Introduction
Paravalvular aortic regurgitation (AR) is a notable complication in transcatheter aortic valve implantation (TAVI) associated with worsened outcomes; yet, assessment of AR remains problematic1.
Contrast aortography is a well-established technique; however, the current standard is semi-subjective with considerable inter-observer variability2. Quantitative video-densitometry used digital assessment of opacification in the left ventricle (LV) and aorta with greater reproducibility than visual grading; however, overlap of the descending aorta remains a significant source of non-analysability3,4.
Due to anatomical variation, no specific projection can be reliably applied without overlap. An ideal technique would determine an overlap-free projection (OFP) irrespective of anatomical variations using minimal radiation exposure and without radiopaque contrast.
We hypothesised that the position of the descending aorta relative to the LV and aortic root can determine the OFP. We report here on the development and validation of an OFP rule.
Methods
The development cohort was identified from patients referred for TAVI at a tertiary centre with computed tomographic angiography (CTA) of adequate quality. The validation cohort was identified from patients undergoing contrast aortography or ventriculography via transfemoral access at two international centres for intraoperative TAVI assessment or an unrelated clinical indication.
CTA scans were analysed using syngo software (Siemens AG, Erlangen, Germany) to create a 3D image with the LV and aorta isolated by image cropping. The region of interest (ROI) was defined as LV apex to aortic root, 2 cm above the sinotubular junction. In the anteroposterior (AP) view, a line was drawn through the ROI (Figure 1) with a vertical reference line (VRL) hemisecting the first line. The descending aorta was defined relative to the VRL (right or left). The 3D image was rotated along the vertical axis to determine the minimum angulation where the descending aorta did not overlap the ROI. This step was carried out in left anterior oblique (LAO) and right anterior oblique (RAO) views with the lower angulation defined as the OFP.
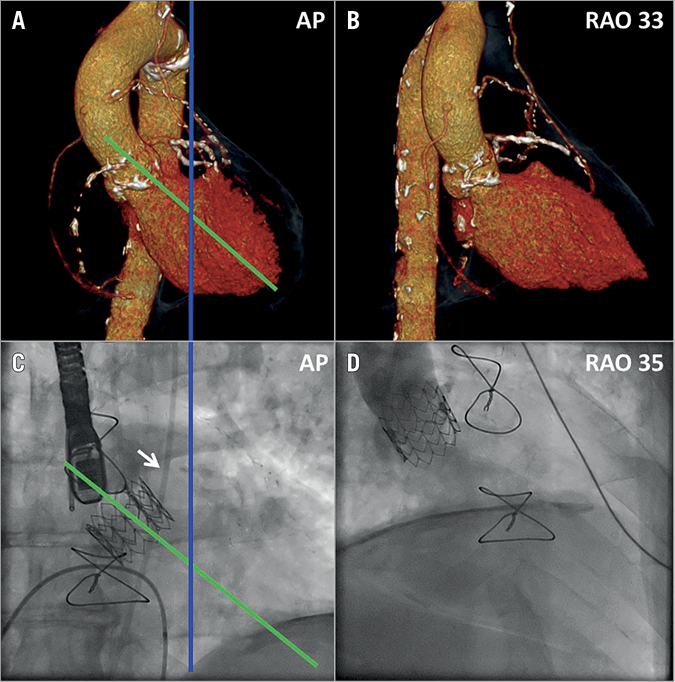
Figure 1. Demonstration of OFP using CTA and applicability to contrast aortography. On a three-dimensional CT reconstruction of the LV and aorta in anteroposterior projection (A) the region of interest is indicated by the green line. This line is hemisected by a blue vertical reference line (VRL) showing the descending aorta on the right side of the patient. The lowest angulation with no overlap of the aortic root or LV over the descending aorta, i.e., overlap-free projection (OFP), was obtained at RAO 33° (B). Fluoroscopy in the AP projection (C) shows a pigtail catheter (arrow) in the descending aorta to the patient’s right of the VRL. Aortography at RAO 35° (D) shows the OFP in fluoroscopy.
For fluoroscopic assessment, a cine acquisition was taken in the AP view and the above method was applied. As the descending aorta is not visible without contrast, a pigtail catheter (via transfemoral access) was used as a proxy. Contrast aortography or ventriculography was performed in the RAO or LAO view depending on the position of the descending aorta to the VRL. Although operators were aware of recommended angles (based on development cohort data), the final angulation was not pre-specified.
STATISTICAL METHODS
Descriptive statistics used median (25th to 75th percentile) for variables without a normal distribution and n (%) for categorical variables. SPSS, Version 20.0 (IBM Corp., Armonk, NY, USA) was used. The chi-square test was used to compare proportions.
Results
A total of 65 CTA scans were suitable for review as the development cohort and an independent cohort of 81 patients was assessed for fluoroscopic validation.
In the CTA development cohort, 58 (89.2%) patients had a descending aorta to the patient’s right of the VRL, whereas seven (10.8%) were to the left. The relative position of the descending aorta to the VRL was associated with an ipsilateral OFP in 64 (98.5%) cases. In cases where the OFP was in the RAO view, the median angle was 35° (31°-39°); in the LAO view the median angle was 35° (31°-45°).
To stratify cases where higher angulation was required, patients were classified as “medial” or “lateral” depending on aorta position. “Medial” position was defined as the descending aorta crossing the VRL within the superior and inferior limits of the ROI, and “lateral” position was defined as no crossover of the descending aorta. There were 37 “medial” and 28 “lateral” cases. The OFP in medial vs. lateral position was 38° (35°-41°) vs. 31° (23°-34°), respectively. From these data, a rule was developed to estimate the OFP for fluoroscopy (Figure 2).
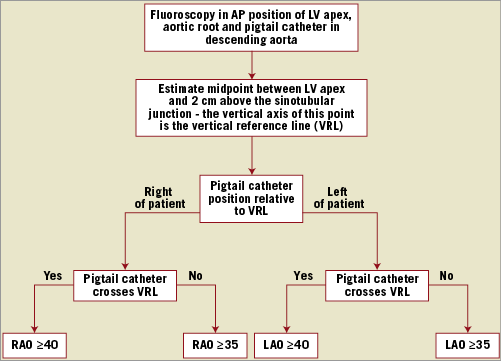
Figure 2. A stepwise approach using fluoroscopy to obtain an overlap-free projection. AP: anteroposterior; LAO: left anterior oblique; LV: left ventricle; RAO: right anterior oblique
In the fluoroscopic validation cohort, the aorta was to the patient’s right of the VRL in 76 (94%). A “medial” aortic position was observed in 14 (17%) and a “lateral” position in 67 (83%) cases. In 41 (51%) patients the projections used were as recommended by the OFP rule (“within rule”: median 35° [35°-36.5°]). In 40 (49%) patients the projections used were not recommended by the OFP rule (“outside protocol”: median 29° [25°-30°]). The reasons for cases being “outside protocol” were: contralateral projection to aortic position in six (15%) and angulation lower than recommended in 34 (85%) by a median 7° (5°-11.5°).
When the projections used were in keeping with the OFP rule (“within rule”), the angiography was free from overlap in almost all cases and the proportion was greater than for those that were “outside protocol” (40 [98%] vs. 18 [45%], p<0.001). In cases where an OFP was obtained despite being “outside protocol”, the angle used was a median 6° (5°-7°) lower than recommended.
Discussion
This study reports the development and validation of a rule to determine reliably the OFP for quantitative contrast aortography. Overlap results in a double hit of contrast which obfuscates assessment. Although OFP may be determined with repeated imaging, this exposes the patient to additional contrast and radiation.
Our data show that the OFP is predominantly ipsilateral to the descending aorta position relative to the VRL and the degree of angulation is dependent on aortic position. If the descending aorta is medial, higher angulation is needed for separation of structures; conversely, if the descending aorta is significantly lateral, OFP is achievable at lower angulation, although caution is needed as catheter bias within the aorta, aortic root dilatation or extreme tortuosity cannot be appreciated without contrast. Despite these factors the rule we have proposed provided robust results.
Recently, Abdelghani et al4 reported on video-densitometry analysis of AR using the left ventricular outflow tract as the ROI. Although this method reduces the potential for overlap, in this study 22% of cases were non-analysable due to overlap. Our rule uses geometric principles to improve feasibility irrespective of ROI.
Limitations
The OFP angle from CTA and fluoroscopy may differ due to blooming effects or catheter bias. We found that, in patients with both CTA and fluoroscopy available, the OFP was approximately 5° lower in fluoroscopy. The fluoroscopic technique relies on a catheter in the descending aorta; if radial access is used, the descending aorta position should be assessed on CTA or by other radiopaque structures.
Conclusions
This method effectively solves a fundamental problem previously encountered in steps towards standardising quantitative aortography studies by using a simple approach to obtain the OFP with either fluoroscopy or CTA.
| Impact on daily practice This article describes a simple method for obtaining an overlap-free projection for video-densitometry, facilitating further development and validation of quantitative methods. |
Conflict of interest statement
The authors have no conflicts of interest to declare.