Abstract
Aims: Coronary artery aneurysms (CAA) are a rare complication after percutaneous coronary intervention (PCI) and are reported with an incidence of 0.6% to 3.9%. While in recent years the use of paclitaxel drug-coated balloons (DCB) has increased, so far no CAA formation after DCB intervention has been reported.
Methods and results: During the years 2010 and 2011 we used DCBs in 704 PCIs. Follow-up angiography was scheduled at four months in all patients and has so far been achieved in 380 PCIs. In three patients we found development of a CAA at the former PCI site within four months of observation. Aneurysm length varied between 8.4 mm and 13 mm and lumina increased 58% to 131%. Retrospectively all patients with CAA development showed small intimal dissection partially with tiny persisting contrast bands parallel to the lumen according to type B and type C of the NHLBI classification after PCI.
Conclusions: CAA formation after DCB intervention was found in three out of 380 PCIs with DCB, consistent with an incidence of 0.8%. Thus, PCI with DCB does not cause an unexpectedly high rate of coronary artery aneurysms.
Introduction
Application of paclitaxel together with a carrier substance like iopromide has been shown to reduce neointimal hyperplasia in the experimental setting1. Application of this drug combination to the site of coronary lesions via a balloon (drug-coated balloon [DCB]) has been reported in randomised trials to have major clinical benefits in bare metal stent (BMS) in-stent restenosis2,3, and in drug-eluting stent (DES) restenosis4,5, and has shown promising preliminary results in small vessels and variable benefit in bifurcation lesions6,7. Benefits have been demonstrated predominantly when used as stand-alone procedures without stenting8,9, while variability of the results has been largely attributed to different technologies leading to different tissue concentrations of paclitaxel and different clinical outcome10,11.
Paclitaxel is a highly hydrophobic agent which allows the drug to invade the arterial vascular wall substantially, where it leads to inhibition of smooth muscle cell proliferation by modulation of the microtubule formation and upregulation of proapoptotic factors12,13.
After application of a DCB, paclitaxel enters the vascular wall. Compared to DES, the acutely applied dose is considerably higher and causes tissue concentrations of paclitaxel of over 300 µg/g tissue during the first minutes14. This might promote additional pharmacologic effects as compared to paclitaxel-eluting stents which reach a tissue concentration of around 3 µg/g tissue15. While the positive effect of apoptosis in patients after percutaneous coronary intervention (PCI) is vessel enlargement (positive remodelling), the possible detrimental sequelae are wall thinning, aneurysm formation and rupture (Figure 1).
Coronary artery aneurysms (CAA) are defined as abnormal coronary dilatations exceeding the diameter of the normal segments by at least 50%16-18. The incidence of CAAs after PCI is reported as 3.9% after percutaneous transluminal coronary angioplasty (PTCA)19 and 0.6% to 1.9% after DES implantation20. There is no difference in incidence after BMS and DES implantation21,22.
While frank rupture of a coronary artery in the follow-up of DCB application has not been reported and might be difficult to prove due to acute death as a result of tamponade, we evaluated our hospital DCB registry to find out the incidence of CAA in our patients.
Methods
Since 2006 we have been performing PCI with DCB, initially for in-stent restenosis and small vessels, often combined with insertion of BMS in the treated area, but within the last two to three years also for bifurcation lesions and native coronary stenosis of small and larger vessels as a stand-alone procedure.
During the years 2010 and 2011 drug-coated balloons (DCBs) were used in 704 PCIs for treatment of in-stent restenosis (ISR), for small vessel disease, bifurcation lesions and other de novo lesions. Follow-up angiography was scheduled at four months in all patients and has so far been achieved in 380 PCIs. The indication for widespread re-angiography was the consideration of patient safety with this new technology. All data thus derived were entered into a hospital DCB registry.
In our programme we assigned all patients to DCB PCI who, after thorough preparation of the lesion by balloon or scoring balloon dilatation at a balloon to vessel ratio of 0.8 to 1.0 with 14-16 bar, had a reasonable result (according to the recommendations of the German Consensus Group23). A reasonable result was defined as a TIMI 3 flow, absence of a more than 30% residual stenosis, and either absent dissection or dissection not more than type B according to the NHLBI classification24 after PTCA. Paclitaxel was administered at a lower pressure than the initial dilatation at 8-12 bar for 30-60 seconds, carefully avoiding geographic mismatch by application of a DCB with a length extending the length of the initial dilatation on both ends by 2-3 mm. If dissection of type C or higher occurred after DCB intervention a BMS was implanted.
All angiograms were pre-screened by the operator and then discussed within the group of interventionalists as to the formation of CAA.
Results
Most PCIs could be performed according to the planned DCB-only strategy, both in ISR and in de novo lesions (Table 1).
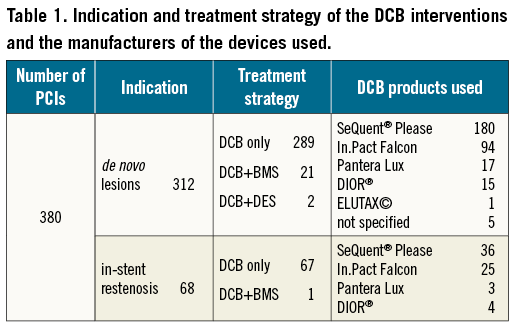
Main indications were de novo lesions, but 18% of PCIs were in ISR lesions. A DCB-only strategy was used in 356 PCIs. Twenty-four lesions were additionally treated with stents (22 BMS) for dissection type C according to the NHLBI classification24 or for recoil.
DCB interventions were performed predominantly using SeQuent® Please (B. Braun Melsungen AG, Berlin, Germany) or In.Pact Falcon (Medtronic Invatec, Roncadelle, Italy).
Restenosis in follow-up was not evaluated systematically, but seemed to be rare and largely confined to ISR. PCI site thrombosis (data on file, unpublished) was confined only to patients with the implantation of BMS after DCB or additional rotablation. However, we found a hitherto unknown complication in a few patients:
– The first patient, a 79-year-old male, presented with stable angina and three-vessel coronary artery disease with a 75% stenosis of the very small medial left anterior descending artery (LAD). After successful PTCA the lesion was treated with a SeQuent® Please (B.Braun Melsungen AG) DCB. In the follow-up angiography we found an aneurysm of 2.4 mm width and 13 mm length at the former PCI site representing a 58% diameter increase compared to the reference vessel.
– The second patient, a 58-year-old male, presented with new onset of lateral stabbing chest pain and exertional dyspnoea NYHA Class II. Angiography showed three-vessel coronary artery disease with a 75% stenosis of the obtuse marginal branch. After successful PTCA the lesion was treated with an In.Pact Falcon (Medtronic Invatec) DCB. Follow-up angiography showed a 3.6 mm wide and 8.4 mm long aneurysm at the former PCI site representing a 91% diameter increase compared to the reference vessel site.
– The third patient, an 82-year-old male, presented with exertional dyspnoea NYHA Class II and a known three-vessel coronary artery disease which had earlier been treated with coronary artery bypass grafting. Angiography revealed a 95% stenosis of the medial LAD (Figure 2). After successful PTCA the lesion was treated with a DIOR® (Eurocor GmbH, Bonn, Germany) DCB (Figure 3). Follow-up angiography showed a 6.7 mm wide and 10 mm long aneurysm of the treated segment of the LAD (131% diameter increase) (Figure 1).
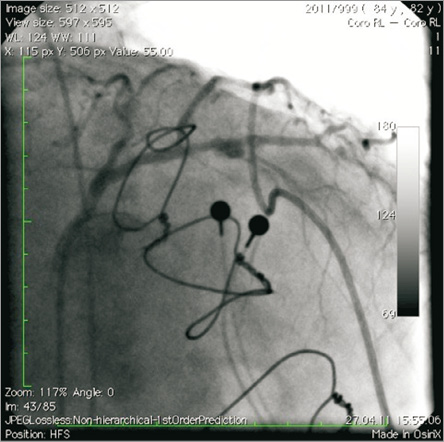
Figure 1. Left cranial view of the left coronary artery with a post-angioplasty aneurysm nearly six months after DCB application in an 82-year-old male.
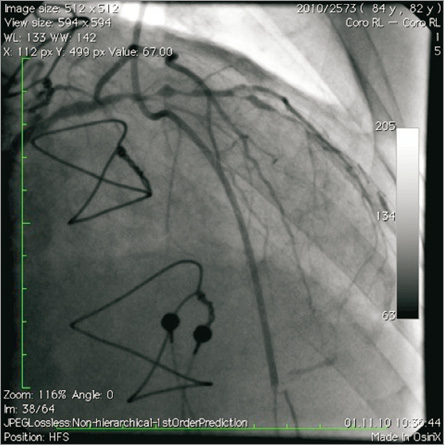
Figure 2. Before intervention the left medial coronary artery showed a de novo lesion with 95% stenosis.
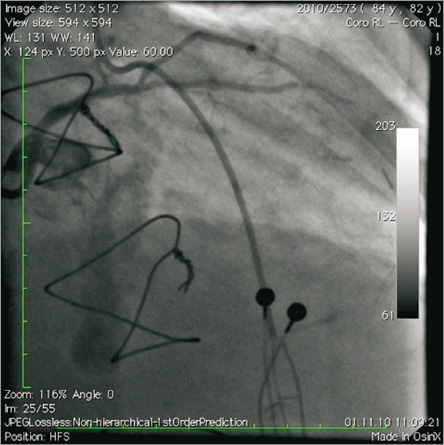
Figure 3. After treatment with a DCB-only strategy there was no residual stenosis but a tiny persisting contrast band indicating type B dissection after the NHLBI classification barely visible at the stop frame picture.
Only in these three out of 380 PCIs did we find development of a CAA at the former PCI site within four months of observation. All patients had had treatment of de novo lesions without additional stenting (DCB-only strategy). All patients stayed free of specific symptoms, and CAAs were only detected at routine angiographic follow-up. All three patients retrospectively showed small intimal dissections partially with tiny persisting contrast bands (type B and type C according to the NHLBI classification) parallel to the lumen at the end of the PCI with DCB. All were considered as unremarkable or remained undetected by the interventionalist at the end of the PCI. The lumen in the slightly dissected area increased massively from the end of PCI to follow-up and coronary diameter in the aneurysms increased by 58% to 131% of the reference diameter.
Discussion
The application of paclitaxel via DCB has been reported to have major clinical benefits in in-stent restenosis2-4 and has shown promising preliminary results in small vessels and bifurcation lesions6,25. All DCB products on the market use paclitaxel as the antiproliferative agent, mostly bound to a carrier substance like iopromide, urea, butyril-tri-hexyl-titrate (BTHC) or shellac10,26,27. However, the administration of the drug by balloon causes much higher initial tissue concentrations of paclitaxel (300 µg/g tissue14) compared to DES (3.2±1.8 µg/g tissue15). This might promote additional pharmacological effects. While positive effects like reduction of neointimal hyperplasia1 and positive remodelling are based on proliferation inhibition due to upregulation of proapoptotic factors13, possible sequelae of apoptosis might be arterial wall thinning, aneurysm formation and rupture.
In our series we found the development of three CAAs after DCB PCI. During this time we performed 704 DCB interventions and received data from 380 follow-up angiographies. Therefore, aneurysm formation after DCB intervention occurred at an incidence of 0.8%.
The likelihood of CAA formation after PCI is reported between 0.6% and 3.9%19,20 and seems to be higher in complex lesions (type B and type C2), after stenting of de novo lesions and after application of DES in chronic total occlusions (CTO)20. It is conceivable that the lower rate of CAA after DCB PTCA as compared to POBA is due to the fact that patients with high grade dissections after lesion preparation were excluded from a DCB strategy according to the current recommendations of the German Consensus Group23.
Paclitaxel is a cytotoxic drug promoting apoptosis. Apoptosis might also be the mechanism of vessel enlargement in an experimental setting, reported by Hou28, when paclitaxel is injected into the pericardial space. In this setting the increase of the space contained by the external elastic membrane (EEM) added much more to the lumen increase of the vessel as compared to the reduction in neointimal formation. While this mechanism might contribute to stabilisation or increase of lumina after PCI with DCB, there might also be a downside to this phenomenon with a slightly increased chance of CAA formation. While this could cause problems in the early phase after PCI, it is unlikely that further aneurysm development after three months will occur, since the effect of paclitaxel is of rather short duration. The presence of tiny type B and type C dissections in all our patients points to the need for careful evaluation of the result before an intervention is finished with a DCB without stenting. While DCB-only interventions (without stenting) have a lower late luminal loss as compared to stents8, the threshold of the benefits might be limited by the dissection.
Limitations
Our study has some limitations. The development of CAA was asymptomatic in all patients. Thus, there are an unknown number of aneurysm formations amongst the patients who refused the control angiogram at four months. While a rupture of aneurysms in a sizeable number of patients is highly unlikely given the good survival rates after DCB PCI10,29, the increasing procedures with application of a DCB only (without stenting) and the relatively smaller percentage of patients treated for in-stent restenosis might still conceal a higher likelihood of CAA formation than estimated by our series. These observations point to the necessity to reinvestigate angiographically patients treated with new technologies, especially to find complications with low incidences. However, it is unlikely, given the low incidence of CAA in our 380 follow-up angiographies, that our observation represents an excessive underestimation of the incidence.
Conclusion
CAA formation after DCB intervention was found in three out of 380 PCIs with DCB, consistent with an incidence of 0.8%. Thus, PCI with DCB does not cause an alarming rate of coronary artery aneurysms.
Addendum
After preparation of this manuscript an electronic report of a single CAA formation after DCB treatment was published by Vassilev D, Hazan M and Dean L. (Aneurysm formation after drug-coated balloon treatment of drug-eluting in-stent restenosis: first case report. Catheter Cardiovasc Interv. 2012;80:1223-6.)
Conflict of interest statement
F. X. Kleber and K. Bonaventura are consultants to B. Braun and received unrestricted scientific grants from B. Braun, Medtronic and Eurocor. A. Schulz and A. Fengler have no conflicts of interest to declare.

