Introduction
Up to 40% of patients with aortic stenosis (AS) present with a low-flow, low-gradient (LF LG) pattern characterised by a discordance between an aortic valve area (AVA) <1.0 cm2, indicating severe AS, and a mean transvalvular gradient <40 mmHg, indicating non-severe AS, in the context of a low-flow state (stroke volume index <35 ml/m2). This LF LG-AS remains one of the most challenging entities to manage in terms of diagnosis, prognosis, and therapeutic decision-making. The outcomes for the different forms of AS, including LF LG, are essentially determined by the severity of AS and the extent of the associated cardiac damage. However, the heart has four chambers, and the assessment of cardiac damage should not be restricted to LV systolic function but should also include the other cardiac chambers. Généreux et al were the first to propose a classification scheme for the comprehensive staging of cardiac damage in AS1. Subsequently, several studies have validated and adapted this concept in various AS populations to enhance risk stratification and better determine the optimal timing and type of aortic valve replacement (AVR)2.
In this issue of EuroIntervention, Nakase et al3 present the results of a retrospective analysis of the nationwide SwissTAVI Registry including 2,090 patients who underwent transcatheter aortic valve implantation (TAVI) between 2007 and 2022 and who were subdivided according to the flow-gradient pattern: i) high-gradient AS, regardless of flow status (HG-AS); ii) “classical” LF LG with reduced ejection fraction (left ventricular ejection fraction [LVEF] <50%); iii) “paradoxical” LF LG with preserved LVEF; and iv) normal-flow LG AS (NF LG-AS), defined as small AVA with LG but in the context of a normal flow and preserved LVEF. About half of the patients presented with LG-AS, of whom 70% were in LF. Mortality was highest in patients with classical LF LG-AS (63.0% at 5 years), followed by paradoxical LF LG-AS (53.0%), and then HG-AS (46.1%), and NF LG-AS (41.1%).
The main findings of the study by Nakase et al3 are as follows: i) The majority (73.6%) of patients with classical LF LG-AS with reduced LVEF had evidence of advanced cardiac damage, which was defined in this study as stage 3 or 4, followed by paradoxical LF LG-AS with preserved LVEF (55.6%), NF LG-AS (51.6%), and HG-AS (50.6%). ii) Mortality in both early and advanced stages was highest in patients with classical LF LG-AS, followed by paradoxical LF LG-AS with preserved LVEF, HG-AS, and NF LG-AS. iii) Advanced cardiac damage conferred increased mortality risk in all AS subtypes but with a different impact across subtypes. Indeed, the absolute mortality excess rates at 5 years between advanced versus early cardiac damage were +22% in paradoxical LF LG, +18% in HG, +14% in NF LG, and +10% in classical LF LG-AS, which are consistent with previous reports4.
Refining the classification scheme for cardiac damage staging
The staging classification scheme initially proposed by Généreux et al was essentially based on echocardiographic parameters, except for atrial fibrillation which was included in stage 2 (Figure 1)1. This classification has since been adapted by Tastet et al2 for application to asymptomatic AS patients. In particular, the LVEF threshold was raised from 50% to 60% for qualification in stage 1. Indeed, a substantial proportion of AS patients with LVEF between 50% and 60% have subclinical LV systolic dysfunction and are, therefore, at increased risk for adverse cardiac events versus those with LVEF >60%. In the present study, Nakase et al3 proposed some incremental modifications to this classification scheme. The criterion of mean pulmonary artery pressure ≥25 mmHg measured by cardiac catheterisation was added to stage 3 (Figure 1). The definition of right ventricular (RV) systolic dysfunction in stage 4 was further refined by using a multiparameter approach that includes not only a tricuspid annular plane systolic excursion <1.7 cm, as previously proposed, but also a tricuspid annulus S’ velocity <9.5 cm/s, and RV fractional area change <35%.
One of the most striking findings of the present study is the high prevalence of advanced cardiac damage, with 74% of patients in the classical LF LG group being in stage ≥3, which is much higher than the prevalence of 34% recently reported in the National Echo Database of Australia for the same LF LG subtype5. This difference may be related to the higher risk profile of the classical LF LG group and the use of different criteria for defining stage 3 or 4 in the study of Nakase et al (Figure 1)3.
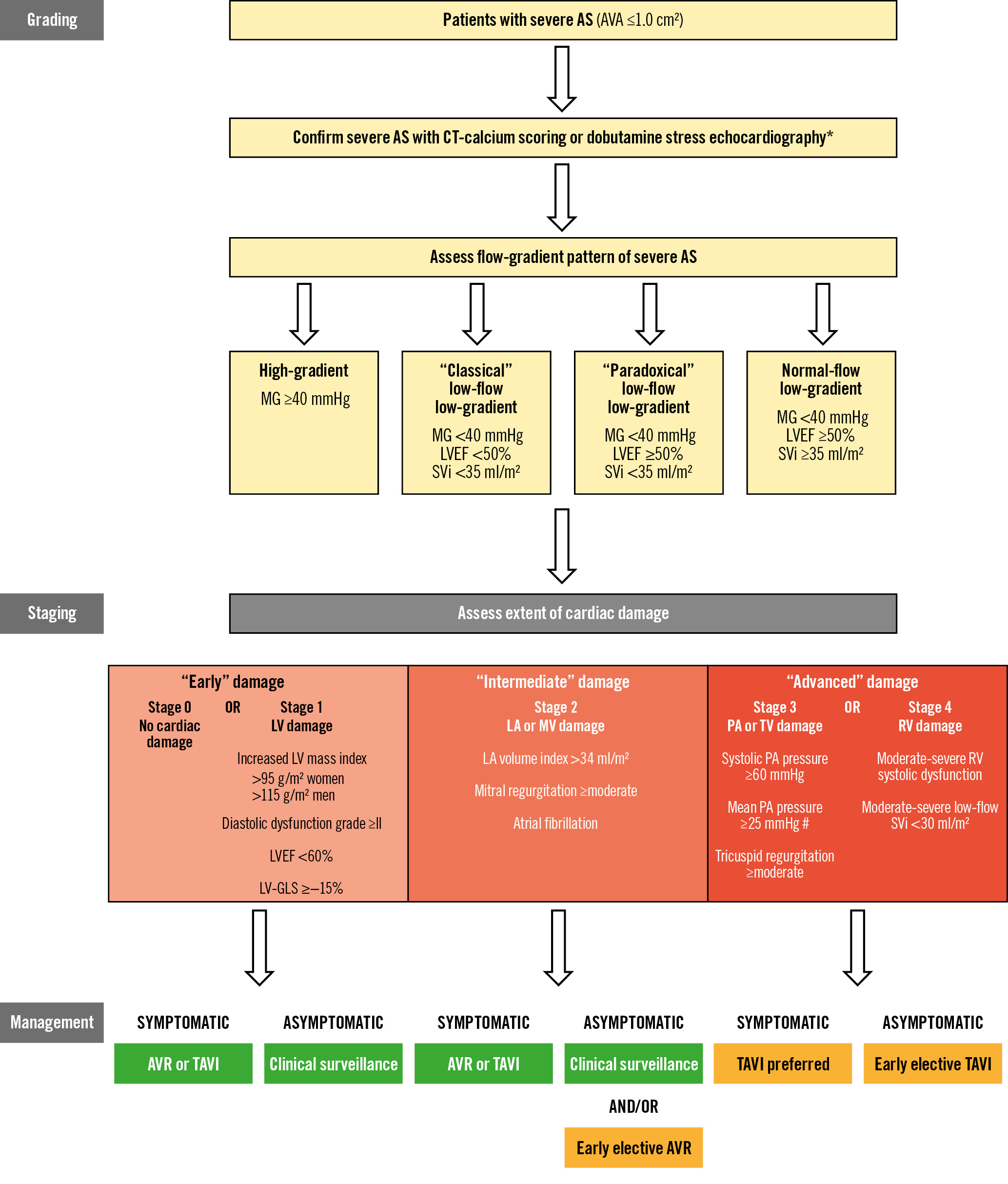
Figure 1. Algorithm for risk stratification and management of severe AS. The patient qualifies for a given stage if at least one of the proposed criteria for this stage is met. * The confirmation of AS severity by non-contrast CT or dobutamine stress echocardiography is only required for LG patterns. # Pulmonary artery pressure estimated by Doppler-echocardiography or directly measured by cardiac catheterisation.
The orange boxes in the Management section contain therapeutic options that are proposed by the authors in light of the recent literature but that are not yet supported by the practice guidelines. AS: aortic stenosis; AVA: aortic valve area; AVR: aortic valve replacement; CT: computed tomography; LA: left atrial; LV: left ventricular; LVEF: left ventricular ejection fraction; LV-GLS: LV global longitudinal strain; MG: mean gradient; MV: mitral valve; PA: pulmonary arterial; RV: right ventricular; SVi: stroke volume index; TAVI: transcatheter aortic valve implantation; TV: tricuspid valve
Impact of cardiac damage staging on outcomes
The enhanced cardiac damage classification scheme proposed by Nakase et al3 performs well for risk stratification in all flow-gradient patterns. Indeed, regardless of these patterns, the 5-year mortality rate was significantly increased in patients with advanced cardiac damage, i.e., damage to the right-side unit of the heart. Prior studies also reported an increased risk of mortality following TAVI in AS patients with concomitant pulmonary hypertension, significant tricuspid regurgitation or RV systolic dysfunction67. Several studies also reported that surgical AVR is associated with significant deterioration of RV systolic function and, consequently, with new onset of cardiac damage stage 4, whereas TAVI appears to better preserve RV function6. These findings provide support for the selection of TAVI rather than surgery in patients with advanced cardiac damage (Figure 1).
Although the present study defined “advanced” cardiac damage stage as stage ≥3, previous studies found that stage ≥2 is associated with an increased risk of short-term mortality in asymptomatic severe AS2. Hence, stage ≥2 should probably not be pooled with stages 0 and 1 in “early damage” but rather should be considered “intermediate damage” (Figure 1).
The orange boxes in the Management section contain therapeutic options that are proposed by the authors in light of the recent literature but that are not yet supported by the practice guidelines. AS: aortic stenosis; AVA: aortic valve area; AVR: aortic valve replacement; CT: computed tomography; LA: left atrial; LV: left ventricular; LVEF: left ventricular ejection fraction; LV-GLS: LV global longitudinal strain; MG: mean gradient; MV: mitral valve; PA: pulmonary arterial; RV: right ventricular; SVi: stroke volume index; TAVI: transcatheter aortic valve implantation; TV: tricuspid valve
Clinical implications and future perspectives
The very high rates of mortality and, thus, of treatment futility in patients with advanced cardiac damage stage are alarming and raise the concern that we probably intervene too late in the course of this disease, especially in patients with LF LG-AS. Whether an earlier referral to intervention in patients with HG- or LG-AS would help prevent the development of irreversible cardiac damage is still unknown. Several ongoing randomised trials will determine whether early TAVI improves outcomes compared to clinical surveillance in patients with severe asymptomatic AS (Evaluation of TAVR Compared to Surveillance for Patients With Asymptomatic Severe Aortic Stenosis [EARLY TAVR]), moderate AS and systolic heart failure (Transcatheter Aortic Valve Replacement to UNload the Left Ventricle in Patients with ADvanced Heart Failure [TAVR UNLOAD]), and moderate AS with evidence of cardiac damage stage ≥1 (Management of Moderate Aortic Stenosis by Clinical Surveillance or TAVR [PROGRESS]). Furthermore, more aggressive management of comorbidities (e.g., ischaemic heart disease, hypertension, diabetes, or atrial fibrillation), which could also exacerbate the extent of cardiac damage and impair the regression of damage following TAVI, may also be beneficial in this context.
Conflict of interest statement
P. Pibarot received funding from Edwards Lifesciences and Medtronic for echocardiography core laboratory analyses in the field of transcatheter aortic valve replacement with no direct personal compensation. L. Tastet has no conflicts of interest to declare relevant to the contents of this paper.

