Abstract
Aims: Aortic valve surgery in the presence of reduced ejection fraction (EF) or low transaortic gradient is associated with adverse outcome. Low gradient (LG) may be associated with reduced EF, known as low EF-low gradient (LEF-LG), or “paradoxically” low with normal EF (P-LG). Our aim was to investigate the impact of EF and transaortic gradient on outcome following transcatheter aortic valve implantation (TAVI).
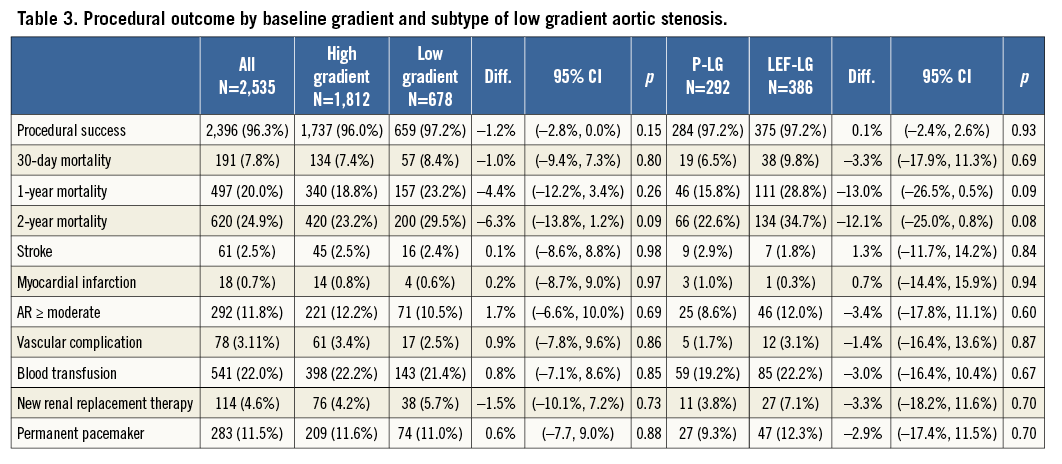
Methods and results: We retrospectively analysed the UK TAVI Registry from 2007 to 2011 (n=2,535 consecutive patients, mean age 81.3±7.5, logistic EuroSCORE 21.8±14). Thirty-day mortality was 7.8%, low EF (<50%) was present in 39%, low gradient (<64 mmHg) was present in 27%, LEF-LG in 15% and P-LG in 12% of patients, respectively. LEF-LG patients had the highest risk profile vs. the other groups (EuroSCORE 30±16 vs. 20±12, p<0.001). Neither EF nor gradient impacted on procedural outcome or 30-day mortality. Mortality at two years was significantly higher in LEF-LG patients (34.7%), whereas, in patients with low EF/high gradient (27.8%) or normal EF/low gradient (23%), mortality was not significantly different from that of normal EF/high gradient (23%) patients. LEF-LG independently predicted reduced survival, HR 1.7 (1.4-2.1).
Conclusions: Neither low EF nor low gradient affected procedural success or 30-day mortality. Long-term survival was reduced in LEF-LG patients but not in those with low EF and high gradient or P-LG with normal EF.
Abbreviations
AR: aortic regurgitation
AVOA: aortic valve orifice area
EF: ejection fraction
LEF-LG: low ejection fraction-low gradient
LG: low gradient
P-LG: paradoxical low gradient (in the presence of normal ejection fraction)
SAVR: surgical aortic valve replacement
TAVI: transcatheter aortic valve implantation
Introduction
Symptomatic aortic stenosis may justify treatment with surgical aortic valve replacement (SAVR) or transcatheter aortic valve implantation (TAVI)1,2. Severe aortic stenosis is defined as a transvalvular velocity >4 m/s (equating to a peak pressure drop of 64 mmHg) and an aortic valve orifice area (AVOA) of <1 cm2 (or valve index <0.6 cm2/m2)3,4.
Discordant echocardiographic measures, where the AVOA is <1 cm2 but the peak velocity is <4 m/s, may be seen in the context of reduced left ventricular ejection fraction (EF), known as low EF-low gradient (LEF-LG) aortic stenosis. A further subset of patients have AVOA <1 cm2, peak velocity <4 m/s but with normal ejection fraction and low transaortic gradients. This phenomenon has been termed “paradoxical” low flow-low gradient aortic stenosis (P-LG), and is often due to a reduced stroke volume (<35 ml/m2)5,6.
Incorrect evaluation of patients with low gradient aortic stenosis may lead either to failure to offer effective treatment, or to inappropriate treatment that may be harmful. Transvalvar velocities are dependent on cardiac contractility, stroke volume and peripheral vascular resistance, factors that are not incorporated into standard evaluation7. Several authors have demonstrated inherent inconsistencies within the diagnostic echocardiographic criteria that may lead to discrepant data4,8. There is historical evidence of patients with low gradient aortic stenosis deemed non-severe who, on re-evaluation with adjustment for variations of transaortic flow, have a high prevalence of truly severe aortic stenosis5,7-10.
The outcome of SAVR in patients with symptomatic severe aortic stenosis is generally better than the outcome with medical therapy. Operable patients with severe aortic stenosis in the context of reduced EF11,12, LEF-LG13-16, and P-LG with or without low stroke volume5,17 all derive benefit from SAVR. However, surgery in these higher risk groups is associated with a higher morbidity and mortality than in patients with normal EF and normal transaortic gradients.
TAVI may be offered to patients who are deemed inoperable or high risk for conventional aortic valve surgery1,2,18. The impact of TAVI on outcome in patients with low gradient aortic stenosis has been less well described than following SAVR, although preliminary data suggest favourable outcomes19-21. The increasing use of TAVI for high-risk patients therefore justifies further evaluation of selection and outcome. We used the UK TAVI database to explore these factors. The specific aims were to determine the early and intermediate outcome of TAVI in patients with depressed ejection fraction, to report the prevalence and impact of low gradient aortic stenosis (LEF-LG and P-LG) on early and intermediate outcome and, finally, to explore the interrelationship of ejection fraction, AVOA, and valve gradient on survival after TAVI.
Methods
UK TAVI REGISTRY
All TAVI procedures in the UK are prospectively recorded in the UK TAVI Registry, as previously described22. Patient selection for TAVI was at the discretion of the Heart Team in each centre but conformed to a standard process with clinical evaluation, angiography and echocardiography performed in all patients prior to decision on treatment made by a multidisciplinary Heart Team.
Standard definitions were used for baseline clinical parameters and these data were uploaded to the central cardiac audit database. Procedural outcome and complications were self-reported according to the definitions outlined in the national data set and published previously22.
All-cause mortality was tracked by linkage, using each patient’s NHS number, with the Office of National Statistics. All deaths in England and Wales are registered with this national body and consequently mortality data are highly robust. The recorded cause of death was not available.
UK centres have adopted transfemoral as the default access, with other access routes (transapical, trans-subclavian and transaortic) used according to local expertise and valve device. The following technologies were available: Medtronic CoreValve (Medtronic, Minneapolis, MN, USA) from 2007, Edwards SAPIEN valve (Edwards Lifesciences, Irvine, CA, USA) (transfemoral 2007, transapical from 2008).
CLASSIFICATION OF AORTIC STENOSIS
The echocardiographic evaluation of the aortic valve recorded in the UK TAVI database is limited to aortic valve orifice area (AVOA) derived from the continuity equation, and peak pressure gradient (PPG) derived from the modified Bernoulli equation; these data were self-reported by the treating centres. Body mass index and gender were recorded, and aortic valve index was calculated according to the Mosteller formula. Left ventricular function was defined as normal (EF >50%), moderately impaired (EF 30-49%), or severely impaired (EF <30%).
Patients in whom the dominant valve pathology was aortic regurgitation were excluded from these analyses. Patients with aortic valve orifice area >1 cm and peak pressure gradient <64 mmHg in the presence of normal ejection fraction were excluded since these subjects did not fulfil accepted criteria for severe aortic stenosis3,4. Patients receiving “valve in valve” TAVI for stenotic surgical prosthesis were not excluded.
Low gradient aortic stenosis was defined as AVOA <1.0 cm2 with a peak pressure gradient <64 mmHg (equivalent to peak velocity <4 m/s). LEF-LG was defined as peak pressure <64 mmHg with EF <50%. P-LG aortic stenosis was defined as peak pressure drop <64 mmHg with normal ejection fraction (>50%).
Stroke volume (by measurement of pulsed wave Doppler in the left ventricular outflow tract) is not reported.
STATISTICAL ANALYSIS
The impact of ejection fraction on survival was examined in binary fashion (normal vs. impaired, and severely impaired vs. others). The impact of gradient on survival was examined in binary fashion (low gradient <64 mmHg vs. high gradient >64 mmHg). Categorical variables were analysed with a two-sample test of equality of proportions using Koopman’s method. Continuous variables were assessed for normality using the Kolmogorov-Smirnov test and informally using quantile-quantile plots. Normally distributed variables were compared using unpaired t-tests, as were skewed variables after transformation. To control for multiple confounders, a Cox regression model was developed. Potential confounders were selected according to clinical importance using components of the logistic EuroSCORE (LES) model, namely age, gender, chronic lung disease, peripheral vascular disease, prior myocardial infarction, stroke, critical status, previous cardiac surgery, vascular access for TAVI, successful valve implantation, and severity of AR (by echocardiography) post procedure. It was not possible to use the LES variable itself because ejection fraction, which is one of its components, was used as a covariate in the regression models. The treating hospital was used as a fixed effect in the regression models to account for clustering within hospitals. To account for missing data, multiple imputation by chained equations was performed, using 20 completed data sets. Survival plots are presented as unadjusted actuarial survival.
Results
A total of 2,490 implants were recorded in 2,591 procedures. Sixteen cases were repeat procedures in patients who had previously had TAVI or attempted TAVI. In 36 patients aortic regurgitation was the dominant pathology and aortic valve area was >1.5 cm2. In 19 patients the echocardiographic criteria submitted did not conform to accepted values of severe aortic stenosis (PPG was <64 mmHg, AVOA was <1 cm2 and EF normal), and these patients were excluded from the analyses. This left a study sample of 2,456 implants in 2,535 procedures.
Completeness of data was as follows: 99% demographics, 96.5% risk factors, and 94% procedural variables. Logistic EuroSCORE and serum creatinine were skewed variables and were log transformed. Mortality tracking was achieved in 100%. Median follow-up was 492 days (range 0-1,981). A total of 741 patients lived beyond two years of follow-up; 630 patients died within two years.
PATIENT CHARACTERISTICS
Baseline data are presented on the basis of valve gradient and subsets of low gradient AS (P-LG vs. LEF-LG) (Table 1). The mean age was 81.3±7.5; logistic EuroSCORE was 21.8±14. Overall procedural success was achieved in 96.8% of patients; unadjusted 30-day mortality was 7.8%. Left ventricular impairment was present in 39.6% and was severe in 9.2% of cases. The prevalence of low gradient severe aortic stenosis was 27.8%; LEF-LG was present in 15% and P-LG in 12% of cases. Low gradient patients were younger, taller and heavier than normal gradient patients, and were more likely to have reduced ejection fraction. Low gradient patients were significantly more likely to be male, to have a higher logistic EuroSCORE, to have pre-existing diabetes, and to be clinically unstable at the time of valve implantation.
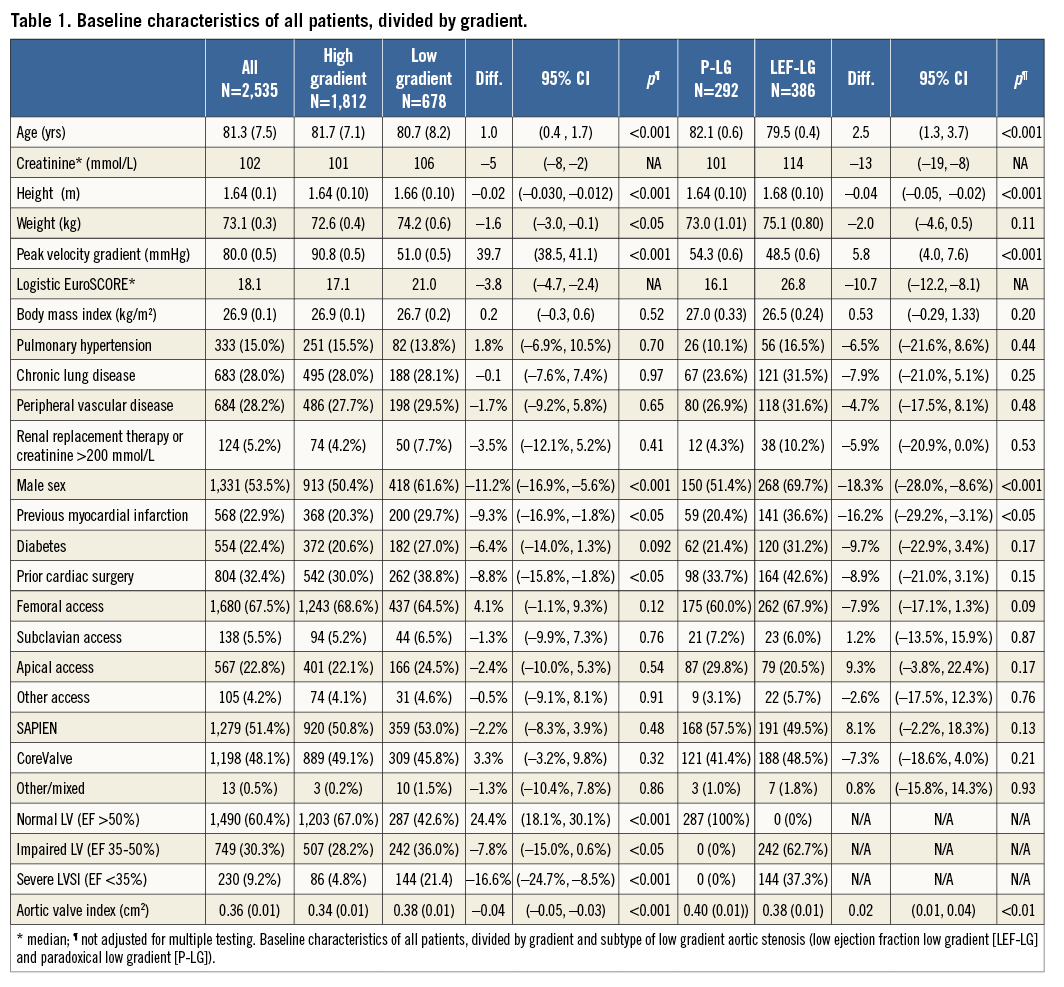
Reduced ejection fraction was associated with male sex (47% male vs. 31% female), diabetes (27% vs. 19%), previous myocardial infarction (34% vs. 16%), and prior cardiac surgery (39% vs. 28%), all p<0.05. The differences observed with gender and ejection fraction meant that P-LG patients were significantly more likely to be female. The AVA/valve index was greater in low-flow patients, and this effect was driven primarily by the P-LG cohort.
OUTCOMES
LEFT VENTRICULAR IMPAIRMENT
Procedural outcome and complication were unaffected by the presence of reduced ejection fraction (Table 2). Unadjusted 30-day mortality was not significantly affected by the presence of reduced EF (6.4% mortality for normal EF, 10% for moderately impaired EF, and 9% for severely impaired EF; p=0.39). Late mortality was increased in patients with reduced EF (one-year 25% vs. 17%, p<0.05, two-year 30% vs. 22%, p<0.05). There was no difference between one-year and two-year mortality rates in patients with moderately impaired EF or severely impaired EF. After adjustment, ejection fraction impacted significantly on survival at final follow-up (median 492 days; range 0-1,981), the hazard ratio (HR) for any reduction in ejection fraction being 1.41 (1.2-1.7) and for severe reduction in ejection fraction being 1.6 (1.3-2.1). However, the adverse effect of LV dysfunction was limited to patients with both low EF and low gradient (HR 1.7 [1.4-2.1]). The presence of low EF with high transaortic gradient (LEF-HG) suggested an intermediate adverse effect that did not meet statistical significance (HR 1.08 [0.67-1.79]) (Figure 1).
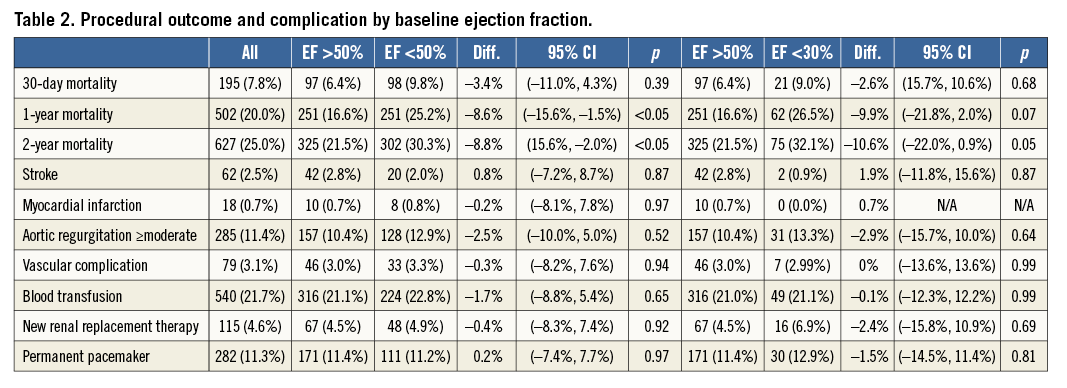
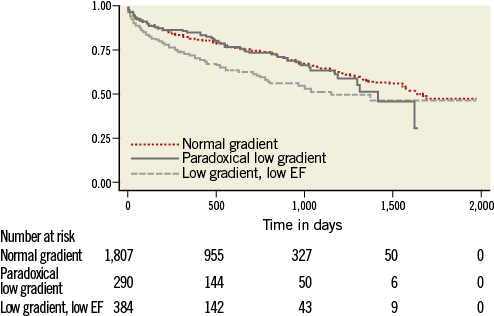
Figure 1. Survival curve by baseline gradient (high gradient vs. low ejection fraction-low gradient [LEF-LG] vs. paradoxical low gradient [P-LG]).
LOW AND HIGH GRADIENT AS
Low gradient aortic stenosis was present in 27.3% of cases. Procedural success, rate of complication and unadjusted survival were unaffected by low gradient (Table 3). After adjustment, survival at final follow-up was worse for low gradient aortic stenosis (HR 1.3 [1.11-1.57]).
SUBTYPES OF LOW GRADIENT AS
The prevalence of LEF-LG was 15% and of P-LG was 12%. Both the unadjusted and adjusted survival rates of patients with LEF-LG were worse than of patients with high-flow aortic stenosis (34.7% vs. 23.2% at two years). In contrast, the outcomes for P-LG patients matched those of high-flow patients both before and after adjustment (Figure 2).
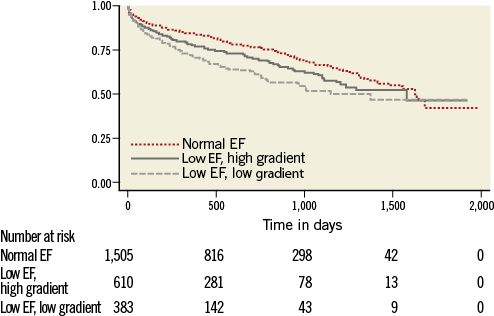
Figure 2. Survival curve by EF and gradient (normal EF vs. low ejection fraction-low gradient [LEF-LG] vs. low ejection fraction-high gradient [LEF-HG]).
Discussion
The findings of this study indicate that both impairment of left ventricular function and low gradient aortic stenosis are common in patients undergoing TAVI, affecting 39.6% and 27% of patients in the UK TAVI Registry, respectively. The interaction of ejection fraction and transaortic gradient has a complex relationship with outcome and risk.
EFFECT OF EJECTION FRACTION
Left ventricular dysfunction by any measure or severity of ejection fraction had no significant effect on procedural success and short-term outcome. Beyond the procedure, low EF is associated with significant attrition. In our study, low EF with high gradient was associated with a more favourable outcome, and this may reflect preservation of cardiac reserve and better EF recovery following TAVI, an effect that has been reported previously23. Real-world data from Canada24, France25 and now the UK have failed to show an adverse impact of left ventricular dysfunction on procedural success or short-term outcome. Only the German TAVI registry has found increased procedural risk with reduced ejection fraction, an effect possibly driven by a different definition of normal EF (>40%)26. The hypothesis generated by these data is that the safety of the TAVI procedure is not influenced by the presence of underlying left ventricular dysfunction. This is in contrast to the literature on surgical aortic valve replacement, where low EF patients are exposed to higher earlier mortality than patients with normal EF. One question is whether TAVI should be a default strategy in patients with reduced EF and/or reduced transaortic gradients. The theoretical benefits of TAVI in high-risk patients with reduced EF include the avoidance of cardiopulmonary bypass and prolonged ventilation, minimisation of patient-prosthesis mismatch, and more rapid recovery of ventricular function than is associated with aortic valve surgery19,21,23,27-29. Comparison of outcome between non-randomised samples of patients treated by surgery and TAVI is challenging due to substantial variation in baseline characteristics. The 30-day mortality of patients with low EF in the UK TAVI population is 9.8%: this compares well to the published surgical outcomes ranging between 9 and 18%16,30,31. The one-year mortality of patients with reduced EF receiving TAVI in the UK is 25%, for LEF-LG 28.8% and P-LG 16%. The equivalent outcomes at one year of patients treated by SAVR for reduced EF range between 15 and 22%16,30-32. The Euro Heart Survey confirmed that a significant proportion of patients with important aortic valve disease were either never considered for SAVR, or were felt to be inoperable due to age, reduced EF and frailty33. Furthermore, the surgical outcomes in the trials cited above are based on patients who were on average 10-15 years younger than the patients in the UK TAVI database and with substantially lower baseline logistic EuroSCORE. Therefore, the current evidence base suggests that procedural safety may favour TAVI over surgery in some patients with reduced EF.
EFFECT OF GRADIENT ON OUTCOMES
Low gradient aortic stenosis was present in 27% of patients, a level consistent with previous reports5,8,30. The presence of low gradient did not affect procedural outcomes. The low gradient group was itself split with about half (15% overall) LEF-LG and the rest (12% overall) P-LG aortic stenosis.
As in other studies, the P-LG patients were older and more often female34, and in this series more likely to be treated with non-femoral access. Despite these more adverse baseline characteristics, the P-LG patients had outcomes no worse than normal EF and high gradient patients following TAVI.
GRADIENT AND FLOW
The present study has no data on transaortic flow (measured by pulsed wave Doppler in the left ventricular outflow tract): therefore, we are unable to define low-flow physiology. Recently, retrospective analyses of the PARTNER data by Herrmann et al and of the Canadian registry by Le Ven et al have highlighted the importance of low transaortic flow, defined as a stroke volume <35 mL/m2, in determining outcome following SAVR and TAVI35,36. Low-flow and low gradient are not the same, but are often associated. The prevalence of low-flow was similar in these papers (55% & 52.3%, respectively), as was the proportion of patients with low-flow with reduced ejection fraction LEF-LG (12% & 15%, respectively).
We can speculate that many of the UK TAVI Registry patients defined as P-LG also had low-flow. Consistent with this assertion is the fact that the proportion of patients in the UK TAVI Registry with P-LG is similar to that of PLF-LG (with normal EF) reported in PARTNER and the Canadian registry (12% in UK TAVI vs. 14% & 9%, respectively) and of LEF-LG (15% in UK TAVI vs. 12% & 15%, respectively).
The impact of aortic stenosis in the context of P-LG or PLF-LG (with normal EF) appears important. A single study on initially asymptomatic patients reported a one-year mortality <5% with an annualised SAVR rate of 13.8%34, but three other studies suggest a less benign natural history of PLF-LG aortic stenosis, with a one-year mortality in the absence of SAVR greater than 15%5,17,30. Subgroup analysis of the PARTNER data suggested a superior survival of PLF-LG patients treated by SAVR or TAVI compared to medical management.
Despite the difficulties of comparing trials, it is clear that aortic stenosis with PLF physiology or P-LG is associated with significant harm in the presence of symptoms, and that these patients are offered SAVR less often17,30. TAVI in these patients seems to perform well: in our study these patients had outcomes matching those of patients with high gradients, while in PARTNER the patients had survival superior to those treated with medical therapy.
The LEF-LG patients have significant attrition beyond the initial procedure, and this finding is consistent with all recent studies. This increase in all-cause mortality is presumably driven by the presence of irreversibly reduced ejection fraction. The combination of reduced EF and low gradient was associated with the worst outcome, survival at one year being 71% and at two years being 65%. Despite this attrition, the 65% two-year survival rate is comparable to surgical outcomes which vary between a 55-80% two-year survival rate following surgery, and <25% survival rate with conservative management12,13,15.
Although ejection fraction appears to dominate long-term outcome, we found evidence that patients with a high gradient in the presence of reduced EF had good outcomes. This presumably reflects adequate cardiac reserve that can be reversed by successful valve intervention.
The present data show acceptable outcomes for TAVI in patients with low EF, low gradient, or both. The combination of low gradient and low EF identified a high-risk population. The phenomena of paradoxical low gradient with normal ejection fraction or high gradient in the presence of reduced ejection fraction did not significantly impact on survival following TAVI, although the survival for LEF-HG was intermediate between normal EF and LEF-LG when plotted with actuarial curves. The 30-day mortality for patients with low gradient, low EF, or both compares well to published outcomes for surgery and, although attrition beyond the TAVI procedure is considerable, the survival is comparable to that of SAVR in published series.
Study limitations
The limitations of the UK TAVI data set have already been partially described in the text. Outcomes are based on all-cause mortality with no discrimination between cardiac and non-cardiac death. The absence of measures of stroke volume, left ventricular dimensions and aortic valve impedance prevent categorisation of low-flow physiology. Furthermore, data from important investigations performed by the treating centres such as stress echo, transoesophageal imaging, cross-sectional imaging and invasive evaluation were not available for analysis. Finally, there is a lack of a control group, such as a group with moderate aortic stenosis or severe aortic stenosis treated conservatively or with SAVR.
Conclusions
Low gradient and low EF were commonly seen in the UK TAVI Registry population. In contrast to the existing literature on SAVR, procedural outcome and 30-day mortality were not significantly affected by reduced EF or low gradient.
Late mortality was increased with the combination of low EF and low gradient, but not in those patients with low EF and high gradient, or in those with paradoxical low gradient AS with normal EF.
| Impact on daily practice Management of aortic stenosis with reduced ejection fraction (EF) or low transaortic gradient can be challenging. Surgical valve replacement is associated with increased morbidity and mortality. In the UK TAVI Registry, the prevalence of reduced EF was 39.6% and low gradient 27.3%. Low gradient was associated with reduced EF in 15% and was paradoxically low with normal EF in 12%. Short-term outcome after TAVI was unaffected by reduced EF or low gradient. Patients with normal EF had the best long-term outcome, even if the transaortic gradient was low. Paradoxical low gradient was associated with smaller, female patients and may be associated with reduced stroke volume. Patients with reduced EF had the worst long-term mortality although a subset of patients with low EF and high transaortic gradient had good outcome. Heart Teams should be reassured that the procedural success of TAVI is unaffected by low gradient or reduced EF. |
Conflict of interest statement
C. Malkin is a consultant for Boston Scientific. M. Thomas is a consultant and proctor for Edwards Lifesciences. N. Moat is a consultant to Medtronic, and has received honoraria from Edwards Lifesciences and Abbott. D. Blackman is a consultant and proctor for Medtronic, and a proctor for Boston Scientific. O. Wendler is a consultant and proctor for Edwards Lifesciences. M. Monaghan is a consultant for Edwards Lifesciences. The other authors have no conflicts of interest to declare.