Introduction
Remodelling of the left ventricle (LV) after a myocardial infarction (MI) results in increased volumes and a reduced ejection fraction (EF). The transmurality of the infarction determines whether a true LV aneurysm will result. Patients with advanced ischaemic cardiomyopathy often suffer recurrent episodes of cardiac decompensation with the need for multiple hospitalisations; they have a limited prognosis. Mixed outcomes have been demonstrated after conventional surgical LV reconstruction1,2. We describe a novel hybrid transcatheter technique to reconstruct the remodelled LV by plication of the anteroseptal LV scar, in order to reduce the enlarged LV volume, decrease the wall stress and increase the EF.
Methods
The procedure, called less invasive ventricular enhancement (LIVE), has the objective of reconstructing the LV by plication of fibrous scar and relies on the micro-anchoring technology of the Revivent TC™ Ventricular Enhancement System (BioVentrix Inc., San Ramon, CA, USA) (Figure 1). This system consists of a number of paired anchors connected by a poly-ether-ether-ketone (PEEK) tether that, once properly positioned, are pulled together with a controlled force by means of a specialised force gauge and finally released. The Revivent TC System represents the evolution of its previous fully surgical version. Major steps forward are represented by the avoidance of both sternotomy and extracorporeal circulation.

Figure 1. Internal and external anchor.
Patients eligible for the procedure present with symptomatic heart failure (NYHA Class ≥II) and ischaemic cardiomyopathy (EF <40%) after anteroseptal MI resulting in a dilated LV with an akinetic/dyskinetic scar in the anteroseptal wall and apex.
Preoperative planning requires gadolinium-enhanced magnetic resonance imaging (MRI) (or alternatively contrast computed tomography [CT]) to define the scar morphology clearly. Scarred regions must comprise at least 50% of the wall thickness to enable safe anchor implantation. The LIVE procedure is a hybrid transcatheter procedure performed by both an interventional cardiologist (IC) and a cardiothoracic surgeon (CTS) in co-operation. Additional support is provided by the presence of a cardiologist skilled in three-dimensional transoesophageal echocardiography (3D-TEE).
LV reconstruction is achieved by implantation of a series of internal and external micro-anchors and brought together over a PEEK tether to form a longitudinal line of apposition between the LV free wall and the anterior septum of the right ventricle (RV) (Figure 2). Typically, two to three pairs are used, depending on the size of the LV and the areas of akinesia/dyskinesia. These “RV-LV” anchor pairs are used in combination with a final “LV-LV” anchor pair that is placed through the LV apex. The aim is to achieve a conical reconstruction of the LV with a completely excluded endoventricular scar and an LV volume reduction of 30-40% (Figure 3).
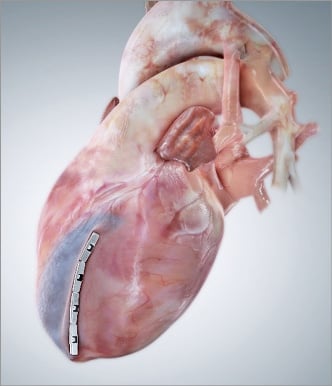
Figure 2. External anchors and plicated LV.
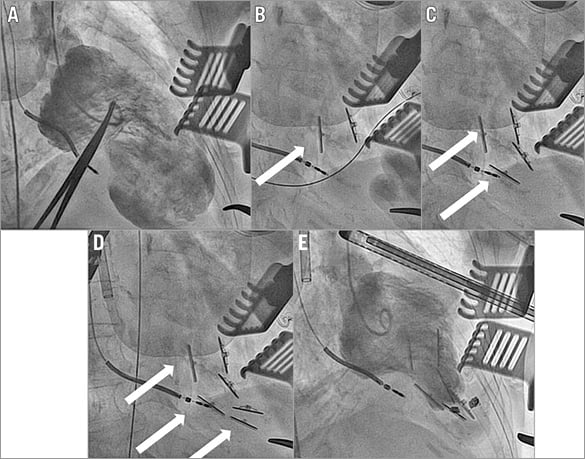
Figure 3. Intraprocedural images with basal LV angiogram (A), subsequent anchor-pair placement (B, C, D) and final result (E).
Results
The CTS performs a left-sided anterolateral minithoracotomy through a 7-8 cm skin incision and accesses the left pleural cavity through the 4th or 5th intercostal space. The IC accesses the right internal jugular vein (RIJV) using the standard technique, with placement of a 14 Fr introducer reaching the right atrium (RA). A Swan-Ganz balloon-tipped catheter is then introduced and advanced to the RV outflow tract (RVOT)/pulmonary artery (PA) via the RV apex and along the free wall of the RV. A 0.025” stiff guidewire is placed into the Swan-Ganz catheter and the 14 Fr sheath is advanced into the RV. The Swan-Ganz catheter is then exchanged for an 8 Fr multipurpose catheter (MP), leaving the 0.025” wire in the RVOT. A multi-looped snare is advanced though the MP and deployed in the RVOT. This will serve to capture a 0.018” guidewire delivered by the CTS through the LV free wall and across the scarred ventricular septum. At this point, the tricuspid valve is evaluated by transoesophageal echocardiography (TEE) for competence.
TRANSVENTRICULAR NEEDLE PLACEMENT
The CTS inserts an 18 G and 10 cm long standard needle 1-2 cm under the LAD through the scarred LV free wall, guided by fluoroscopy, TEE and continuous pressure monitoring. The needle is aimed at the (also scarred) anterior to mid interventricular septum and is advanced towards the RV. The septal puncture location is defined by preoperative MRI or CT. Once entry into the RV cavity is verified, a 0.032” guidewire is advanced into the RV. A 6 Fr dilator is then placed over the 0.032” wire and brought to the RV. The 0.032” wire is withdrawn and a 5 Fr Amplatz Right Mod Catheter (AR) with a right-angle tip is advanced to the RV. The AR directs the 0.018” guidewire into the RVOT and towards the multi-looped snare.
WIRE SNARING AND RETRIEVAL
Once the 0.018” guidewire is through the loops of the snare, the 0.025” stiff guidewire is withdrawn and the snare is pulled back to grab the 0.018” guidewire. The MP is then advanced over the 0.018” guidewire and the snare. The CTS advances the AR to the tip of the MP. The snare, 0.018” guidewire, and the MP are withdrawn through the 14 Fr introducer. In a carefully coordinated manner, the CTS initially advances the AR through the LV and then into the 14 Fr introducer. The IC continues retracting the MP through the 14 Fr introducer and the CTS continues to advance the AR until wire and catheter are completely across the heart from the LV free wall through the septum and RV then out of the RIJV. The 0.018” wire is then exchanged for a 0.014” wire.
INTERNAL ANCHOR INSERTION AND PLACEMENT
The internal anchor assembly with the “over-the-wire” tether is advanced over the 0.014” wire by the IC from the RIJV. This wire must be kept under tension by both surgeon and cardiologist at all times to allow smooth advancement. The internal anchor assembly is advanced into the 14 Fr introducer ensuring proper orientation for seating on the septum (anchor hinge towards patient’s midline). Simultaneously, the CTS pulls in synchrony with the IC on the opposite end of the anchor tether. Once the internal anchor reaches the RV septum, the 14 Fr introducer is slightly withdrawn, exposing the anchor. The thumb switch on the assembly anchor handle is activated and rotated if necessary to gain proper alignment parallel to the septum.
EXTERNAL ANCHOR ATTACHMENT
The CTS grasps the exposed tether protruding from the LV free wall and places the external anchor onto it. The anchor is advanced until slight resistance is felt at the epicardial surface. It is critical to maintain such tension on the anchor tether so that the internal anchor remains properly positioned on the RV septum. Once placed, the tether can be bent away from the surgical field and clamped temporarily with a mosquito clamp. The IC releases the internal anchor from the delivery system by turning the release mechanism completely. Final disengagement is performed after checking accurate positioning on fluoroscopy. Until that point, the anchor assembly can still be retrieved and withdrawn (Moving image 1).
The procedure continues with placement of anchor pairs until complete plication of the scarred wall, using the previously implanted anchor as reference. Adjacent anchors do not need to be in direct contact to obtain full exclusion. The recommended sequence is to start with the most apical “RV-LV” anchor-pair placement and proceed towards the more basilar regions with additional anchors.
APICAL ANCHOR PLACEMENT
The last anchor pair is placed at the LV apex beyond the point at which the RV extends, dictating the final conical shape of the reconstructed LV. The CTS begins by identifying the scarred regions of the LV apex and palpating the most apical “RV-LV” anchor pair. Using a strong needle holder, the needle tip of the apical anchor assembly is then directed from the right side of the LV apex towards the left. Once the needle tip is seen protruding out of the left side of the apex, it is grasped and the tether pulled through the apex and out of the incision. The needle tip is cut from the tether and, as before, an external anchor is mounted to the exposed tether.
Discussion
The LIVE technique is a novel hybrid transcatheter technique to reconstruct a remodelled LV in patients with symptomatic ischaemic heart failure. By means of micro-anchoring technology, the myocardial scar is plicated, which reduces the enlarged LV volume, decreases the wall stress and increases the EF. It is a minimally invasive and “off-pump” alternative to the classic surgical ventricular reconstruction.
Limitations
At present, the main limitation of this technique is represented by its applicability only in patients with previous antero-septal-lateral infarction, while patients with infarctions in other territories are not candidates for this procedure.
Conclusion
This minimally invasive technique has the promise of offering an effective LV reconstruction at lower risk in a very high-risk group of patients.
| Impact on daily practice The LIVE technique is a promising innovation with the potential to offer a new treatment option for patients with advanced ischaemic cardiomyopathy. The relatively suboptimal results currently offered by the conventional surgical interventions1 could be overcome by this novel less invasive technique, thus adding a valuable tool for the treatment of these delicate patients. |
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Detailed animation reproducing all steps of the LIVE technique.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Detailed animation reproducing all steps of the LIVE technique.