![]()
Abstract
This paper presents data on the nascence and development of the interventional cardiology service in Kazakhstan. It provides details of the structure of the Kazakhstan interventional cardiology service, staff training, the number of coronary and structural heart interventions for the period of 2010-2015, as well as the peculiarities of the capitation payment method. The number of coronary interventions is increasing year by year, though the number of intracoronary imaging techniques and intracoronary flow/pressure techniques remains inadequate. Structural heart interventions are mostly performed at tertiary hospital level, with an ever increasing number of transcatheter aortic valve implantation (TAVI) procedures.
Demographics and organisation
Kazakhstan is the ninth largest country in the world by area, with a population of 17.7 million (as of the year-end 2015) but ranks only No. 184 by its average density of population: 6.5 per km². Kazakhstan’s population is relatively young, with children under 15 accounting for 26.9%.
By Global Competitiveness Index for 2014-2015, Kazakhstan ranked No. 42 and by Health and Primary Education Index, Kazakhstan ranked No. 93 among 140 nations1. By Human Development Index in 2014, Kazakhstan ranked No. 70 among 187 nations and joined the high human development category.
EVOLUTION OF INTERVENTIONAL CARDIOLOGY AND CARDIAC SURGERY SERVICE
Interventional cardiology and cardiac surgery have long been underdeveloped in Kazakhstan. Suffice to say that in 2005 three national cardiac surgery centres performed a total of 171 coronary artery stenting procedures and 175 coronary artery bypass surgeries. With the implementation of the National Program on Boosting the Cardiology and Cardiac Surgery Care in the Republic of Kazakhstan for the period of 2007-2009, four regional cardiac surgery centres, based in the province/city hospitals, along with cardiac surgery departments were established in all of the fourteen province centres.
Further efforts were made to develop and improve the cardiology and cardiac surgery service under the Salamatty Kazakhstan (Healthy Kazakhstan) National Health Care Development Program for the period of 2011-2015. The number of cardiac surgery interventions significantly increased from 838 in 2005 to 30,249 in 2015: over 10,000 open heart surgeries and over 20,000 interventional cardiology procedures.
PHARMACEUTICAL SUPPLY
At outpatient level, over 400 pharmaceuticals are dispensed free of charge to more than two million Kazakhstani citizens under the government subsidised programme. Post stenting, dual antiplatelet therapy, such as aspirin plus clopidogrel or ticagrelor, is given free to all patients for 12 months. Only statins were recently removed from the free drug list.
UNTOWARD SPECIFICS OF THE KAZAKHSTAN HEALTHCARE SYSTEM
In spite of positive public health trends, Kazakhstanis’ life expectancy is almost ten years shorter than in OECD (Organization for Economic Cooperation and Development) countries and there is still a significant gap between the male and female life expectancy (8.82 years in 2014), with active working age men’s mortality exceeding that among women by 24%2.
Though hospital beds were cut by 14 thousand, the bed supply indicator in Kazakhstan is still 20% higher than in OECD countries, with longer average length of stay (ALOS): 9.5 inpatient days in 2014 vs. 6.0 in OECD countries. Over 60% of the public healthcare budget is channelled to in-patient hospitals.
The level of healthcare financing has increased considerably, from $3.86 billion in 2010 to $4.86 billion in 2014. However, the budget investments in the Kazakhstan healthcare sector are still significantly below the level seen in developed markets. Total health expenditure as % of GDP amounts to 3.6% in Kazakhstan vs. 9.4% in OECD countries. In general, current per capita healthcare expenditure in Kazakhstan is nine times lower than in OECD countries: $268 vs. $2,414.
ORGANISATIONAL STRUCTURE OF THE KAZAKHSTAN INTERVENTIONAL SERVICE
As of 2015, adult interventional care was provided by 47 cathlabs in 31 clinics, of which number seven are national level (tertiary level) healthcare facilities, 19 are province/city level clinics, one is a departmental institution (The Central Clinical Hospital under the Kazakhstan Presidential Administration), and the remaining four are private healthcare facilities. Of the 47 cathlabs, 38 deal with acute coronary syndrome in a 24/7 mode. Nine cathlabs stationed at the three national level hospitals and three privately run healthcare facilities manage elective cases only. Six cathlabs in six hospitals go without cardiac surgery support: four of them are operational 24/7, with a nearby cardiac surgery support clinic located 10 km (three clinics) and 50 km (one clinic) away.
Acute coronary syndrome is still closely monitored by the Ministry of Health and is on the top five healthcare development items list for 2016-2020. Through the media, the public is informed of the signs and symptoms of acute coronary syndrome (ACS) and what needs to be done when diagnosed with it. All cardiologists and interventional cardiologists take a one-week training in the ACS algorithm. Over the past few years, most percutaneous coronary intervention (PCI) centres have been equipped with a second angiographic set in order to ensure uninterrupted care to ST-segment elevation myocardial infarction (STEMI) patients. All PCI centres routinely monitor the time parameters of providing interventional care to STEMI cases: first medical contact-to-electrocardiogram (FMC-ECG), FMC-to-needle, and door-to-balloon. Though every effort is made to increase the number of primary PCIs we still cannot completely abandon a pharmacological invasive approach given the low density of Kazakhstan’s population and the huge distances (over 1,000 km at times) between neighbouring PCI centres.
OPERATORS AND STAFF TRAINING
One hundred and twenty-eight interventional cardiologists are employed at the above-mentioned 47 cathlabs. Personnel are provided with training at domestic universities. Retraining of specialists took 16 to 18 weeks: upon passing the qualification tests, a physician would be authorised to work as an interventional cardiologist. However, with the adoption of the Bologna education system in 2014, Kazakhstan medical university graduates are no longer able to have that short-term retraining. Instead, any physician seeking to become a highly specialised expert has to undergo a three-year residency training. Upon completion of the residency, physicians take qualification tests at the Specialised Test and Practical Skills Assessment Centres and, if successful, will be granted a Certificate of Specialism, which entitles them to work in a clinic. Although the average number of PCIs per operator is relatively small (around 100), most interventional cardiologists will engage in peripheral interventions and some will insert pacemakers.
REIMBURSEMENT POLICIES
During its development phase (2005-2010), the Kazakhstan interventional cardiology service focused on introducing as quickly as possible the world’s best interventional cardiology practices into its everyday clinical routine. To this end, under the ad hoc designed state programmes, cathlabs were set up in each province centre, physicians and nurses were trained in the leading local and foreign training centres, the world’s leading experts were invited to hold masterclasses, and premium quality equipment such as stents, balloon catheters, guiding catheters, etc., were procured from the world’s leading manufacturers.
Any new technology, as we saw, can best be disseminated if it is placed on the so-called HSHC (Highly Specialised Health Care) list, with a respective high capitation payment model in place. In each hospital, interventional cardiology units have turned into the most profitable and groundbreaking centres of excellence. Stenting interventions have become absolutely free for Kazakhstani citizens, while waiting lists are short or non-existent. Drug-eluting stent penetration in Kazakhstan has exceeded 80%, reaching 100% in some individual hospitals. No shortage of stents has ever been experienced, the payment being usage-based. All equipment (stents, balloon catheters, guiding catheters, coronary guidewires, contrast material, etc.) is thoroughly counted, and hospitals stocks are then replenished through the Health Care Services Reimbursement Committee. Later on, these data were used to calculate the average single stenting costs and the flat rate capitation payment system was introduced. Now, regardless of the number of stents implanted (one or four or five), the hospital gets a fixed payment, still extremely lucrative for it. For instance, even implanting two drug-eluting stents would earn a hospital over $2,000 per single stented patient, while medical treatment for other cardiovascular morbidities would earn that same hospital significantly less money.
All of the above has resulted in an exponential growth of new technologies in Kazakhstan. For example, the number of hi-tech managed cases increased fivefold over the period from 2010 to 2014. However, beginning from 2014, the universal usage of new technologies made it possible to downgrade about thirty such technologies, including PCI from the HSHC category to the Specialised Health Care category. This had an immediate impact on the level of remuneration for new-tech managed cases: in particular, PCI is now paid half as much. Under the new tariffs, only the first stent implanted will earn the hospital some money, while the second one brings it no profit; any further stent(s) will be implanted at the clinic’s expense. Fortunately, despite the virtually zero profit under the new tariffs, the number of stenting procedures has remained the same. However, the number of stents per procedure has decreased, the procedure has become staged (multi-stage PCI), and patients with multivessel lesions are now increasingly referred to surgeons for coronary artery bypass grafting (CABG); the latter being on the HSHC list is quite a lucrative procedure for any hospital, though practised commonly elsewhere.
Despite the decreased level of case management payments, the percentage of drug-eluting stents (DES) used remains high (above 80%). Bare metal stent PCI is paid less than DES PCI, roughly by the amount of the difference between the costs of these two types of stent. Thus, clinics are unable to earn more money through more frequent use of bare metal stents. This practice seems unacceptable, given the findings from the most recent research and the 2014 Myocardial Revascularisation Guidelines by the European Society of Cardiology.
Imaging and flow/pressure techniques, and atherectomy are not “carved out” from the total amount of remuneration for PCI: that is to say, a PCI procedure with or without the use of these methods will cost the same. As a result, these methods, sensibly underpaid as they are, have never gained popularity, and are used incidentally in a limited number of clinics.
All interventions and cardiac surgery operations, including left ventricular assist device (LVAD) implantation (a total of 240 such LVADs have been implanted to date), are performed free of charge. Patients enjoy unlimited access to these expensive devices. In Kazakhstan, we have a so-called hospitalisation portal, via which a patient may choose a hospital where they would like to undergo the aforementioned procedures or surgery. In other words, “money follows the patient”, that is to say clinics are motivated to create a steady patient inflow.
Private insurance companies are operational in the market. However, they do not cover expensive operations, such as PCI and CABG among others. Exceptions are only made for those individual clients who have special caveats in their insurance policies. A public mandatory health insurance is to be introduced in Kazakhstan starting from 2018.
NATIONAL REGISTRIES
We lack national interventional cardiology registries. However, in 2016 we launched a pilot version of the national registry “Acute Coronary Syndrome” in three regions of Kazakhstan. Three cathlabs (10%) participate in this registry, with local quality control (local audit) and no website so far. Once approved and duly improved, the registry will be universally used across the country.
NATIONAL WORKING GROUP
The National Public Association “The Kazakhstan Society of Interventional Cardiologists” was established in 2011, and currently has 120 members. The Society meets biannually, and holds its congresses in Astana (the capital city) and Almaty (the former capital city). In years between the congresses, there are visiting sessions out in the regions. The website of the Society is: www.endovascular.kz
Coronary interventions
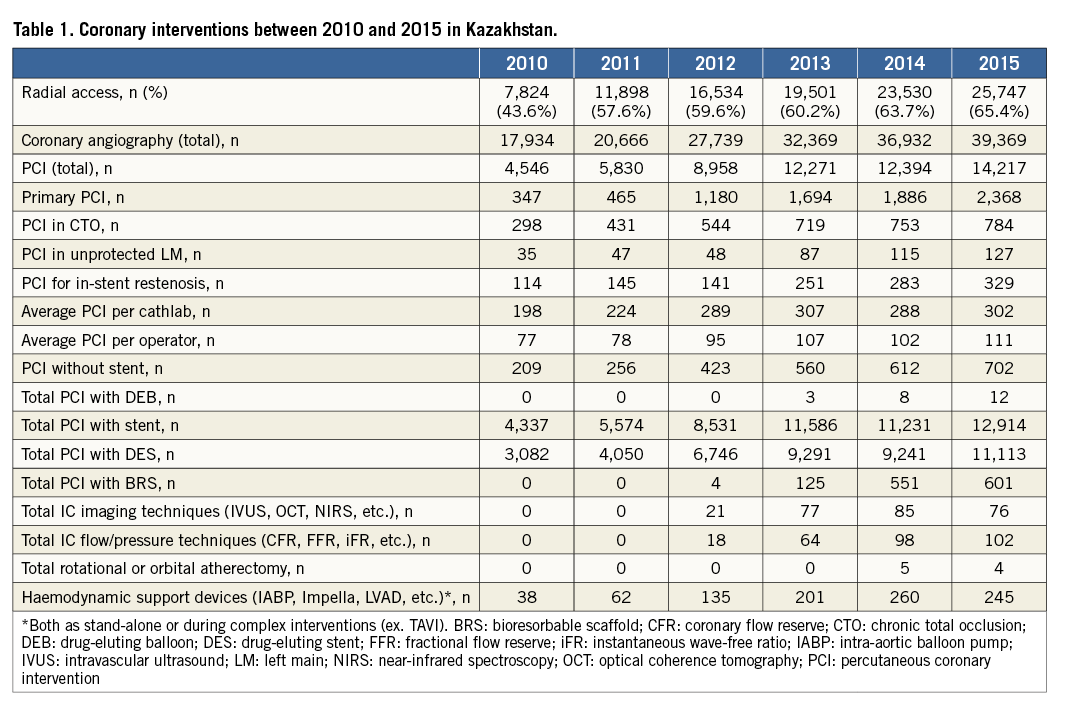
The number of coronary angiographies is increasing year by year, as is the number of radial access cases. The number of PCIs had also been on the rise before 2014 when reimbursement rules changed resulting in less capitated payment. That same year saw a decrease in average PCI per cathlab and per operator. Bioresorbable scaffolds (BRS) became available in Kazakhstan in October 2012. From that point onwards, we have seen a steadily growing trend in the number of BRS PCIs, with over half of those devices implanted in the Almaty City Heart Center. Drug-eluting balloons (DEB), intracoronary imaging and flow-pressure techniques, and rotational or orbital atherectomy, being highly expensive procedures, are not fully remunerated and are performed extremely rarely in Kazakhstan. Intra-aortic balloon pumps (IABP) are the only devices used for haemodynamic support purposes (Table 1).
Structural heart interventions
Structural heart interventions are also provided free of charge. They are still on the HSHC list, though originally the management case payment did include a negligible margin (profit) for a clinic, given the high prime cost of the devices. These interventions are mostly performed at the national level clinics. Alcohol ablation, mitral balloon valvuloplasty and other interventions on the mitral valve are still being performed sporadically, as they have been for many years now. Occluder implantations had been on the rise until 2014, and then their numbers dropped in 2015. This downward trend is likely to persist over the years to come as more and more patients are operated upon in their childhood. With the increasing percentage of the elderly, better diagnosis and more experienced operators, TAVI numbers have increased, and will continue to do so. All in all, 94 devices were implanted in five centres, with a non-uniform distribution among them: 64, 16, 10, 3 and 1 cases. Eighty-six cases (91.4%) were performed via the femoral access (Table 2).
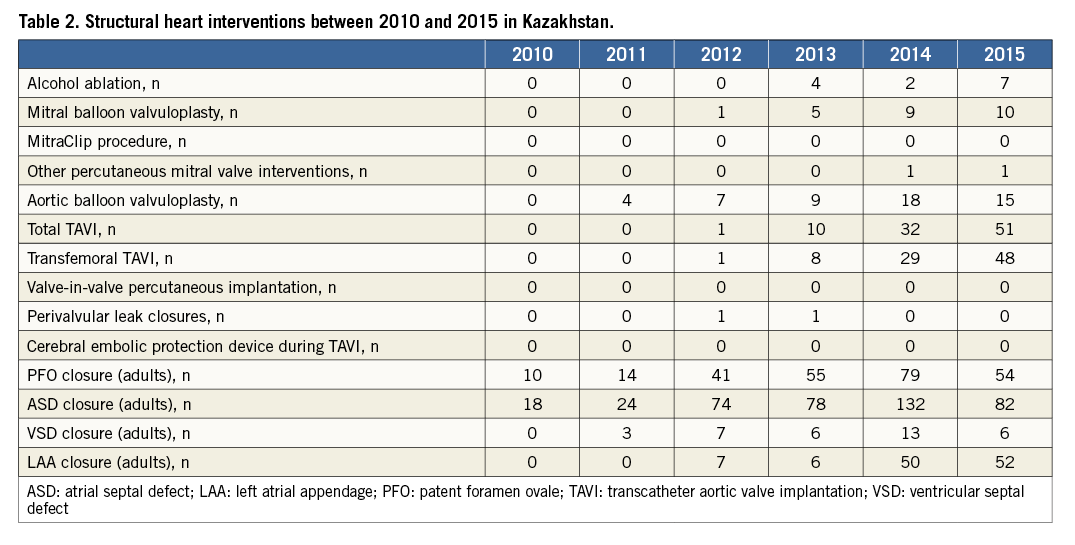
Lately, we began using innovative suture-closing techniques. A NobleStitch™ EL device (Nobles Medical Technology Inc., Fountain Valley, CA, USA) was used to suture close the patent foramen ovale in three patients in 2014 and another three in 2015. On 14 June 2016 at the National Research Cardiac Surgery Centre, upon completion of the first-in-man transapical aortic valve implantation in two patients, we used the HeartStitch™ TA device (Sutura Inc., Fountain Valley, CA, USA) to suture the left ventricle apex incision site.
Conflict of interest statement
The authors have no conflicts of interest to declare.

