CASE SUMMARY
BACKGROUND: An 80-year-old, hypertensive, hypercholesterolaemic patient with a history of previous coronary artery bypass graft was admitted for an acute coronary syndrome and underwent a coronary angiography revealing three-vessel disease with occlusion of the venous grafts, patency of the left internal mammary artery and a significant aneurysm at the bifurcation of the left anterior descending artery with its first diagonal branch.
INVESTIGATION: Coronary angiography, intravascular ultrasound, coronary computed tomography.
DIAGNOSIS: Coronary bifurcation wide-neck aneurysm.
MANAGEMENT: Percutaneous Y-stent-assisted coil embolisation.
KEYWORDS: aneurysm, coil embolisation, coronary bifurcation
PRESENTATION OF THE CASE
An 80-year-old, hypertensive, hypercholesterolaemic patient with a history of previous coronary artery bypass graft in 1994 was admitted to our institution because of a non-ST-segment elevation myocardial infarction. Coronary angiography revealed three-vessel disease with occlusion of the venous grafts to the obtuse marginal branch and the posterior descending artery, and patency of the left internal mammary artery grafted to the left anterior descending artery (LAD). The first diagonal branch (D1) had not been bypassed despite having a good calibre. Moreover, an aneurysm measuring 6×7 mm was found at the bifurcation of the LAD with D1 (Figure 1), proximal to two big septal perforator branches and the bypassed stenosis. Since echocardiography showed inferior wall hypokinesis, percutaneous coronary intervention was performed in the native right coronary artery. Then, an imaging study of the aneurysm was undertaken with intravascular ultrasound (IVUS) revealing the aneurysm developing from the LAD, with D1 origin being only 1 mm proximal to the aneurysm itself (Figure 2A). Coronary computed tomography subsequently confirmed this anatomy (Figure 2B).
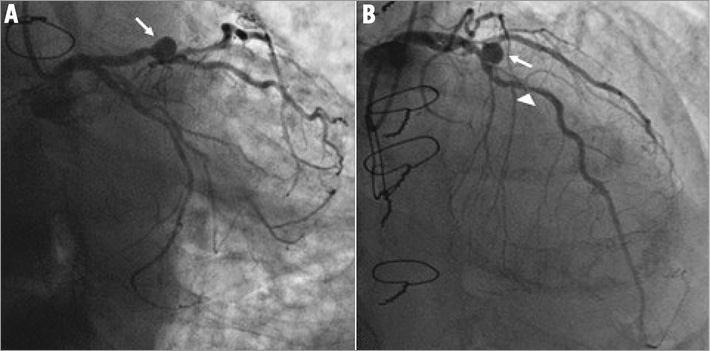
Figure 1. Coronary angiograms showing a coronary aneurysm (arrow) at the bifurcation between the left anterior descending coronary artery and its first diagonal branch. Coronary artery disease had been previously treated by coronary artery bypass graft (sternum sutures); however, the first diagonal branch had not been bypassed. The aneurysm had developed on the left anterior descending coronary artery proximally to two big septal perforator branches and its bypassed stenosis (arrow head). A) Left oblique anterior caudal projection. B) Right anterior oblique cranial projection.
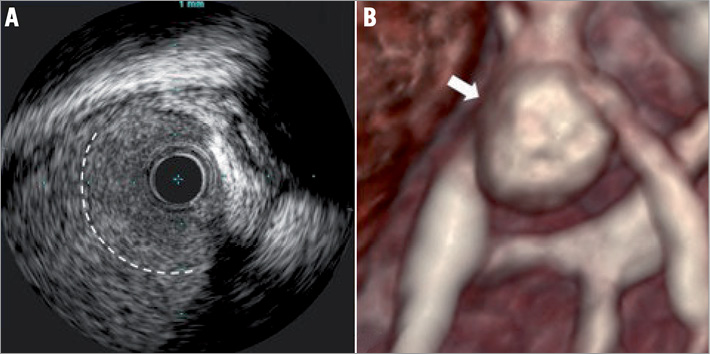
Figure 2. Intravascular ultrasound (IVUS) imaging of the aneurysm (A) showing the large neck of the aneurysm (dotted line). Computed tomography three-dimensional reconstruction (magnification) of the aneurysm demonstrating the origin of the first diagonal branch from the left anterior descending coronary artery 1 mm proximal to the aneurysm (B). The arrow shows the point of the IVUS section.
How would I treat?
THE INVITED EXPERT’S OPINION
This is a really nice case for discussion. A few initial questions come to mind - was the RCA territory felt to be the cause of the acute coronary syndrome (perhaps due to closure of the PDA vein graft)? Was the patient asymptomatic prior to this? And lastly, was there any evidence of aneurysm formation at the time of the bypass in 1994? For the sake of argument, I will answer these questions as yes, yes, and no, respectively.
The question then becomes, “Do we need to do anything to the LAD/D1 bifurcation?”.
As far as the LAD is concerned, the issue is not ischaemia - the vessel is well supplied distally by a LIMA graft - the issue is risk of aneurysm rupture. The natural history of coronary aneurysms “remains obscure”1 but there is an incidence of rupture. In this particular case, however, that risk might be mitigated by likely pericardial adherence following CABG.
For the D1, the issue is ischaemia. Angiographically the stenosis appears significant. This could be confirmed with a pressure wire –but even if this vessel is ischaemic, is it accounting for any symptoms, or for more than 5% of the total myocardial mass? Is it important enough to treat2?
If we decide to treat the LAD aneurysm one option is to exclude it using a covered stent. These stents are prone to neointimal hyperplasia, but restenosis is of no concern here due to the LIMA. Unfortunately, IVUS shows that the neck of the aneurysm is only 1 mm beyond the bifurcation and therefore stent placement could risk inadvertent occlusion of the D1 (in addition to the first septal). Therefore, a better option might be to consider coiling the aneurysm, bearing in mind that a wide-necked aneurysm is easier to access, but harder to isolate.
If treating this lesion, I would therefore take an XB3 guide (Cordis, Johnson & Johnson, Warren, NJ, USA), a Runthrough extra-floppy wire (Terumo Corp., Tokyo, Japan) to the LAD, a Runthrough hypercoat (Terumo) to the D1 and an Echelon microcatheter (ev3 Endovascular, Inc., Plymouth, MN, USA). I would pass the guidewire into the aneurysm and advance the microcatheter over it. I would take a 5 mm×20 cm Helix coil (ev3) and gently feed this into the aneurysm to protect the patient from potential later rupture. Having done this, I would predilate the D1 at the bifurcation and would stent it from LAD to D1 with a 2.5×18 mm BioMatrix™ stent (Biosensors International, Morges, Switzerland). Proximal optimisation3 would be performed with a 3×6 mm Hiryu® balloon (Terumo). There would be no need for a kissing balloon dilatation (which would necessarily deform the stent) as the LAD is supplied by the LIMA.
Leaving aside the interesting intellectual challenges of treating this patient, in reality how would we treat this lesion in my institution? At our MDT we would discuss the options above, and an interesting theoretical discussion would ensue. But after some chin scratching and intellectual posturing, we would, I hope, decide to treat this asymptomatic 80-year-old man with “masterly inactivity”4.
Conflict of interest statement
The author has no conflicts of interest to declare.
How would I treat?
THE INVITED EXPERTS’ OPINION
Coronary artery aneurysms can be treated conservatively, surgically or percutaneously. In this case, the size of the aneurysm (6×7 mm) makes medical therapy difficult, as the risks of progression, rupture and impingement of the ungrafted first diagonal can be high. Surgical treatment would perhaps be a possibility, but this would carry a significant risk since this would be a re-do operation, which is inherently associated with higher risks. Such risks are augmented by the patient’s advanced age and also the fact that he is on dual antiplatelet therapy. In addition, a re-do operation would put the anastomosed left internal mammary artery (LIMA) at risk, which at the point of presentation was patent with good flow in the left anterior descending artery (LAD).
Placement of a covered stent (Direct-Stent® Stent Graft; InSitu Technologies, St Paul, MN, USA; Be graft; Bentley InnoMed, Hechingen, Germany; JOSTENT GRAFTMASTER; Abbott Vascular, Santa Clara, CA, USA; Over and Under® Pericardium Stent; ITGI Medical Ltd, Or Akiva, Israel) from the LAD towards the diagonal is an option as the LAD is grafted, although this could compromise flow in the nearby septal perforators and still allow retrograde flow from the LIMA to the aneurysm. The simultaneous inflation of a covered stent towards the LAD and a protection balloon in the diagonal can be performed with a 6 Fr guiding catheter, though this does not resolve the potential issue of septal occlusion. The same applies for an approach utilising a covered stent with a preformed hole for the diagonal that is delivered over two wires5.
Another approach would be coil embolisation. This can be either “unassisted” or “stent-assisted” and is an approach that is widely used in the treatment of intracerebral aneurysms. Recently, a case of successful “stent-assisted” embolisation of a distal left main stem (LMS) aneurysm extending to the LAD has been reported6. A “stent-assisted” approach would be preferred here if coil embolisation is chosen, due to the aneurysm’s wide neck, as this would reduce the risk of coil prolapse and migration. Coil placement can take place either before or after stent placement. The advantage of this technique is that it allows access to the nearby branches, which can be treated if required, whilst also ensuring treatment of the aneurysm.
Among all the proposed techniques, the one which in our view appears the most simple is the use of the MGuard™ stent (InspireMD, Inc., Tel Aviv, Israel) as the mesh surrounding the stent would probably interfere sufficiently with laminar flow in the aneurysm causing this to thrombose. Furthermore, if flow in any of the nearby branches is affected, these could be wired through the mesh with subsequent balloon dilatation. In addition, this allows coil embolisation to be performed in the future if the desired result is not obtained following placement of the MGuard stent.
Conflict of interest statement
A. Latib serves on a Medtronic advisory board. The other authors have no conflicts of interest to declare.
How did I treat?
ACTUAL TREATMENT AND MANAGEMENT OF THE CASE
The patient was discharged with indication to elective percutaneous coil embolisation of his coronary artery aneurysm, joining interventional cardiology skills and neuroradiology technique in order to preserve D1 patency while achieving a safe and effective exclusion of the aneurysm. Indeed, after standard heparinisation and following wiring of both LAD and D1, a bare metal stent was implanted in the LAD to support coils packing into the aneurysm and improve the safety and efficacy of the next steps (Figure 3A). After rewiring D1 through the struts of the LAD stent, a microcatheter was advanced into the aneurysm over a coronary wire (Figure 3B, Moving image 1) and six Guglielmi detachable coils were successfully released and packed into the aneurysm (Figure 3C, Moving image 2). At the end of the procedure, the patient suddenly complained of chest pain and an electrocardiogram showed ischaemic changes in lateral leads. Angiography showed thrombotic occlusion of proximal D1 (Figure 4A) which was promptly reopened by balloon dilation. Then, an IVUS pullback documented coil prolapse within the branch (Figure 4B). The percutaneous bifurcation intervention was therefore completed with a second bare metal stent implanted in D1 according to the T stenting and small protrusion (TAP) technique (Figure 5A), yielding a very nice final result (Figure 5B).
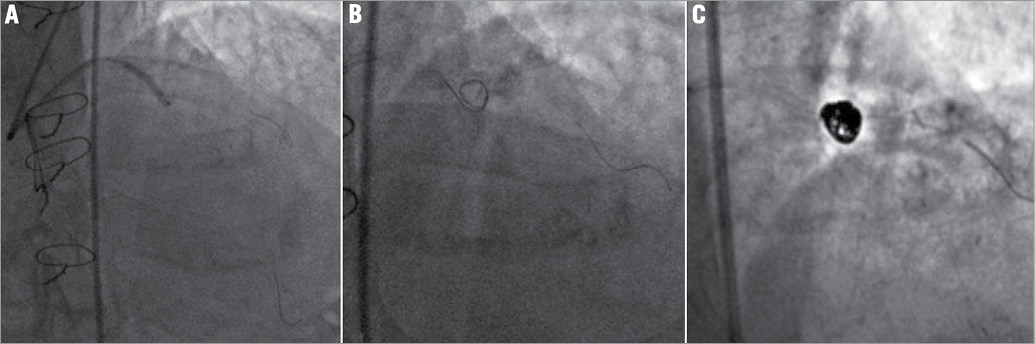
Figure 3. Bare metal stent deployment in the left anterior descending coronary artery (LAD) at the bifurcation with its first diagonal branch, which has previously been “protected” by a coronary wire (A). The coronary wires have been switched and a third wire is now rolled in the aneurysmatic sac to guide successive microcatheter advancement (B, Moving image 1). Guglielmi detachable coils are nicely packed into the aneurysm (C, Moving image 2).
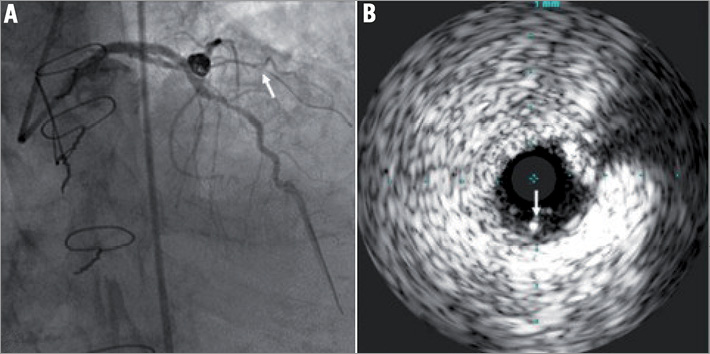
Figure 4. Right anterior oblique cranial angiography showing embolisation of the aneurysm on the left anterior descending coronary artery and occlusion of its first diagonal branch (arrow, A). Intravascular ultrasound imaging of the first diagonal branch showing a coil prolapsed into the vessel (arrow, B).
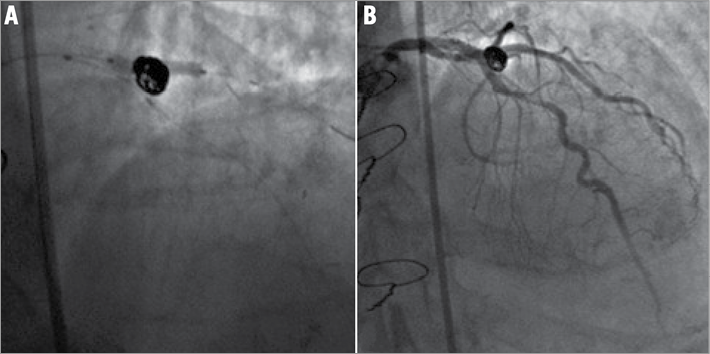
Figure 5. A second stent is deployed according to the T stenting and small protrusion technique in the first diagonal branch while a balloon is kept non-inflated in the left anterior descending coronary artery (A). Final angiographic result after completion of the percutaneous bifurcation procedure with a second stent implanted in the first diagonal branch (B).
Discussion and conclusion
A coronary aneurysm is an abnormal dilatation of a coronary artery segment to more than 50 percent of the diameter of the normal adjacent vessel7. Giambatista Morgagni first described this anomaly about 250 years ago (Figure 6).
Figure 6. Frontispiece and title page of Giovanni Battista Morgagni’s “De sedibus, et causis morborum per anatomen indagatis” (Venice, 1761) containing the first description of coronary artery aneurysms.
In the angiographic series of the CASS (Coronary Artery Surgery Study) registry comprising more than 20,000 patients, the incidence of coronary artery aneurysms was 4.9% and, in a retrospective study involving 30,000 patients who underwent coronary angiography from 1993 to 2003, coronary aneurysms conferred a five-year rate of death of 29.1%8,9. At multivariable analysis, coronary artery aneurysm was one of the strongest independent predictors of mortality (HR 1.56, 95% CI: 1.01-1.41, p=0.04)9. Also, patients with both aneurysms and CAD had a reduced five-year actuarial survival relative to patients with CAD alone (74% vs. 83%)9.
Atherosclerosis is the most common aetiology of coronary aneurysms accounting for about half of cases diagnosed in adults. The next most common cause is congenital, accounting for up to one third of cases while, in a minority of patients, inflammatory and connective tissue disorders are deemed to be associated with coronary aneurysms, as in Kawasaki disease or following implantation of first-generation drug-eluting stents10. The pathophysiology of coronary artery aneurysms is thought to be similar to that of aneurysms of larger vessels, with destruction of the vessel media resulting in increased wall stress and subsequent dilation7.
Complications of coronary aneurysms could be due to associated atherosclerosis, distal embolisation of thrombus formed due to the abnormal flow pattern in the aneurysm or rupture leading to cardiac tamponade. It has also been proposed that patients with aneurysms and angina can experience a paradoxical worsening of ischaemia after using nitroglycerine11. However, the exact incidence of these complications is unknown. Therefore, the indication for treatment and the best modalities are still debated. Significant experience has been obtained with surgery. Indeed, data from the CASS study showed no difference in survival after CABG between patients with CAD and aneurysms and CAD alone8. However, in a patient previously submitted to coronary artery bypass graft surgery, the operative risk would have been that of a re-do intervention.
More recently, different studies have reported the treatment of coronary aneurysm with polytetrafluoroethylene (PTFE) covered stents as a valuable alternative to surgery12,13. However, several limitations apply to covered stents including low flexibility, high risk of restenosis and lack of access of side branches, something which was of particular concern in our patient due to the close proximity to the aneurysm of D1 origin14.
Neuroradiologists have developed considerable experience in endovascular embolisation of intracranial aneurysms since Guido Guglielmi introduced the use of detachable platinum coils15. However, the endovascular approach to the treatment of wide-neck aneurysms remains challenging. To achieve a safe embolisation, with high packing density, stent-assisted coil embolisation has been proposed to prevent coil prolapse into the parent artery.
Moreover, coronary aneurysms involving bifurcation sites offer special challenges to interventional treatment. Ingenious solutions have been reported involving simultaneous kissing stent technique with one covered stent and one bare metal stent16 or custom-made covered bifurcation stents5.
To avoid these limitations, we successfully applied provisional Y-stent-assisted coil embolisation as an effective and modular approach allowing simple, safe and staged treatment of coronary aneurysms involving bifurcations, eventually preserving patency of both branches.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. A coronary wire is rolled in the aneurysmatic sac to guide microcatheter advancement.
Moving image 2. A Guglielmi detachable coil is embolised through a microcatheter which has been placed in the aneurymastic sac and is nicely packed into it.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. A coronary wire is rolled in the aneurysmatic sac to guide microcatheter advancement.
Moving image 2. A Guglielmi detachable coil is embolised through a microcatheter which has been placed in the aneurymastic sac and is nicely packed into it.

