Conversely, those with PLF-LG severe AS had similar in-hospital and one-year outcomes to HGAS patients10.
Amabile et al adopted a slightly different approach and aimed to assess the impact of a low preprocedural mean gradient (<40 mmHg) on cardiovascular mortality following TAVI11. Of 3,933 consecutive patients enrolled in the FRANCE2 registry, almost a quarter (24%) had a low MG (13.3% had LEF-LG severe AS and 10% had PLF-LG severe AS). As compared with HGAS, patients with low-gradient AS had significantly lower 30-day (93.5% vs. 90.6%, p<0.001) and one-year (88.1% vs. 81.3%, p<0.001) cardiovascular survival rates. Similar to the observation by Lauten et al, this was predominantly driven by a lower cardiovascular survival rate among the subgroup of patients with LEF-LG (77.2%) versus the other AS subgroups (PLF-LG [86.6%] vs. HGAS/normal LVEF [89.7%] vs. HGAS/low LVEF [84.8%]). Furthermore, a low MG was an independent predictor of cardiovascular death in the overall patient population, suggesting that a low MG could be used as a marker to identify high-risk patients11. Echocardiographic follow-up data demonstrated that LVEF improved in both LEF-LG and low LVEF/HGAS patients following TAVI to a similar extent11.
What can we learn from these large-scale observational studies? The clear message is that patients with LEF-LG severe AS have the poorest outcome after TAVI. Despite acceptable in-hospital mortality rates, which have actually improved from 16.1% in the German TAVI registry (2009-2010) to 7.8% in GARY (2011), one-year mortality rates have remained stubbornly high (36.9% and 32.3%, respectively). Further studies are needed to improve patient selection and/or to assess whether better management of comorbidities such as concomitant coronary artery disease or mitral regurgitation may further help improve clinical outcomes among LEF-LG patients.
Major limitations of both studies have been acknowledged by the authors and relate to the lack of dobutamine stress echocardiography (DSE) and stroke volume data in both groups. Lack of DSE data precludes a comparative analysis of clinical outcomes among LEF-LG patients with and without flow reserve. The latter group in fact has the highest perioperative mortality of all with conventional SAVR and may have most to gain with either TAVI4 or just being treated with optimal medical treatment.
To conclude, the studies by Lauten et al and Amabile et al are the largest to date to demonstrate the clinical outcomes of patients according to AS subtype. Patients with LEF-LG severe AS are at highest risk and carry the poorest prognosis. As a simple rule, the higher the transvalvular gradient (despite the low LVEF), the better the chance of LVEF improvement and the better the overall prognosis is. Conversely, the lower the MG, the higher the risk of the intervention and the poorer the long-term prognosis becomes. This needs to be kept in mind.
Future studies in this patient subgroup should address the question of whether TAVI is still utile and not already futile in patients with low LVEF and low MG, and which factors need to be evaluated before a TAVI intervention or aortic valve surgery. Stress and viability testing play an important role during the screening phase for TAVI, as patients with LEF-LG AS may suffer from a combination of cardiac problems, and the poor LVEF might not be induced by the aortic valvular disease. Consequently, information regarding the potential improvement of LVEF and on the degree of myocardial fibrosis as well as viability appears crucial.
Of note, symptomatic improvement may only be achieved if LVEF increases after TAVI in this setting. Last but not least, in order to improve midterm and long-term clinical outcomes, especially by reducing the risk of cardiovascular mortality, not only technical success but also advanced strategies for the post-TAVI period need to be defined and developed, e.g., specific and intensive medical treatment of heart failure as well as electrophysiological therapeutic options need to be considered.
Conflict of interest statement
P. Wenaweser has received honoraria and lecture fees from Medtronic and Edwards Lifesciences and an unrestricted research grant from Medtronic to the University of Bern, Switzerland. C. O’Sullivan has no conflicts of interest to declare.