Abstract
Aims: Approximately 40% of severe aortic stenosis (AS) patients have a low-gradient (<40 mmHg) AS (LG-AS). The aim of this study was to investigate the invasively measured haemodynamic changes and long-term outcome after transcatheter aortic valve replacement (TAVR) in the subgroups of LG-AS.
Methods and results: A total of 600 LG-AS patients with haemodynamic assessment by left and right heart catheterisation were divided into three groups: normal-flow (NFLG-AS; n=296), paradoxical low-flow (PLFLG-AS; n=153), and classic low-flow (CLFLG-AS; n=151). Post TAVR, PLFLG-AS and CLFLG-AS showed a significant reduction in global afterload (p<0.005), as well as a significant elevation of stroke volume index (SVI), and left and right ventricular stroke work index (p<0.001). NFLG-AS was associated with an elevation of global afterload and a decrease of SVI (p<0.05). Overall survival was highest in NFLG-AS, followed by PLFLG-AS and CLFLG-AS. All subgroups experienced similar symptomatic improvement.
Conclusions: NFLG-AS was the most prevalent form of LG severe AS and was associated with adequate left ventricular compensation and good prognosis. On the other hand, CLFLG-AS represents the heart failure with reduced ejection fraction (HFrEF) form of AS and was associated with the worst prognosis, whereas PLFLG-AS represents the heart failure with preserved ejection fraction (HFpEF) form of AS with intermediate prognosis. Both groups showed early haemodynamic reverse response after TAVR.
Introduction
Calcific aortic stenosis (AS) is the most frequent heart valve disease in developed countries1. When patients with severe AS develop symptoms, effective treatment by surgical aortic valve replacement (SAVR) or transcatheter aortic valve replacement (TAVR) is necessary to reduce mortality and improve symptoms. Usually, standard transthoracic echocardiography is an appropriate imaging modality to evaluate disease severity. Thereby, severe AS is defined as aortic valve area (AVA) ≤1.0 cm2 or indexed AVA (AVAi) ≤0.6 cm2/m2, and a mean transvalvular gradient (MG) ≥40 mmHg2. However, in about 40% of AS patients, echocardiographic findings are discordant and multimodality imaging is required. The most common constellation is called “low-gradient AS” (LG-AS) with a small AVA (≤1.0 cm2) and low MG (<40 mmHg) and is associated with uncertainties regarding disease severity and therapeutic management2,3,4,5,6,7,8. According to the current European guidelines, LG-AS should be divided into three subgroups depending on flow pattern and left ventricular ejection fraction (LVEF): classic low-flow, low-gradient AS (CLFLG-AS) with reduced LVEF; paradoxical low-flow, low-gradient AS (PLFLG-AS) with preserved LVEF but reduced stroke volume index (SVI); and normal-flow, low-gradient AS (NFLG-AS) with preserved LVEF and SVI. According to the European guidelines, AVR is recommended in CLFLG-AS and PLFLG-AS (class IIa2). For NFLG-AS there are no specific recommendations. These patients are more likely to have moderate AS, although recent studies have shown that approximately 50% have severe AS8,9. Regarding PLFLG-AS, conflicting results concerning the outcome and benefit of AVR have been published8,10,11. To provide optimal therapy, multimodality imaging before and after AVR is necessary to understand the pathophysiology2,3,4. Although previously published studies provide evidence of echocardiographic improvement after AVR7,12,13,14,15, there are no invasively measured data showing haemodynamic changes after AVR7,16,17. Therefore, the objective of the present study was to evaluate the invasive measurements before and directly after TAVR to gain more insight into the haemodynamic changes and to understand which of the entities benefits most.
Methods
PATIENT POPULATION AND STUDY DESIGN
Six hundred (600) LG-AS patients (invasively measured AVA ≤1.0 cm2 or indexed AVA [AVAi] ≤0.6 cm2/m2; invasively measured MG [MG (invasive)] <40 mmHg) with full invasive haemodynamic assessment before and after TAVR, who were treated between September 2009 and November 2017 in our hospital were included. The patients were divided into three groups according to the guidelines2: NFLG-AS (n=296; LVEF ≥50%, stroke volume index [SVI] >35 ml/cm2); PLFLG-AS (n=153; LVEF ≥50%; SVI ≤35 ml/cm2); CLFLG-AS (n=151; LVEF <50%) (Figure 1). All patients underwent extended echocardiographic examination as well as haemodynamic assessment by left and right heart catheterisation directly before and after the TAVR procedure. A detailed specification of the parameters which were assessed and calculated is provided in Supplementary Appendix 1.
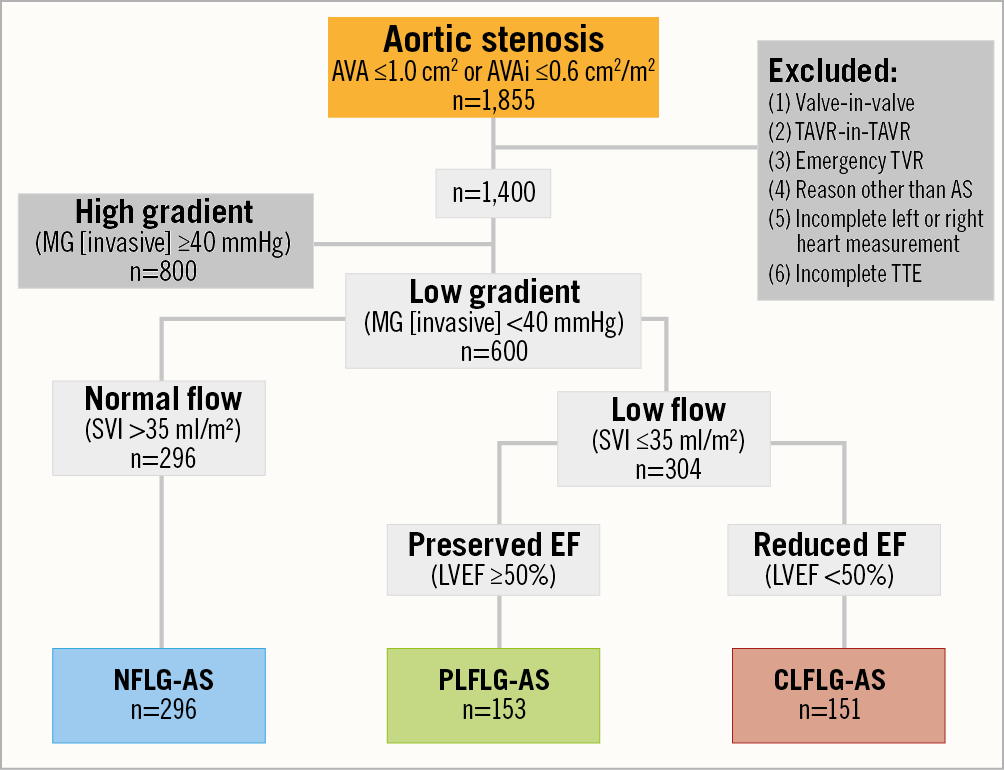
Figure 1. Flow chart of patient population selection. AS: aortic stenosis; AVA: aortic valve area; AVAi: indexed AVA; CLFLG: classic low-flow low-gradient; LVEF: left ventricular ejection fraction; MG (invasive): invasively measured mean transvalvular gradient; NFLG: normal-flow low-gradient; PLFLG: paradoxical low-flow low-gradient; SVI: invasively measured stroke volume index
TRANSCATHETER AORTIC VALVE IMPLANTATION PROCEDURE
A Heart Team consisting of an interventional cardiologist, a cardiac surgeon, and an anaesthesiologist evaluated severe symptomatic AS patients and made the final decision for TAVR procedures. TAVR procedures were performed using standard techniques. According to the device availability at different time points, commercially available valves were implanted via a transfemoral (n=515), transaxillary (n=36), transapical (n=43), or transaortic (n=6) access. Clinical outcomes were assessed according to the Valve Academic Research Consortium (VARC)-2 criteria18. Cause of death and complications after TAVR, as well as New York Heart Association (NYHA) functional class at six-month, one-year and maximum follow-up of 8.5 years were collected.
STATISTICAL ANALYSIS
Continuous variables are described as means and standard deviations or medians and interquartile range (IQR), as appropriate; they were compared by one-way analysis of variance (ANOVA) with post hoc Bonferroni correction for multiple comparisons and t-tests. Categorical data are described with absolute and relative frequencies and compared using Fisher’s exact test. A two-tailed p-value <0.05 was considered statistically significant, except for multiple (n=3) two-group comparisons, for which p<0.0167 was considered statistically significant. Hazard ratios (HR) were calculated in a multivariable analysis, including all variables with a p-value <0.05 in the univariate analysis, and were used to determine independent predictors of one-year mortality after TAVR. A p-value <0.05 was considered statistically significant. Kaplan-Meier analysis was used to estimate the incidence of clinical outcomes at one- and five-year follow-up. Statistical analyses were performed with Statistical Package for Social Sciences, version 20.0.0 (IBM Corp., Armonk, NY, USA).
Results
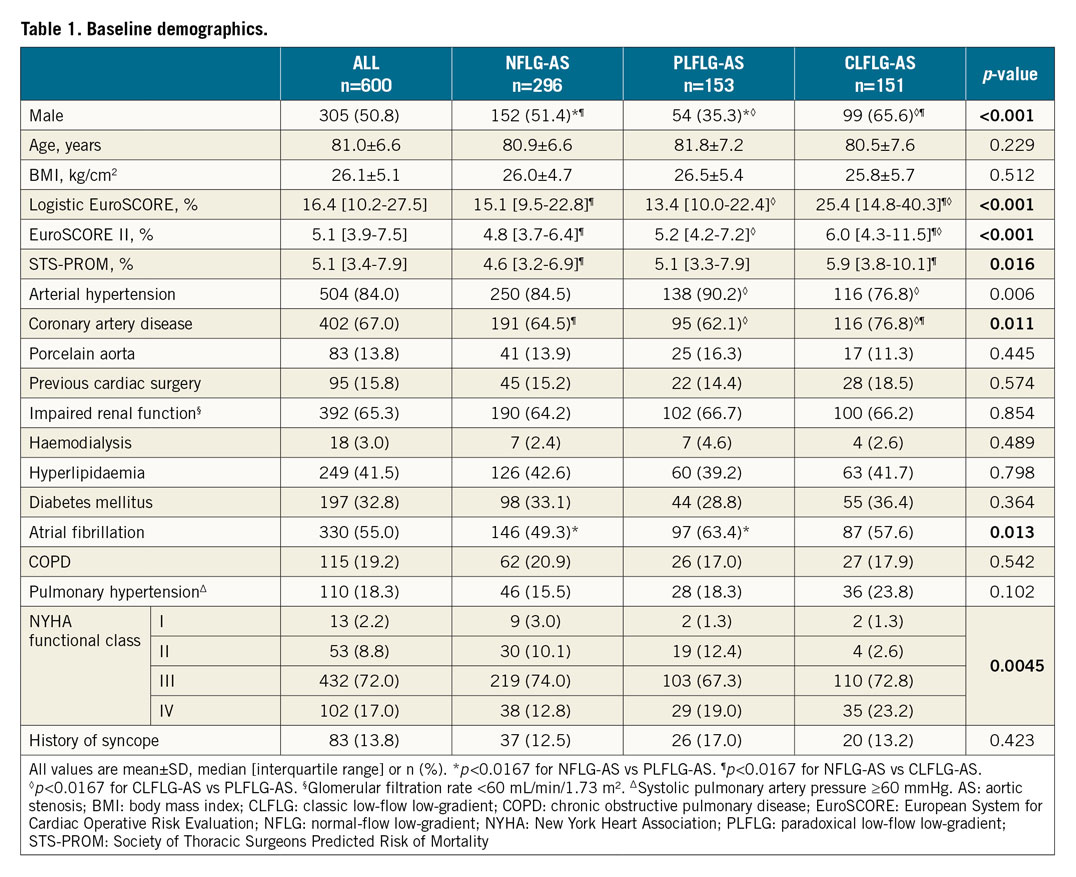
PATIENTS’ CLINICAL CHARACTERISTICS
Mean age was 81.0±6.6 years, and 49.2% of the patients were female. Females were significantly more prevalent (64.7%) among PLFLG-AS than among NFLG-AS (48.6%) or CLFLG-AS (34.4%), whereas males more often had CLFLG-AS. CLFLG-AS, as opposed to PLFLG-AS or NFLG-AS, showed higher operative risk scores, significantly more often had coronary artery disease, and presented more often in NYHA Class ≥III. PLFLG-AS patients markedly more often had atrial fibrillation than NLFLG-AS patients and more often had arterial hypertension than CLFLG-AS patients (Table 1).
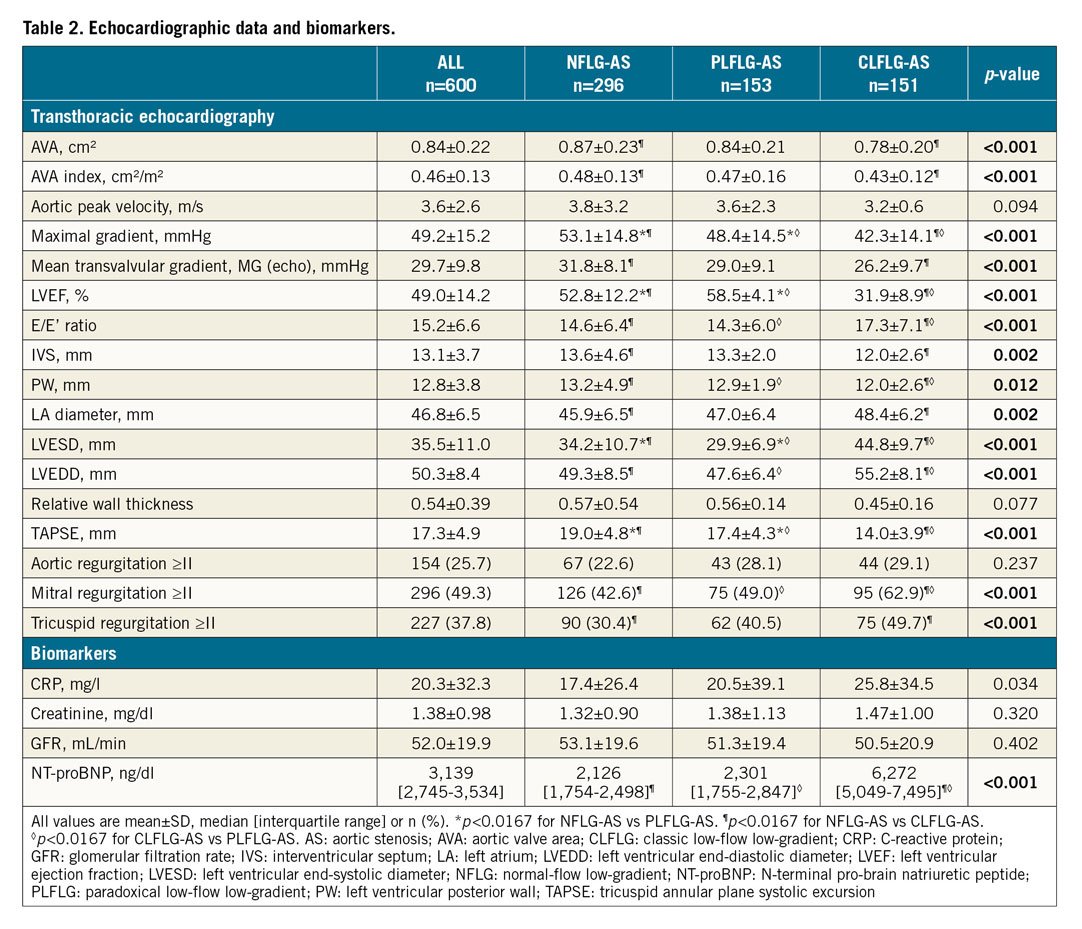
ECHOCARDIOGRAPHIC AND LABORATORY CHARACTERISTICS
CLFLG-AS presented with significantly lower LVEF, tricuspid annular plane systolic excursion (TAPSE), and thinner posterior wall, more dilated LV, and a higher prevalence of mitral regurgitation (MR) compared to both of the other groups. Furthermore, NFLG-AS had significantly greater AVA and higher MG measured by echocardiography (MG [echo]). Moreover, these individuals had a lower prevalence of tricuspid regurgitation (TR) compared to CLFLG-AS, and lower LVEF than PLFLG-AS (Table 2, Supplementary Figure 1, Moving image 1A, Moving image 1B, Moving image 2A, Moving image 2B, Moving image 3A, Moving image 3B). In the laboratory tests, CLFLG-AS presented with markedly higher levels of NT-proBNP, while similar levels were documented in both of the other groups.
ACUTE HAEMODYNAMIC CHANGES POST TAVR
Significant increase in AVA and decreases in MG (invasive) and valvular resistance (VR) were documented in all patients, whereas a significant decrease of systemic vascular resistance index (SVRI) was noted in PLFLG-AS. CLFLG-AS was associated with still elevated SVRI after TAVR. Consequently, PLFLG-AS and CLFLG-AS had a significant decrease of valvuloarterial impedance (Zva), whereas NFLG-AS had a statistically significant, but clinically not relevant increase of Zva (Supplementary Table 1, Figure 2, Supplementary Figure 2, Supplementary Figure 3). Significant elevations in LV end-diastolic (LVEDP) and pulmonary capillary wedge pressures (PCWP) were observed in all patients. While SVI, cardiac output (CO), cardiac index (CI), left ventricular stroke work index (LVSWI), and left cardiac work index (LCWI) were significantly increased in PLFLG-AS and CLFLG-AS, NFLG-AS exhibited a decrease of SVI after TAVR. Increases in pulmonary artery (PAP) and right arterial pressures (RAP) were noticed in all patients. While pulmonary vascular resistance index (PVRI) was normal before TAVR and unchanged in NFLG-AS after TAVR, it was moderately increased in CLFLG-AS before, and decreased significantly after valve deployment. In PLFLG-AS, the slightly elevated pulmonary resistances at baseline did not change after TAVR. Right ventricular function, left ventricular stroke work index (RVSWI) and left cardiac work index (RCWI) were normal at baseline in all patients and improved in PLFLG-AS and CLFLG-AS, but not in NFLG-AS, after TAVR.
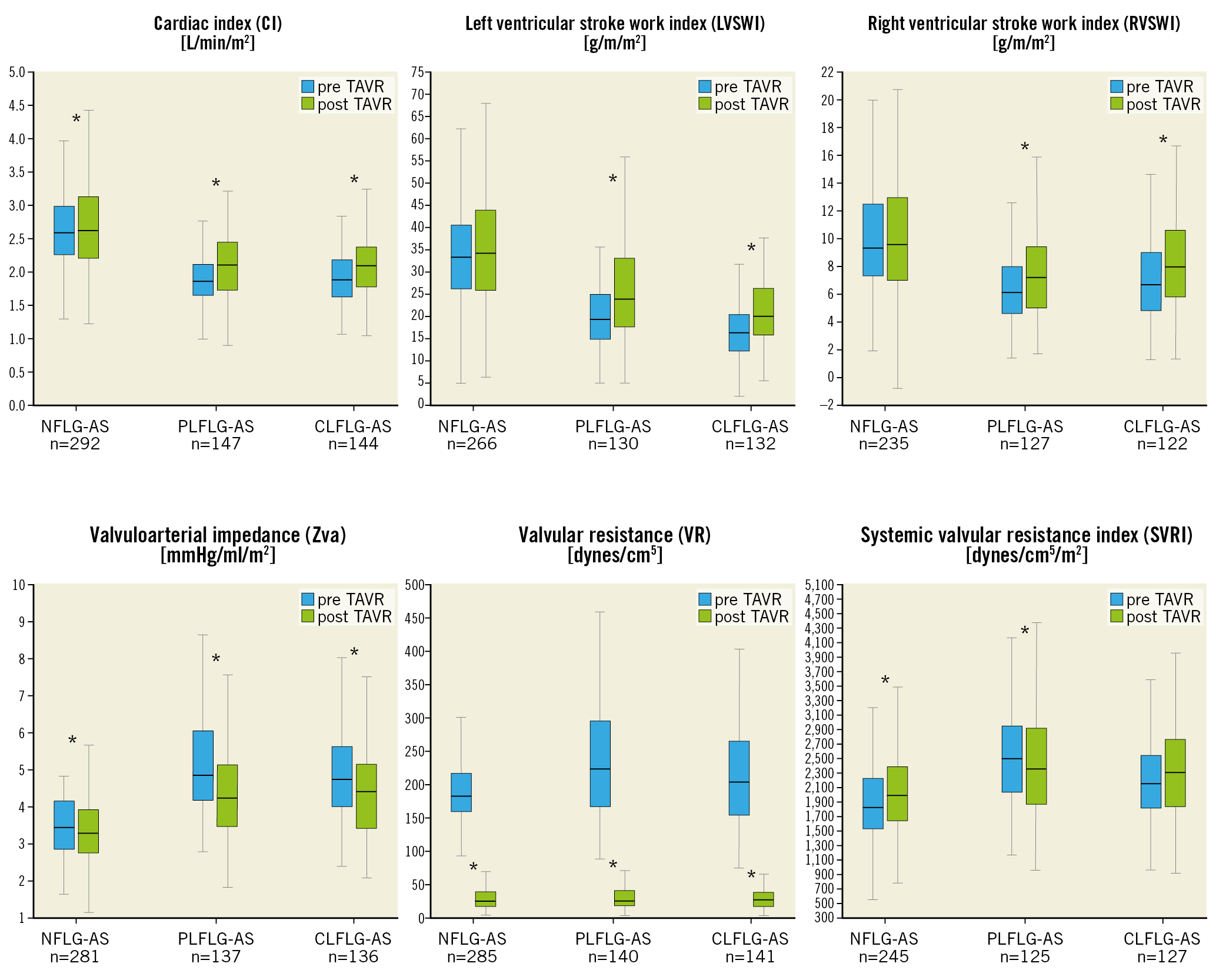
Figure 2. Haemodynamic parameters in the LG-AS subgroups. Box plots of selected haemodynamic parameters pre (blue) and post TAVR (green) according to LG-AS subgroup. *p<0.05 for pre versus post TAVR. LG-AS: low-gradient aortic stenosis
OUTCOMES
Acute device success was 95.8%, with correct positioning of one prosthesis in 99.3% of cases. Eight patients had moderate-to-severe paravalvular regurgitation despite post-dilatation. In four patients, MG (invasive) was ≥20 mmHg after TAVR. Four patients required conversion to open heart surgery, two patients due to ventricular embolisation of the prosthesis, and two patients due to myocardial perforation. Overall in-hospital stroke rate was 5.0%. Life-threatening or disabling bleedings occurred in 38 patients, while overall major bleedings were observed in 14.5% (Supplementary Table 2). Overall survival at one and five years was highest in NFLG-AS (Figure 3A-Figure 3C). Freedom from cardiovascular death at one year was similar in NFLG-AS and PLFLG-AS, and higher in CLFLG-AS (Figure 3B), which gained more expression after five years (Figure 3D). While baseline NYHA class differed significantly among the subgroups, with the most common occurrence of NYHA Class ≥III being in CLFLG-AS (p=0.006), the functional class after TAVR was not significantly different among the three subgroups at six (p=0.354) and 12 months (p=0.212) (Figure 4).
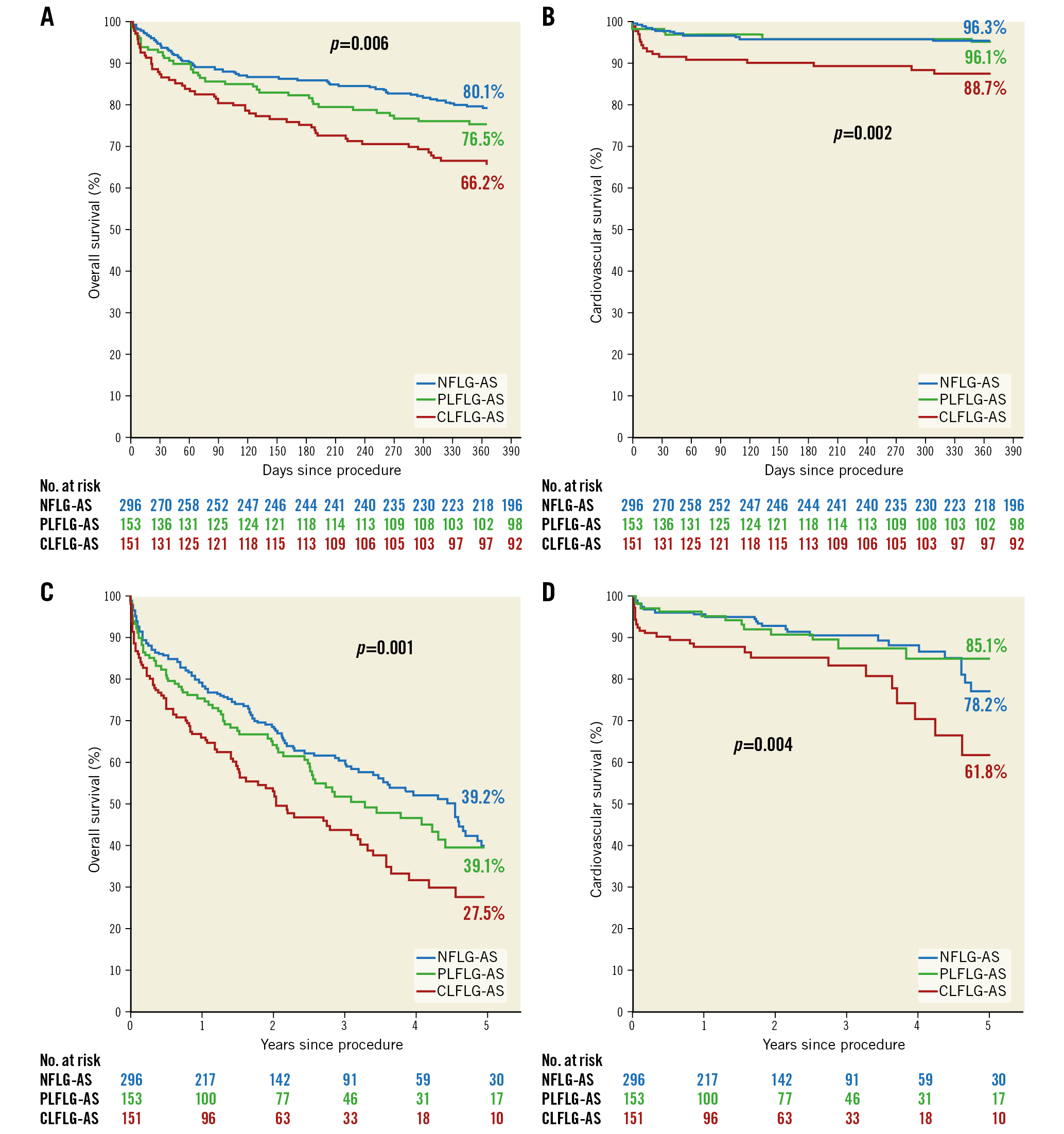
Figure 3. Kaplan-Meier curves for all-cause (A & C) and cardiovascular (B & D) survival at one year and five years according to LG-AS subgroup. LG-AS: low-gradient aortic stenosis
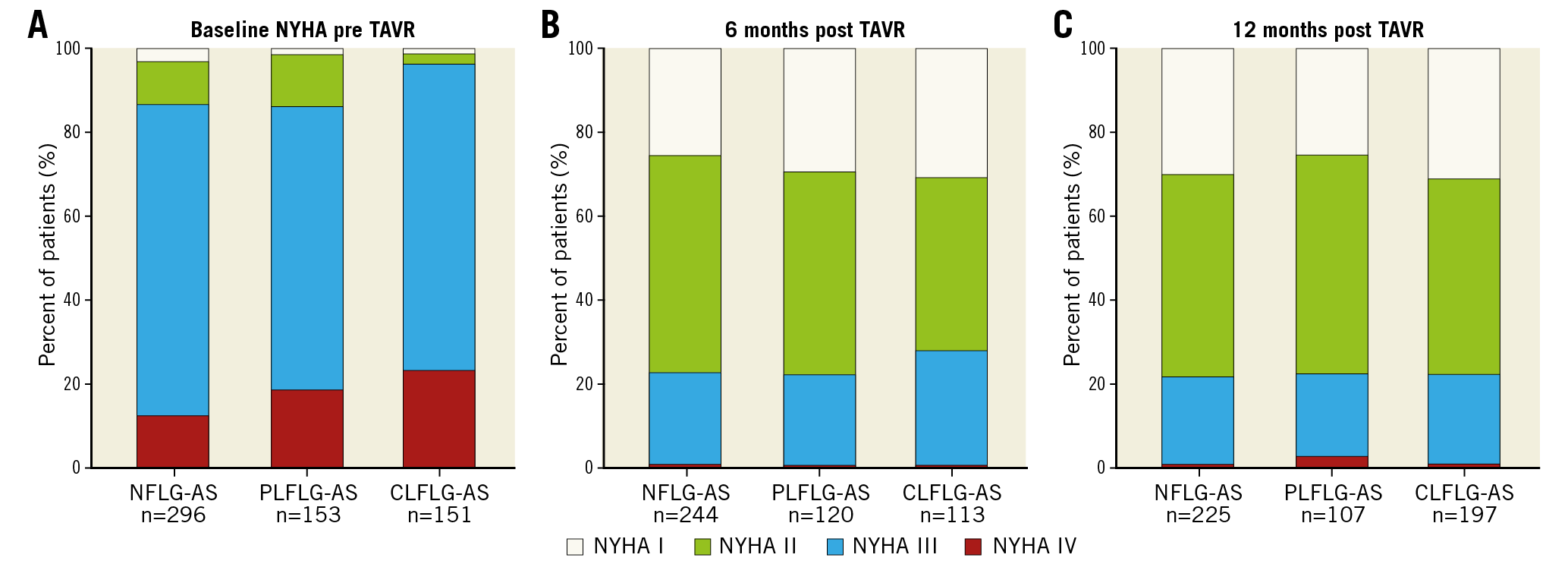
Figure 4. New York Heart Association (NYHA) functional class. A) Baseline. B) Six months. C) 12 months. LG-AS: low-gradient aortic stenosis
PREDICTORS OF ONE-YEAR MORTALITY
In a multivariable analysis of NFLG-AS, age (hazard ratio [HR] 1.09, 95% confidence interval [CI]: 1.05-1.14) and pulmonary hypertension (HR 2.92, 95% CI: 1.65-5.14) were shown to be independent predictors for one-year mortality. In PLFLG-AS, only age (HR 1.06, 95% CI: 1.00-1.12) was predictive for death. In CLFLG-AS, age and atrial fibrillation were significant predictors in the univariate analysis but not in the multivariable analysis (Supplementary Table 3).
Discussion
This is the first retrospective study analysing early invasively measured haemodynamic changes and long-term outcomes in different subgroups of LG-AS patients undergoing TAVR. The main findings can be summarised as follows:
1. PLFLG-AS is typically accompanied by increased global afterload due to increased systemic and valvular resistances, and by haemodynamically measured impaired systolic LV function despite a preserved LVEF.
2. CLFLG-AS patients have the most impaired haemodynamics, with significantly decreased LV function and increased systemic and pulmonary resistances.
3. NFLG-AS is associated with almost regular haemodynamic parameters and showed less clinically relevant changes after TAVR.
4. In PLFLG-AS and CLFLG-AS, TAVR leads to haemodynamic improvement directly at the end of the procedure.
5. Overall survival at one and five years was highest in NFLG-AS, followed by PLFLG-AS and lowest in CLFLG-AS.
The pathophysiology of the different LG-AS entities is very complex. This challenging topic has been brought into focus regarding the diagnostic uncertainties and treatment strategy, due to the fact that over 40% of all patients with severe AS have a low-gradient status2,3,4,5,6,7,8. Multimodality imaging and haemodynamic assessment are necessary to obtain more insight into the pathophysiology in order to facilitate decision making – observation versus conservative treatment versus AVR4,5,6,8.
NORMAL-FLOW, LOW-GRADIENT AORTIC STENOSIS
NFLG-AS represents the largest entity of LG-AS (approximately 50%)4, but less is known about the pathomechanism. This entity was first described by Hachicha et al in 20072,19. Currently, the guidelines advise a re-evaluation of the measurements, and declare that moderate AS is more likely in this patient group. Finally, there is no recommendation on specific therapeutic management2. Nevertheless, conflicting data were published by Minners et al who described a discrepancy between the cut-off values and suggested that an AVA ≤1.0 cm2 might more likely correspond to an MG of 30-35 mmHg rather than 40 mmHg20. However, other authors suggest that approximately 50% of cases have severe AS, and that symptomatic patients benefit from AVR8,9. The HAVEC group categorised this entity as “stage D4” and recommended performing multislice computed tomography with aortic valve calcium scoring to verify the severity stage3. In our study, only symptomatic high-risk patients with significantly elevated levels of both NT-proBNP and calcium score, in the absence of other reasons for symptoms, were considered for TAVR. Compared to regular RV and LV function at the baseline echocardiography, in the invasive haemodynamic tests only slightly decreased LV function (LVSWI) with elevated PCWP was assessed. These findings suggest that a symptomatic NFLG state represents less advanced but already ongoing cardiac damage (stage 1-2 according to Généreux et al21). Carter-Storch et al analysed echocardiographic findings in NFLG-AS (n=33) and suggested that this entity probably has less severe AS with less reverse remodelling after AVR but benefits via a reduction of symptoms14. The smaller haemodynamic improvement in the present subgroup of NFLG-AS supports this suggestion. Furthermore, multiple studies have shown that NFLG-AS benefits from AVR more compared to conservative treatment5,8,22. In our patients, overall one- and five-year mortality was lower in NFLG-AS compared to the other two groups. Thus, these findings support the fact that NFLG-AS has the best prognosis compared to the other two subgroups, as previously described5,8.
PARADOXICAL LOW-FLOW, LOW-GRADIENT AORTIC STENOSIS
PLFLG-AS was first described in 2007 by Hachicha et al and is observed in 5-15% of severe AS patients19. It was suggested that, in contrast to CLFLG-AS, PLFLG-AS patients can be referred to as having “heart failure with preserved ejection fraction” (HFpEF)4. Typically, these patients are more often female, with arterial hypertension, atrial fibrillation, and a small LV cavity due to established concentric remodelling, with restrictive functionality and pronounced LV diastolic dysfunction. These factors, as well as significant MR or TR, lead to a low-flow status, despite a preserved LVEF6,19,23,24,25. Partially, this constellation was able to be proved in the present analysis. Both echocardiographic (E/E’) and invasive measurements (LVEDP) documented a diastolic function similar to NFLG-AS. However, the haemodynamic assessments provided evidence of more advanced impairment of LV function. Moreover, while RV function was still preserved, propagation of LV impairment was reflected in increased pulmonary resistances and pressures, resulting in more elevated RAP. As was suspected previously by measurements of global longitudinal strain, these findings emphasise that LVEF quantification by echocardiography overestimates LV function in these patients, which actually seems to be in a more advanced stage of cardiac damage (stage 2-3)15,21. Furthermore, it was observed that impaired longitudinal LV function has been found to improve after AVR as a sign of reverse remodelling15,24, which is supported by our haemodynamic results with improvement of LV and RV function, and global afterload.
Our results support the findings of previous studies which showed a very similar survival in PLFLG-AS and CLFLG-AS patients, and a significantly better outcome in NFLG-AS patients26. Regardless of the mechanism of reduced flow, these patients are at an advanced stage of the disease and benefit from TAVR.
CLASSIC LOW-FLOW, LOW-GRADIENT AORTIC STENOSIS
This entity can be found in 5-15% of severe AS26 and is associated with male individuals, ischaemic cardiomyopathy and increased operative risk5. It is well documented that CLFLG-AS patients have the worst outcome, regardless of treatment by SAVR or TAVR. These patients have larger LV dimensions, impaired LV and RV function, and a higher prevalence of significant MR5. Accordingly, invasive haemodynamic assessments revealed severely decreased LV systolic and diastolic function. As a consequence of the severely advanced cardiac damage, pulmonary haemodynamics (resistance and pressures) and RV function are impaired most compared to the other two entities. These patients represent the heart failure with reduced ejection fraction (HFrEF) form of AS. Happily, our invasive measurements support previous echocardiographic studies which demonstrated reverse remodelling with improvement in LV and RV function after AVR, especially in CLFLG-AS patients12,13,14.
Limitations
The limiting aspects of the present investigation are as follows. This was a retrospective analysis, although the data were collected prospectively. Due to the fact that haemodynamic measurements were performed directly prior to TAVR, there could be some discordant findings in measurements depending on sedation and volume status. Although computed tomography including measurements of the extent of aortic valve calcification were performed, these data have not been analysed in detail. No stress echo data routinely exist for CLFLG-AS. In elderly patients with a low-flow state, invasive measurement of AVA could underestimate AVA compared to echocardiography27.
Conclusions
Severe symptomatic low-gradient AS is almost as prevalent as high-gradient AS (approximately 40%), but less is known about the outcome and early changes of haemodynamics after TAVR in these patients. In the present study, we were able to show that NFLG-AS was the most prevalent form of LG severe AS and was associated with adequate left ventricular compensation, less improvement of haemodynamics after TAVR and best survival compared to the other two entities. These patients seem to be at the early stage of severe AS disease, becoming either PLFLG-AS or CLFLG-AS if the disease progresses. While CLFLG-AS represents the HFrEF form of AS, which gives the impression of “end-stage” cardiac damage with poor prognosis, PLFLG-AS represents the HFpEF form of AS and correspondingly showed depressed systolic function in the haemodynamic assessment despite a preserved LVEF with intermediate prognosis. Both groups showed a significant improvement in haemodynamics after TAVR compared to NFLG-AS. Further analyses are needed to assess changes in haemodynamics and their impact on long-term mortality after TAVR.
|
Impact on daily practice Multimodality imaging and haemodynamic assessment are the key points for understanding the stage of severity of low-gradient aortic stenosis. By an invasive work-up, we were able to demonstrate different pathways and outcomes of AS entities: CLFLG-AS represents the HFrEF form of AS and was associated with the worst prognosis, whereas PLFLG-AS represents the HFpEF form of AS with intermediate prognosis. Both groups showed early haemodynamic improvement after TAVR. On the other hand, NFLG-AS was the most prevalent form of severe LG-AS and was associated with adequate left ventricular compensation, less haemodynamic improvement and good prognosis after TAVR. Additional large multicentre studies are needed to assess the optimal imaging work-up and the optimal therapy strategy for LG-AS subgroups. |
Conflict of interest statement
C. Frerker has been working as a proctor for St. Jude Medical, Medtronic, and Boston Scientific and has received lecture honoraria from Edwards Lifesciences. T. Schmidt has received lecture honoraria from Medtronic. K-H. Kuck reports having received consulting fees/honoraria from Biosense Webster, Medtronic, Boston Scientific, and St. Jude Medical. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1A. Apical four-chamber view of a patient with NFLG-AS.
Moving image 1B. Parasternal long-axis view of a patient with NFLG-AS.
Moving image 2A. Apical four-chamber view of a patient with PLFLG-AS.
Moving image 2B. Parasternal long-axis view of a patient with PLFLG-AS.
Moving image 3A. Apical four-chamber view of a patient with CLFLG-AS.
Moving image 3B. Parasternal long-axis view of a patient with CLFLG-AS.