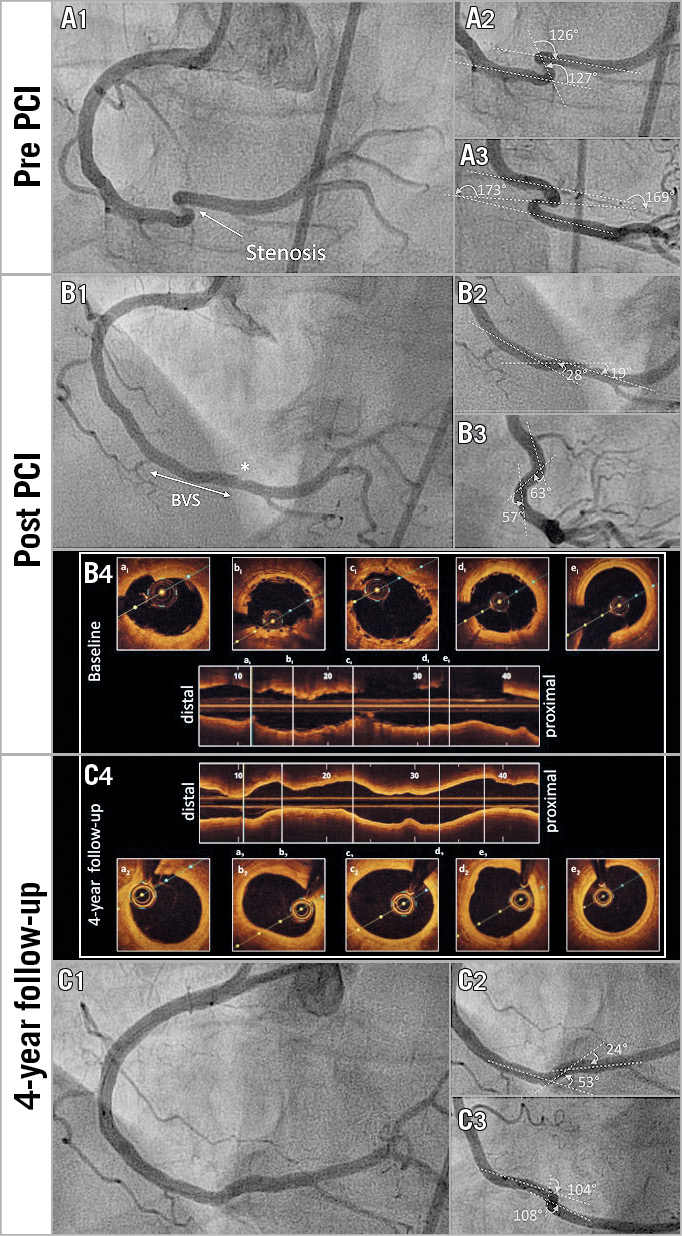
Figure 1. Pre- and post-treatment coronarography angiogram with OCT findings. A) Coronary angiogram of the right coronary artery showing the stenosis in the middle of a kinking of the distal artery (A1). The angles proximal and distal to the stenosis were >125° in both LAO 30°/cranial 20° (A2) and RAO 30° (A3) views. B) Modifications in vessel geometry immediately after bioresorbable vascular scaffold (BVS) implantation in LAO 30°/cranial 20° view (B1). The angles proximal and distal to the BVS were <90° in both LAO 30°/cranial 20° (B2) and RAO 30° (B3) views. Optical coherence tomography findings post PCI are shown (B4). C) Coronary angiogram of the right coronary artery at four-year follow-up in LAO 30°/cranial 20° view (C1). The angles proximal and distal to the BVS were <110° in both LAO 30°/cranial 20° (C2) and RAO 30° (C3) views. Optical coherence tomography findings at four-year follow-up are shown (C4).
We describe the case of a 68-year-old woman known to have cardiovascular disease who presented with crescendo angina pectoris. The coronary angiogram revealed a tight stenosis of the distal right coronary artery within an extreme kinking (Figure 1A1-Figure 1A3). After adequate lesion preparation with a 2.50/10 mm SC balloon, a 3.00/18 mm Absorb™ bioresorbable vascular scaffold (BVS) (Abbott Vascular, Santa Clara, CA, USA) was implanted (15 atm, 60 seconds). The immediate angiographic result was good, with improvement in the vessel geometry (Figure 1B1-Figure 1B3) compared to its initial anatomy (Figure 1A1-Figure 1A3). Optical coherence tomography (OCT) confirmed complete stent apposition (Figure 1B4).
Dual antiplatelet therapy consisted of aspirin lifelong and clopidogrel for 12 months. At four-year angiographic follow-up, the result was excellent with modification of the initial kinking to a more physiological anatomy (Figure 1C1-Figure 1C3). OCT confirmed complete BVS resorption (Figure 1C4). At five-year follow-up, the patient was asymptomatic.
Coronary kinking is considered to be one of the most notorious risk factors for stent fracture, encountered in up to 8% of drug-eluting stents (DES)1, and is thought to predispose to in-stent restenosis and stent thrombosis2. No recommendations exist regarding the type of stent to use in extreme kinking stenosis. Although first-generation BVS showed a higher risk of thrombosis in the first two years after implantation3, the risk vanishes with BRS disappearance and artery healing and permits a more physiological anatomy afterwards4. In contrast, metallic stents have a higher resistance to fracture, but the risk increases steadily with each heartbeat. In this case, with actual knowledge, we hypothesised that implanting a BVS instead of a DES would lessen the risk of long-term stent fracture and restore a more physiological vessel anatomy. The long-term clinical, angiographic and OCT results are actually in line with our expectations.
In conclusion, although the attractiveness of the first-generation BVS quickly disappeared, the second-generation BVS could be a suitable option for the treatment of complex anatomic lesions with extreme kinking. More literature is obviously needed in this field.
Conflict of interest statement
The authors have no conflicts of interest to declare.