Introduction
A coronary artery aneurysm (CAA), defined as a localised dilation of a coronary artery segment >1.5 times the adjacent normal coronary diameter, can often pose significant diagnostic and management challenges1. Although various percutaneous treatment modalities have been described, controversies remain regarding the indication and the optimal choice of treatment2. Covered stents used in the repair of CAAs have demonstrated excellent angiographic results. However, their inflexibility, propensity to restenosis, and side branch occlusion may limit their utility and durability in patients with CAA3.
Using double layers of stents may provide adequate coverage of the neck of the CAA by the thick mesh braided struts of the stents. This technique has been shown to be effective in the treatment of intracranial aneurysms4. Herein, we describe a case series of nine patients who underwent successful CAA closure with double layers of stent implantation at Fuwai Hospital, Beijing, China.
Methods
PATIENTS
Nine patients with CAA underwent double-layer stent implantation at our centre between 2012 and 2018. All were males; the mean age was 58.7±11.0 years. Informed consent was obtained from all patients, and the study was approved by the ethics committee of Fuwai Hospital.
DOUBLE-LAYER BARE METAL STENT (BMS) PROCEDURE
Dual antiplatelet therapy was initiated at no less than seven days before the procedure. A guidewire was passed through the body of the CAA. Balloon predilatation was performed in the stenosed coronary segment, followed by double-layer stent implantation. The key aspect of this technique is that the overlapping of the double layer of BMS covers the neck of the CAA completely (Figure 1A-Figure 1C).
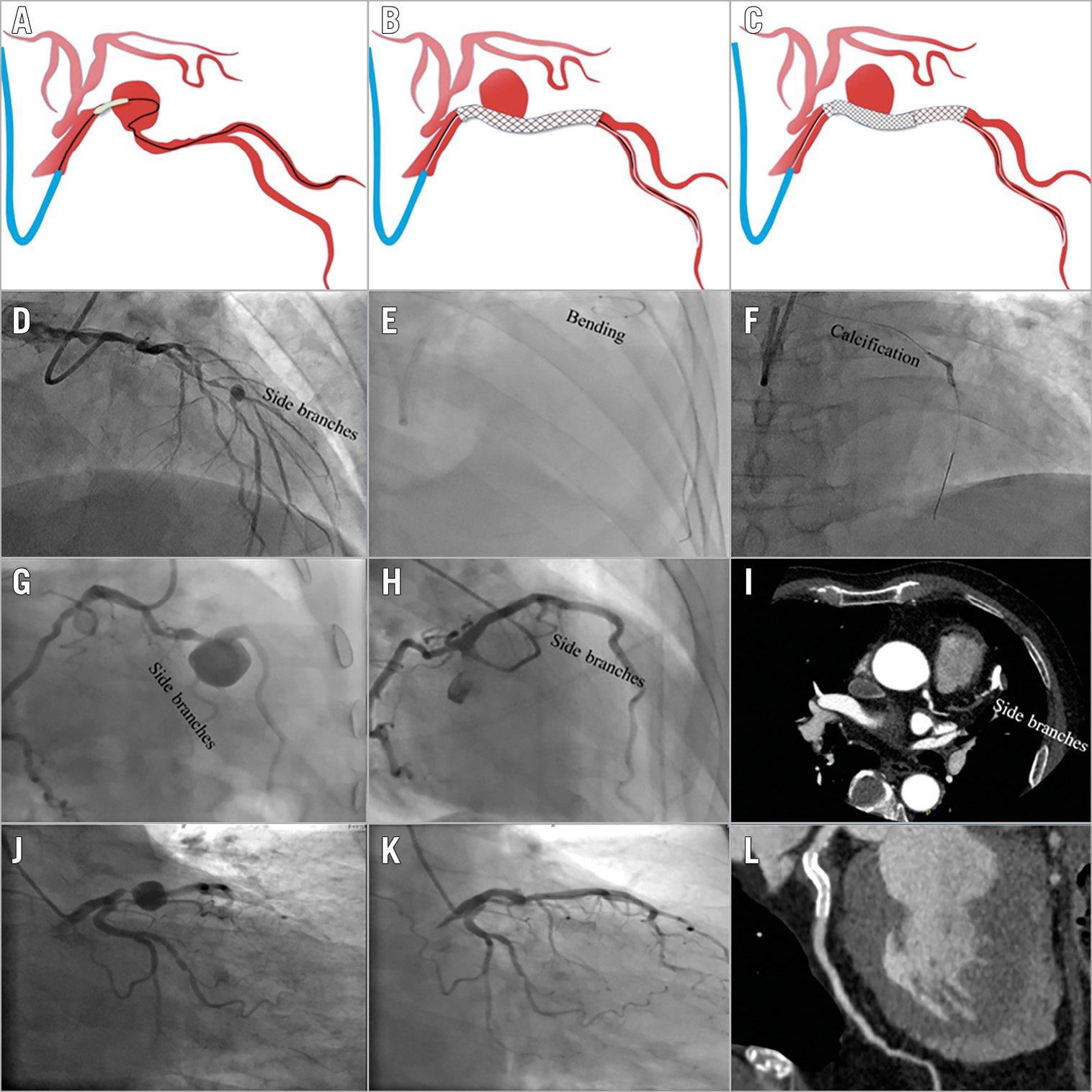
Figure 1. Double-layer BMS procedure and outcome in the CAA at six-month follow-up. A) - C) Details of the double-layer procedure. A) Predilatation of the stenosed segment. B) First bare metal stent (BMS) implantation. C) Second BMS implantation. D) Side branches adjacent to the coronary artery aneurysm (CAA). E) Vessel bending. F) Calcification evident in the proximal part of the CAA. G) & J) CAA in the left anterior descending artery. H) & K) Coronary artery angiography at the six-month follow-up. I) & L) Coronary computed tomography angiography at the six-month follow-up.
FOLLOW-UP
During the six-month postoperative period, all patients received dual antiplatelet therapy. Coronary artery angiography and/or coronary computed tomography angiography was performed according to the patient’s preference.
Results (Table 1)
Three patients had non-ST-elevation myocardial infarction and six had refractory angina pectoris. The left anterior descending artery was the most frequently affected vessel (66.7%). Features of severe stenosis in the adjacent segment (100%) and adjacent side branches (88.9%) were observed (Figure 1D), and 44.4% had bending or calcification in the coronary segment proximal to the CAA (Figure 1E, Figure 1F).
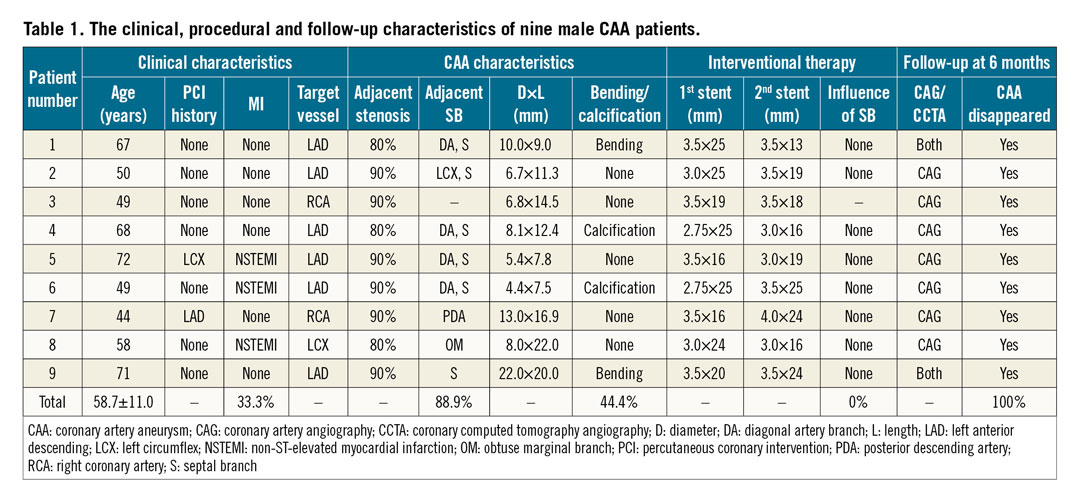
All nine patients underwent successful double-layer BMS (Coroflex®; B Braun, Melsungen, Germany) implantation without side branch occlusion.
At the six-month follow-up visit, the patients were symptom-free and excellent angiographic outcomes (Figure 1G-Figure 1L) were observed in all patients.
Discussion
This case series documents the feasibility and the efficacy of double-layer BMS implantation in treating CAA. Covered stent repair of CAA has demonstrated excellent short-term angiographic results; however, the associated disadvantages severely limit its clinical use in CAA patients. Covered stents are stiff and are delivered via large coronary guiding catheters, thereby increasing procedural complications, especially in tortuous or calcified vessels. BMS implants have better flexibility than covered stents, and are delivered one at a time, making double-layer BMS procedures in tortuous or calcified vessels easier. In addition, implantation of covered stents in CAAs has a higher rate of adjacent side branch occlusion, especially in bifurcation lesions. By individual implantation of the BMS and one-layer stent coverage of the adjacent side branch, we were able to decrease the risk of adjacent side branch occlusion.
Double-layer BMS implantation could provide a mechanical barrier to isolate the thrombosis in the cavity of ectatic coronaries and can also significantly reduce stenosis in the adjacent segment. Turbulent flow inside the aneurysm promotes mural thrombosis5, which cannot propagate inside the stent due to the opposing effect of fast-flowing blood6. Therefore, the mechanical properties of double layers of BMS could promote thrombosis in the cavity of CAAs and subsequent endothelialisation.
Limitations
In addition to the small sample size, this study suffers from the known limitations of observational studies (e.g., selection bias). In addition, its single-arm nature and short-term follow-up preclude comparative assessment with other treatment strategies for CAA. Nonetheless, these preliminary data suggest the feasibility and safety of our double bare metal stent implantation technique, which needs to be validated in further studies.
Conclusion
Double-layer BMS implantation for the repair of CAAs has a good prognosis and may be a safe and efficacious technique. We speculated that double-layer BMS have advantages over covered stents in that the delivery of the stent is easier in tortuous or calcified vessels and permits access to side branches.
|
Impact on daily practice Double-layer BMS stents might be a more promising therapeutic alternative for CAA than covered stents. |
Conflict of interest statement
The authors have no conflicts of interest to declare.