
Abstract
Aims: This study aimed to evaluate the prognostic value of high-sensitivity C-reactive protein (hsCRP) during 10-year follow-up after percutaneous coronary intervention (PCI).
Methods and results: Between April and October 2002, hsCRP was measured in 468 all-comer patients who underwent PCI with sirolimus-eluting stent implantation for stable coronary artery disease or acute coronary syndrome. The primary endpoint was the composite of all-cause mortality or myocardial infarction at 10-year follow-up. Kaplan-Meier event curves displayed ongoing divergence of the hsCRP groups (hsCRP <1 mg/L: 14.7% vs. 1-3 mg/L: 31.1% vs. >3 mg/L: 43.1%). After adjustment for established cardiovascular risk factors and clinical presentation in a Cox regression model, higher CRP levels were associated with a higher incidence of the composite endpoint (>3 mg/L vs. <1 mg/L: HR 2.87, 95% CI: 1.69-4.87, p<0.001; 1-3 mg/L vs. <1 mg/L: HR 2.30, 95% CI: 1.31-4.03, p=0.004). Although adding hsCRP to a prediction model containing conventional cardiovascular risk factors did not significantly improve discriminatory power (area under the receiver operating characteristic curve 0.71 to 0.73, p=0.56), hsCRP was able to improve risk classification (net reclassification index=0.40, p=<0.001).
Conclusions: In patients undergoing PCI, higher CRP levels at the time of the procedure are predictive for 10-year mortality and myocardial infarction. High-sensitivity CRP may be a useful biomarker to improve further risk assessment in patients undergoing PCI.
Introduction
Chronic inflammation is considered to be an essential component in the pathogenesis and progression of atherosclerosis1-5. Increasing amounts of data have suggested a possible role for C-reactive protein (CRP) at different stages of atherogenesis and the atherosclerotic process6. CRP, a member of the pentraxin family of innate immune response proteins, is produced in the liver in response to various cytokines, such as interleukin-6, interleukin-1β and tumour necrosis factor-α7. The precise pathophysiological role of CRP in the instigation and progression of atherosclerosis remains unclear. However, this lack of current basic pathophysiological insight detracts little from the accumulating evidence indicating an association between elevated CRP levels and adverse outcome in CAD patients undergoing percutaneous coronary intervention (PCI). CRP has been associated with an increased incidence of cardiac events, including all-cause and/or cardiovascular mortality, (non-fatal) acute myocardial infarction and (urgent) revascularisation in multiple studies8-13. The majority of these results, however, derive from an era in which percutaneous revascularisation took place by plain balloon angioplasty or bare metal stent implantation. Less is known about the predictive value after drug-eluting stent implantation or about long-term follow-up. This study aimed to evaluate the prognostic value of high-sensitivity CRP (hsCRP) during 10-year follow-up after PCI in the drug-eluting stent era.
Methods
STUDY POPULATION
The design of the Rapamycin-Eluting Stent Evaluated At Rotterdam Cardiology Hospital (RESEARCH) registry has been described in detail elsewhere14. RESEARCH is a single-centre all-comers registry conducted with the main purpose of evaluating the safety and efficacy of a sirolimus-eluting stent (SES) (CYPHER®; Johnson & Johnson-Cordis, Cordis Europa NV, Roden, The Netherlands) implantation. In brief, SES implantation was used as the default strategy for all consecutive percutaneous coronary interventions between April 2002 and February 2003 in the Erasmus MC, Rotterdam, The Netherlands. High-sensitivity CRP was prospectively measured in a subset of 468 consecutive RESEARCH patients who were enrolled between April 2002 and October 2002.
ETHICS
This was an observational study. Patients were not subject to acts, neither was any mode of behaviour imposed other than as part of their regular treatment. Therefore, this study was not subject to the Dutch Medical Research Involving Human Subjects Act, and written informed consent for a patient to be enrolled was not required. This study was conducted according to the privacy policy of the Erasmus MC, according to Erasmus MC regulations for the appropriate use of data in patient-oriented research, and in accordance with the Declaration of Helsinki.
HIGH-SENSITIVITY C-REACTIVE PROTEIN
Serum samples were drawn immediately before the PCI procedure. High-sensitivity CRP (hsCRP) was determined at the Clinical Chemistry Department of Erasmus Medical Center by using a rate near-infrared particle immunoassay (IMMAGE Immunochemistry System; Beckman Coulter, Inc., Brea, CA, USA). This system measures concentrations from 0.2 to 1,440 mg/L, with a within-run precision <5% and a total precision <7.5%.
CLINICAL ENDPOINTS
As part of the RESEARCH registry, information about in-hospital outcomes was obtained from an electronic clinical database for patients maintained at our centre and by review of hospital records for those discharged to referring hospitals. Post-discharge survival status was obtained from municipal civil registries. Yearly questionnaires were sent to all living patients to obtain information on anginal status and medication use. Subsequently, hospital discharge letters were obtained and treating physicians and institutions were contacted for additional information (i.e., discharge letters and coronary angiogram) whenever necessary.
The primary endpoint of this report was the composite of all-cause mortality or myocardial infarction at 10 years of follow-up. Myocardial infarction was defined as the clinical diagnosis of ST-segment elevation myocardial infarction (STEMI) or non-STEMI. The secondary endpoint was defined as all-cause mortality at 10 years of follow-up. All endpoints were adjudicated by trained personnel.
STATISTICAL ANALYSIS
CRP levels were also categorised as low (<1 mg/L), intermediate (1-3 mg/L), or high (>3 mg/L) according to the recommendations from the Centers for Disease Control and Prevention and the American Heart Association15. Continuous variables were compared by the analysis of variance (ANOVA) test and are presented as mean±standard deviation or as median (interquartile range). Categorical variables were compared by chi-square test and are presented in numbers and percentages. Patients lost to follow-up were considered at risk for death until the date of last contact, at which time point they were censored. Cumulative event rates were estimated according to the Kaplan-Meier method. Kaplan-Meier event curves were compared by log-rank test. Cox proportional hazards regression analyses were performed to evaluate the associations between CRP and the study endpoints. In multivariable analyses, the variables age, gender, diabetes mellitus, hypertension, hypercholesterolaemia, smoking, history of myocardial infarction, clinical presentation and multivessel coronary disease were considered as potential confounders and were entered into the full model. The final results are presented as crude and adjusted hazard ratios (HR) with 95% confidence interval (95% CI). Receiver operating characteristic (ROC) curves were constructed to evaluate the supplemental value of these biomarkers for discrimination between cases and controls over conventional cardiovascular risk factors. The area under the ROC curves were compared using the method described by Hanley et al16. Additionally, continuous net reclassification improvement indices (NRI) were calculated to evaluate improvement in risk classification by the new biomarkers over conventional cardiovascular risk factors17. All data were analysed with SPSS software (SPSS 20.0, IBM Corp., Armonk, NY, USA). All statistical tests were two-tailed and p-values <0.05 were considered statistically significant.
Results
BASELINE CHARACTERISTICS
The mean age of the patients was 61±11 years and 69% were men (Table 1). Patients with diabetes (p=0.034), smokers (p=0.008) and patients with a history of myocardial infarction (p=0.001) had higher hsCRP levels (Table 2). Female patients tended to have higher CRP levels, although the difference compared to men was not statistically significant (p=0.074).
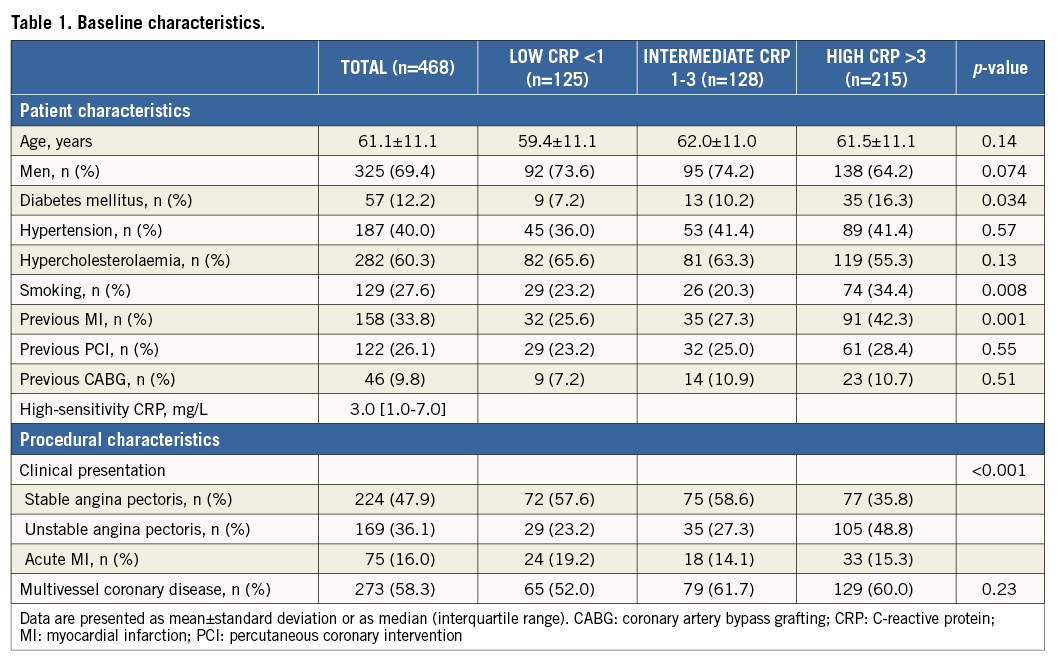
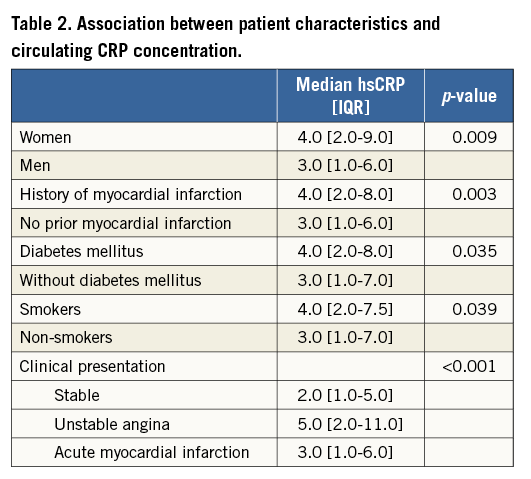
Serum hsCRP concentrations were dependent on the clinical presentation (p<0.001). Patients with stable angina pectoris (median 2.0 [1.0-5.0] mg/L) had the lowest circulating CRP concentrations. Higher hsCRP levels were observed in patients with unstable angina pectoris (median 5.0 [2.0-11.0] mg/L) and patients with acute myocardial infarction (median 3.0 [1.0-6.0] mg/L) (p<0.001).
INCIDENT EVENTS DURING FOLLOW-UP
The vital status at 10-year follow-up was acquired for 464 (99.1%) patients. The response rate of the yearly questionnaires that were sent to all living patients was at least 79% in each year. After 10 years of follow-up, 146 patients reached the composite endpoint of all-cause mortality or myocardial infarction. The Kaplan-Meier event curves displayed ongoing divergence of the hsCRP groups (hsCRP <1 mg/L: 14.7% vs. 1-3 mg/L: 31.1% vs. >3 mg/L: 43.1%) (Figure 1).
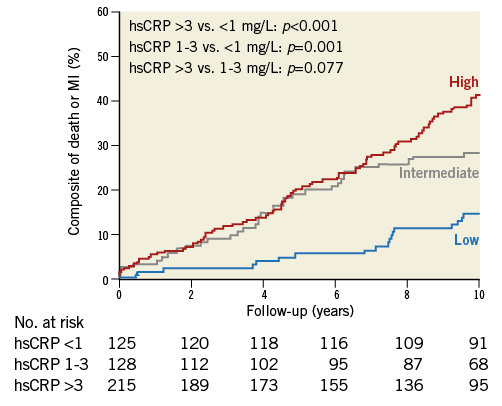
Figure 1. Prediction of cardiovascular outcome. CRP: C-reactive protein
PREDICTION OF CARDIOVASCULAR OUTCOME
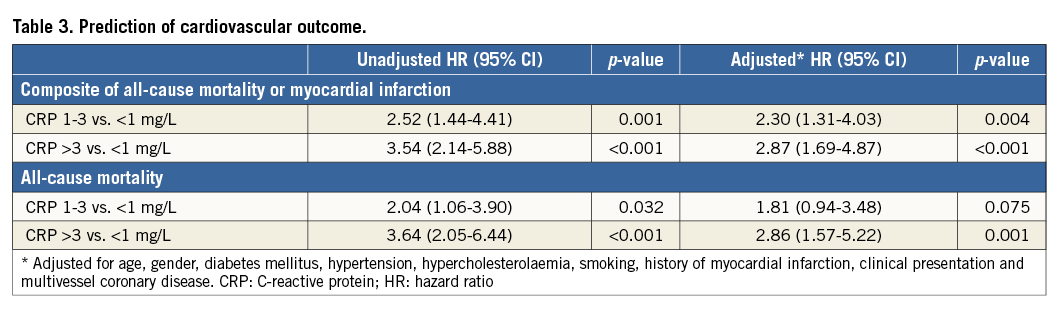
In univariable analysis, higher CRP levels were associated with a threefold increased incidence of the composite endpoint of all-cause mortality or myocardial infarction during follow-up (high vs. low hsCRP: HR 3.54, 95% CI: 2.14-5.88, p<0.001; 1-3 vs. <1 mg/L: HR 2.52, 95% CI: 1.44-4.41, p=0.001) (Table 3). The association was observed in patients admitted with ACS (high vs. low hsCRP: HR 3.64, 95% CI: 1.74-7.61, p=0.001; 1-3 vs. <1 mg/L: HR 2.80, 95% CI: 1.22-6.44, p=0.015) as well as in patients with stable angina (high vs. low hsCRP: HR 3.18, 95% CI: 1.54-6.57, p=0.002; 1-3 vs. <1 mg/L: HR 2.33, 95% CI: 1.10-4.95, p=0.028) (p for heterogeneity=0.80). Higher CRP levels were also associated with all-cause mortality only (>3 vs. <1 mg/L: HR 3.64, 95% CI: 2.05-6.44, p<0.001; 1-3 vs. <1 mg/L: HR 2.04, 95% CI: 1.06-3.90, p=0.032). After adjustment for established cardiovascular risk factors and clinical presentation, CRP levels of >3 mg/L remained independently predictive of the highest cardiovascular risk (HR 2.87, 95% CI: 1.69-4.87, p<0.001), followed by CRP levels of 1-3 mg/L (HR 2.30, 95% CI: 1.31-4.03, p=0.004) compared to CRP levels of <1 mg/L.
DISCRIMINATION
First, we evaluated a model for prediction of 10-year cardiovascular outcome which contained conventional cardiovascular risk factors, including age, gender, diabetes mellitus, hypertension, hypercholesterolaemia, smoking, history of myocardial infarction, clinical presentation and multivessel coronary disease. This model displayed an area under the ROC curve of 0.71 (95% CI: 0.66-0.76) (Figure 2). Although not statistically significant, adding CRP to this model slightly improved discriminatory ability (area under the ROC curve=0.73, 95% CI: 0.69-0.78, p=0.56).
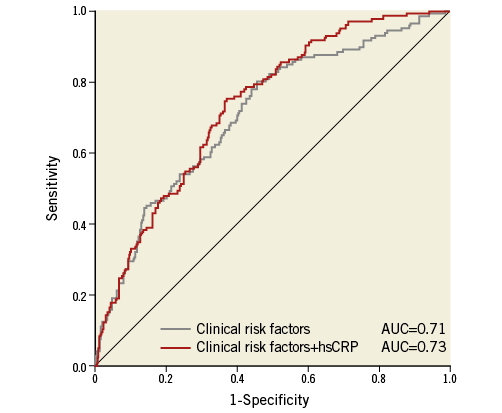
Figure 2. ROC curves displaying improved discrimination with C-reactive protein. Clinical risk factors include: age, gender, diabetes mellitus, hypertension, hypercholesterolaemia, smoking, history of myocardial infarction, clinical presentation and multivessel coronary disease. AUC: area under the curve; CRP: C-reactive protein
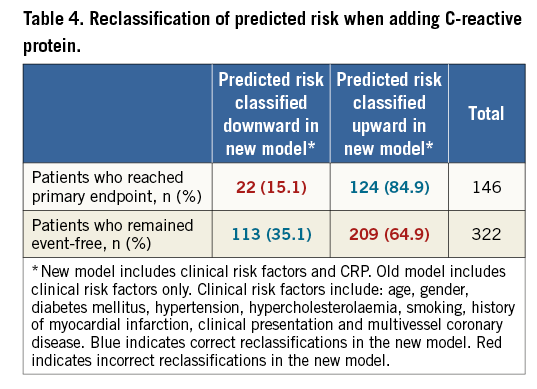
RECLASSIFICATION
We examined whether adding CRP to the model consisting of conventional cardiovascular risk factors results in correct reclassification of risk of death or myocardial infarction during follow-up (Table 4). Baseline CRP level significantly improved the risk classification (NRI=0.40, 95% CI: 0.20-0.60, p<0.001).
Discussion
This study investigated the association between circulating hsCRP concentration and 10-year cardiovascular outcome in patients undergoing PCI with drug-eluting stent implantation. The main finding is that a single baseline measurement of hsCRP is predictive for cardiovascular outcome with ongoing divergence of the survival curves until 10 years of follow-up. High hsCRP (>3 mg/L) levels were associated with a threefold increased risk for mortality and the composite of mortality or myocardial infarction, while intermediate hsCRP (1-3 mg/L) levels were associated with a twofold increased risk.
CRP is an acute phase protein and its concentration in serum reflects the inflammatory status of the patient18. Despite a lack of specificity for the cause of inflammation, many epidemiologic studies have shown significant associations between elevated serum CRP concentrations and the risk of recurrent cardiovascular events among patients with established coronary artery disease and the incidence of first cardiovascular events among individuals with cardiovascular risk factors15,19-21. However, few studies are available on the prognostic value of hsCRP in patients undergoing PCI although risk assessment at this certain time point is important and of particular interest in clinical practice. These studies have consistently shown that higher CRP levels measured at the time of the PCI procedure for both acute coronary syndrome and stable CAD are predictive of an increased long-term risk of recurrent cardiovascular events and death. For example, Park et al found that elevated CRP levels were significantly associated with an increased risk of stent thrombosis, death, and MI during a median follow-up time of 3.9 years in patients receiving drug-eluting stents22. The longest reported follow-up period is six years20,23. To the best of our knowledge, this is the first study which extends the evidence on the predictive value of CRP to 10 years after PCI.
The mechanism underlying the association of CRP with prognosis may be twofold24. Firstly, high CRP levels have previously been shown to be associated with stent thrombosis and restenosis after PCI with first-generation drug-eluting stents15,22,24. A growing body of evidence suggests that late adverse reactions to drug-eluting stents and bare metal stents may be different in relation to pathogenesis, histopathologic features, and clinical presentation24. Although less evidence is available for second-generation drug-eluting stents, Lasave et al demonstrated that elevated CRP is also associated with neointimal hyperplasia in patients who received zotarolimus-eluting stent (a second-generation drug-eluting stent) implantation25. Secondly, another underlying mechanism of the association of CRP with prognosis may be that high CRP levels are associated with coronary plaque burden and with new events in native vessels26.
Current clinical practice guidelines have indicated that measurement of hsCRP may be useful in 1) primary prevention, as an adjunct to other major risk factors for further assessment of absolute cardiovascular risk, and 2) patients with stable coronary disease or acute coronary syndromes, as an independent marker for assessing the likelihood of recurrent events, including death, myocardial infarction, or restenosis after PCI27. For the latter indication, it should be noted that secondary preventive interventions with proven efficacy should not be dependent on hsCRP levels. Furthermore, the guidelines have stated that serial testing of hsCRP should not be used to monitor the effects of treatment. The results of our study confirm that hsCRP may be a useful biomarker to assess the risk of death and myocardial infarction in patients with established coronary artery disease who undergo PCI. Furthermore, we demonstrated that only a single measurement of hsCRP at the time of a PCI procedure is sufficient to provide information on cardiovascular risk for a period as long as 10 years. The therapeutic implications of increased inflammatory status after drug-eluting stent implantation are still under investigation25. Statins are shown to have anti-inflammatory properties28. Patients with intense activation of inflammatory cells, as detected by systemic CRP levels, are likely to enjoy the highest benefit from a high-dosed statin treatment.
Limitations
Some limitations of this study need to be acknowledged. Firstly, this is a single-centre study. Caution is urged in extrapolating these results to other populations. However, other studies have shown consistent results on the long-term predictive value of hsCRP. Secondly, in this study, the prognostic value of hsCRP was evaluated in patients who underwent PCI with first-generation drug-eluting stent implantation. Caution is urged in extrapolating these results to patients with new-generation drug-eluting stent implantation or patients with coronary artery disease in general. Thirdly, the number of patients at risk at the end of the follow-up period was relatively small. However, the 10-year association was strongly significant. Finally, despite using multivariable analysis to adjust for possible confounders which may be correlated to study outcomes, we cannot exclude the possibility of residual confounding. For example, in patients who presented with myocardial infarction, time-to-presentation was not registered in our study database. In these patients, CRP levels may be affected by ongoing necrosis.
Conclusions
In conclusion, in patients undergoing PCI with drug-eluting stent implantation, high (>3 mg/L) and intermediate (1-3 mg/L) hsCRP levels are independently associated with a threefold and twofold increased risk, respectively, of mortality and myocardial infarction during follow-up. The survival curves of patients with high and intermediate hsCRP levels displayed ongoing divergence from that of patients with low hsCRP levels until 10 years after PCI, indicating that a single measurement of hsCRP at the time of a PCI procedure is sufficient to provide information on cardiovascular risk during a period as long as 10 years. Although adding hsCRP to a prediction model that contains conventional cardiovascular risk factors did not significantly improve discriminatory power, hsCRP was able to improve the risk classification over the conventional cardiovascular risk factors. Therefore, hsCRP may be a useful biomarker for long-term risk assessment in patients with established coronary artery disease and undergoing PCI.
| Impact on daily practice In patients undergoing PCI with drug-eluting stent implantation, a single baseline measurement of CRP is predictive of cardiovascular outcome with ongoing divergence of the survival curves until 10 years of follow-up. High (>3 mg/L) and intermediate (1-3 mg/L) CRP levels are independently associated with a threefold and twofold increased risk, respectively, of mortality and myocardial infarction. Furthermore, CRP was able to improve the risk classification over the conventional cardiovascular risk factors, and may therefore be a useful biomarker for long-term risk assessment in patients with established coronary artery disease and undergoing PCI. |
Guest Editor
This paper was guest edited by Adnan Kastrati, MD; Deutsches Herzzentrum München, Munich, Germany.
Acknowledgements
We would like to thank the interventional cardiologists of the Erasmus MC for their contribution to this study.
Funding
R.M. Oemrawsingh and J.M. Cheng are supported by the Netherlands Heart Foundation (grant number NHS2007B012 and NHS2009B091, respectively).
Conflict of interest statement
The authors have no conflicts of interest to declare. The Guest Editor has no conflicts of interest to declare.

