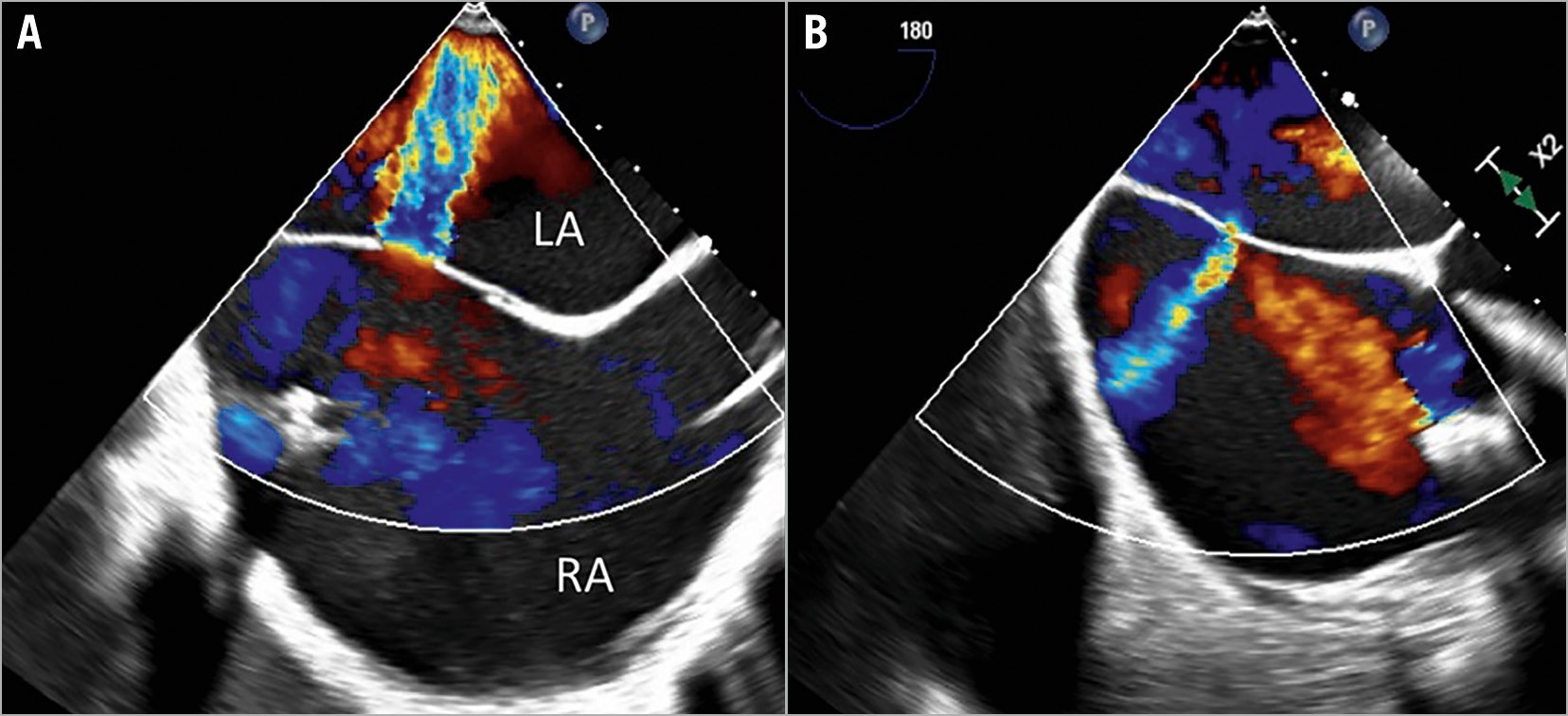
Figure 1. Intraprocedural transoesophageal echocardiography during simultaneous PMVR and PTVR. A) Interatrial shunt (IAS) (right-to-left) after PMVR and before PTVR. B) Reversal of IAS (left-to-right) after PTVR. LA: left atrium; PMVR: percutaneous mitral valve repair; PTVR: percutaneous tricuspid valve repair; RA: right atrium
An 83-year-old man presented with symptomatic primary severe mitral regurgitation (MR) and secondary massive tricuspid regurgitation (TR). The systolic pulmonary artery pressure was not elevated. The left and right ventricular function was moderately impaired. Due to high surgical risk, a simultaneous percutaneous mitral valve repair (PMVR) and tricuspid valve repair (PTVR) was performed under deep sedation with propofol without endotracheal intubation. The decision for simultaneous PMVR and PTVR was made by a multidisciplinary Heart Team.
For PMVR, a PASCAL device (Edwards Lifesciences, Irvine, CA, USA) was placed between the anterior and posterior leaflets resulting in a reduction of severe MR to a residual moderate MR (reduction of 3D effective regurgitant orifice area [EROA] from 0.58 cm2 to 0.28 cm2) (Moving image 1, Moving image 2). No further device was placed because of a slightly elevated transmitral pressure gradient. A reduction of mean left atrial (LA) pressure was observed after PMVR (20 mmHg to 12 mmHg). A post-PMVR iatrogenic atrial septal defect (ASD) with a deoxygenating right-to-left interatrial shunt (IAS) was observed (Figure 1A, Moving image 3), due to effective reduction of the MR and remaining massive TR. A decrease in peripheral oxygen saturation was observed and high-rate oxygen supply was needed to stabilise the patient (SaO2 91% under 9-15 l*min–1). Prior to PTVR, the mean right atrial (RA) pressure was 20 mmHg. For PTVR, a PASCAL Ace device (Edwards Lifesciences) was implanted between the septal and anterior leaflets resulting in a significant TR reduction from massive to moderate (reduction of biplane vena contracta width from 15 mm to 6.8 mm) (Moving image 4-Moving image 7) and mean RA pressure reduction to 7 mmHg. Subsequently, a reversal of the IAS was observed, resulting in a left-to-right shunt (Figure 1B, Moving image 8), proving the effectiveness of the TR reduction and leading to respiratory stabilisation of the patient. Therefore, an ASD closure was not indicated. The patient reported an improvement of dyspnoea and no fluid retention at the three-month follow-up.
Right-to-left IAS as part of PMVR should be considered in patients with concomitant severe, massive or torrential TR. Simultaneous PMVR and PTVR might be a solution in such cases. Periprocedural ASD occlusion remains an option in case of relevant shunts1 but prevents subsequent PMVR if optimisation is needed. However, its prognostic effects need to be proven2. Future studies are required to confirm the feasibility, safety and efficacy of simultaneous PMVR and PTVR.
Conflict of interest statement
T. Geisler reports personal fees from AstraZeneca, Boehringer Ingelheim, Pfizer, and Ferrer, grants and personal fees from Bayer Healthcare, Bristol Myers Squibb, Daiichi Sankyo, and Eli Lilly, and has received research grants and personal fees from Medtronic and Edwards Lifesciences. J. Schreieck received speaker fees from Bayer Healthcare, Edwards Lifesciences and Boston Scientific. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. MR before PMVR.
Moving image 2. MR after PMVR.
Moving image 3. IAS before PTVR.
Moving image 4. TR before PTVR.
Moving image 5. TR after PTVR.
Moving image 6. TR before PTVR transgastric view.
Moving image 7. TR after PTVR transgastric view.
Moving image 8. IAS after PTVR.