Optical coherence tomography (OCT) is an intravascular imaging technique that provides high-resolution (10-20 μm) images. During percutaneous coronary intervention (PCI), OCT offers useful information to guide treatment strategies and assess optimal stent implantation (Figure 1). However, OCT remains markedly underused in the real world. For further integration of OCT into clinical practice, it is necessary to accumulate evidence showing that OCT has a beneficial impact on the outcomes of PCI. In 2012 and 2015, Prati et al1,2 reported the clinical benefits of OCT guidance in PCI using data from a large retrospective registry named CLI-OPCI (Centro per la Lotta contro l’Infarto-Optimisation of Percutaneous Coronary Intervention). The CLI-OPCI study demonstrated that OCT guidance in PCI was associated with a significantly lower risk of cardiac death or myocardial infarction during a one-year follow-up period in comparison with angiography guidance alone1. Subsequently, the CLI-OPCI II study showed that OCT-defined suboptimal stent implantation, defined as in-stent minimum lumen area <4.5 mm2, distal stent edge dissection >200 μm, or significant reference vessel plaque and lumen area <4.5 mm2 at either distal or proximal stent edges, was an independent predictor of device-oriented cardiovascular events (a composite of cardiac mortality, target vessel myocardial infarction, and target lesion revascularisation) during a one-year follow-up period2.

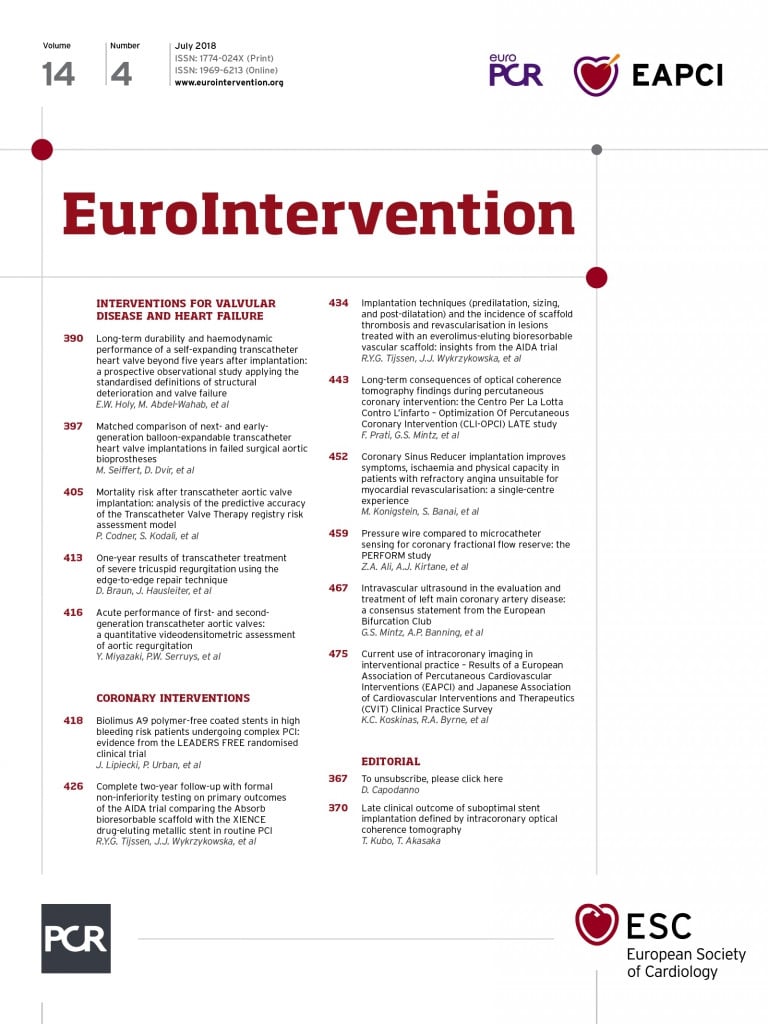
Figure 1. OCT images immediately after stent implantation. A) Stent malapposition. B) Stent underexpansion. C) In-stent tissue/thrombus protrusion (white arrow). D) Coronary artery dissection at stent edge (yellow arrow). E) Coronary artery dissection at reference segment (green arrow). *Guidewire artefact
Present study
In this issue of EuroIntervention, Prati et al3 report the results of the CLI-OPCI LATE study.
The CLI-OPCI LATE study evaluated the impact of OCT-defined suboptimal stent implantation at long-term follow-up. The authors demonstrated that: 1) during a median follow-up period of approximately three years, the presence of in-stent minimum lumen area <4.5 mm2, distal stent edge dissection >200 μm, or significant reference vessel plaque and lumen area <4.5 mm2 at either distal or proximal stent edges was an independent predictor of device-oriented cardiovascular events; 2) conversely, in-stent minimum lumen area divided by mean reference lumen area <70%, acute stent malapposition, and intrastent plaque/thrombus protrusion were not associated with worse outcomes; and 3) the impact of the suboptimal OCT-defined stent implantation was confined to the early phases of follow-up, while the clinical outcome was comparable after the first year.
OCT guidance in PCI
One major challenge for OCT is to develop criteria for optimal stent implantation. Previously, two pivotal studies used their own original OCT criteria for optimal stent implantation. The ILUMIEN III: OPTIMIZE PCI (OPtical Coherence Tomography Compared to Intravascular Ultrasound and Angiography to Guide Coronary stent Implantation: a Multicenter RandomiZEd Trial in Percutaneous Coronary Intervention) study defined acute procedural success as stent expansion of ≥90% (the minimum stent area of the proximal segment of the stent is ≥90% of the proximal reference lumen area, and the minimum stent area of the distal segment of the stent is ≥90% of the distal reference lumen area); no stent edge dissections classified as major (dissection with ≥60° of the circumference of the vessel or ≥3 mm in length); and no stent malapposition categorised as major (incomplete stent apposition associated with unacceptable stent expansion [<90%])4. The OPINION (OPtical frequency domain imaging versus INtravascular ultrasound in percutaneous coronary interventiON) study defined the goal of stent implantation as stent expansion of ≥90% (in-stent minimal lumen area is ≥90% of the average reference lumen area); complete apposition of the stent over its entire length against the vessel wall; symmetric stent expansion (minimum lumen diameter divided by maximum lumen diameter ≥0.7); and no plaque protrusion, thrombus, and edge dissection with potential to provoke flow disturbances5. However, these OCT criteria were not determined based on the clinical evidence; therefore, their clinical impact is unclear. The CLI-OPCI LATE study identified significant OCT criteria for stent implantation associated with clinical outcomes. Further prospective study will be required to investigate whether OCT guidance using the criteria determined in the CLI-OPCI LATE study improves outcomes of PCI.
Lack of assessment of the clinical impact of OCT before PCI is a weakness of the CLI-OPCI LATE study. According to previous studies, pre-PCI lesion assessment by using OCT helps to predict complications during PCI6-8. OCT-derived lipid-rich plaque with a thin fibrous cap is potentially associated with the no-reflow/slow-flow phenomenon after PCI6 and therefore may require the use of a distal protection device. A coronary bifurcation lesion with a small bifurcating angle and protruding carina has a high risk for side branch occlusion after main branch stent implantation7 and therefore may need the use of a second wire for side branch protection. A heavily calcified lesion including a thick and circumferential calcification is likely to cause stent underexpansion8 and therefore may warrant the use of a rotablator or cutting balloon. In addition, precise measurement of the reference lumen diameter and lesion length by using OCT helps to select the appropriate size of balloon and stent, which leads to a reduction in the incidence of tissue protrusion and stent edge dissection. Hence, OCT before PCI might play an important role for the guidance of PCI and induce changes in PCI procedures.
In the CLI-OPCI LATE study, 69% of the lesions with satisfactory angiographic results had OCT-defined optimal stent implantation. This suggests that the majority of lesions with satisfactory angiographic results do not require OCT assessment. OCT has some drawbacks including the cost of the imaging catheter and the additional time to perform imaging procedures. Therefore, routine use of OCT is not necessarily to be supported. Further efforts are needed to identify specific subgroups of patients in whom OCT is significantly effective for improving outcomes of PCI.
Final remarks
The CLI-OPCI LATE study determined the OCT criteria immediately after stent implantation for predicting late device-oriented cardiovascular events. The results of the CLI-OPCI LATE study will exert a direct influence on PCI optimisation strategies and also form a basis of future studies for OCT-guided PCI.
Conflict of interest statement
T. Kubo and T. Akasaka have received lecture fees and research funds from Abbott Vascular Japan Co., Ltd.