The arrival of bioresorbable vascular scaffolds (BVS) in the clinical arena was heralded by an impressive list of promises which, in the end, led to a declaration that the fourth revolution in percutaneous coronary intervention (PCI) had taken place1. The reasons for that announcement were sound: it was expected that BVS would put an end to the problem of stent thrombosis and other vascular issues associated with leaving behind a metallic cage once the stenosis had been successfully resolved.
It was a great paradox that stent thrombosis, the ultimate unmet need of metallic stents, the biggest expectation for the newcomer technology, would eventually become the very Achilles’ heel of BVS. The excess of BVS thrombosis compared to drug-eluting stents (DES) shown by most clinical trials led to disappointment, strong revision of new stent technologies and, ultimately, to the discontinuation of BVS use in clinical practice2.
But what about the many other pre-existing expectations concerning the new technology? Out of preventing stent thrombosis, other potential benefits of BVS had been framed into a concept with Promethean resonances, namely vascular restoration therapy (VRT)1. In a nutshell, resorption of the BVS might restore normal endothelial function, allow compensatory vascular remodelling (i.e., even better results of PCI in the long term), and preserve normal vasomotricity – this was VRT.
The commitment of leading investigators to demonstrating the existence of the overall concept of VRT was titanic. Without any fear of exaggeration, the intracoronary images obtained in pioneer BVS studies must be among the most thoroughly revisited and analysed medical documents in history. Therefore, it is understandable how disappointing the results of the ABSORB II trial were in this regard: at one-year follow-up, the vasomotor response to intracoronary nitrates at the target PCI site, the co-primary endpoint of the study and a key metric of VRT, was of a similar magnitude in the BVS and DES arms3.
However, the same study generated new hopes for VRT: compared to DES, and despite higher luminal loss and percent stenosis, the use of BVS was associated with better relief of angina at one-year follow-up. These striking and hypothesis-generating findings coincided in time with a small study reporting an improvement in coronary flow reserve and microcirculatory resistance immediately after BVS implantation, compared with historical DES controls4. The VRT concept was equipped with new armoury: vascular restoration after BVS occurred not only in the epicardial vessel, its salutary effects extended also to the coronary microcirculation.
Six years down the line, we have ample evidence that BVS are not more effective than DES in decreasing post-PCI angina rates: this was shown not only in the three-year results of ABSORB II, but also in the ABSORB IV trial, whose design addressed the topic in a pre-specified and rigorous manner5,6. However, the mysterious observations made at a microcirculatory level remained largely unaddressed4,7, keeping open the question – do BVS and DES have a different effect on the microcirculation and vascular function?
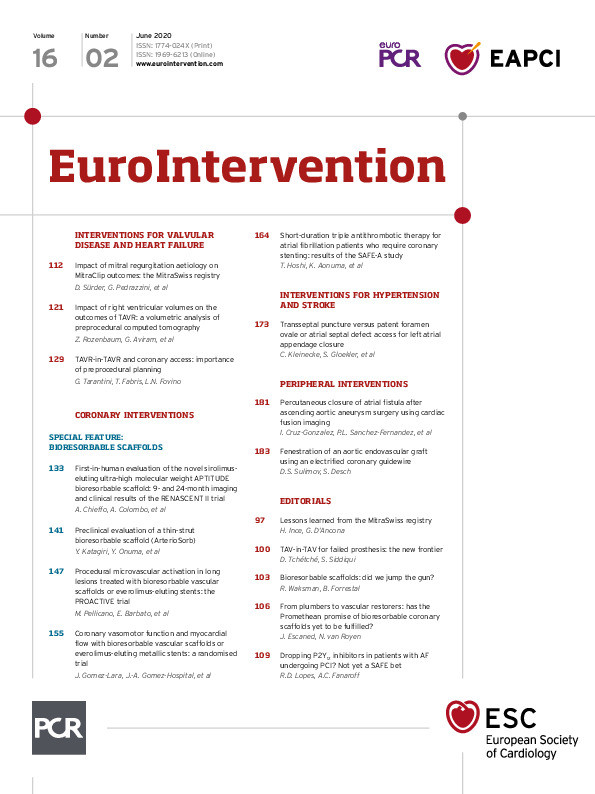
Two new randomised studies, published in this issue of EuroIntervention, provide new evidence on this topic. In the first one, the PROcedure related microvascular ACTIVation in long lEsions treated with bioresorbable vascular scaffold versus everolimus-eluting stent implantation (PROACTIVE) trial8, the investigators focused on periprocedural changes of microcirculatory resistance associated with randomly assigned implantation of BVS and DES in 66 stable patients with long (≥25 mm) coronary stenoses.
The use of BVS was associated with an unexpected acute decrease in the thermodilution-based index of microcirculatory resistance (IMR). The authors investigated whether differences in delta IMR were related to differences in cardiac enzyme leakage between the study groups: wider polymer BVS struts might become less embedded within the vessel wall (the snow-shoe phenomenon) than thinner DES ones, decreasing the chances of microembolisation, microcirculatory plugging and myocardial injury. Yet, no significant differences in high-sensitivity troponin I rise were found between the study arms.
Complementing the observations of the PROACTIVE trial, the BVS-FLOW study provides valuable information on the long-term impact of BVS and DES on vascular and microcirculatory function9.
The study enrolled 70 patients, randomly assigned to BVS or DES treatment, of whom 55 (79%) could be evaluated 13 months after PCI using intracoronary Doppler, pressure measurements and acetylcholine (Ach) testing. In the microcirculatory domain, the authors found similar values of maximal coronary flow velocity, coronary flow reserve and microcirculatory resistance in vessels treated with BVS or DES. In the epicardial vessels, Ach testing revealed similar degrees of endothelial dysfunction causing vasoconstriction in peri-scaffold and peri-DES vascular segments. Of note, vasoconstriction occurred at the in-BVS segment, but not at the in-DES segment, suggesting higher compliance and vasomotricity of BVS-treated segments. Finally, there were no significant differences in any of the components of the Seattle Angina Questionnaire between BVS- and DES-treated patients.
The authors of both studies should be commended for the solid methodology applied in their research and their valuable observations. How to interpret their findings in a combined manner? The PROACTIVE study confirmed an acute drop in microcirculatory resistance immediately after BVS implantation, something already observed in two smaller studies4,7; however, this effect of BVS on the microcirculation must be of a transient nature since, as shown by the BVS-FLOW study, metrics of microcirculatory function had similar long-term values in BVS- and DES-treated vessels. In addition to similar coronary flow reserve and maximal hyperaemic flow values, the data shown in the BVS-FLOW article (Table 4) allow calculation of similar values of long-term hyperaemic microcirculatory resistance for BVS and DES groups (1.67 and 1.75 mmHg/cm/s respectively, both well under the 2.5 mmHg/cm/s cut-off). Again, the latter observations are in agreement with long-term observations with IMR and PET in other studies7,10. This increases the likelihood that the acute reduction in IMR as compared with EES is related to intense reactive hyperaemia associated with the specific BVS implantation technique which, as documented in the study, requires mandatory BVS post-dilation, leads to longer procedural times and, potentially, causes more intense periprocedural ischaemia.
Finally, Ach testing in the BVS-FLOW study yielded, from the perspective of VRT, sweet and sour results. On the one hand, the study demonstrated preserved long-term vasomotricity of BVS-treated segments; however, on the other hand, this observation came at the expense of revealing endothelial dysfunction causing vasoconstriction in the scaffolded segment. These observations mirror those made with Ach testing in vessels treated with magnesium bioresorbable stents11.
In agreement with the ABSORB IV study, the BVS-FLOW study could not find differences in anginal symptoms between BVS- and DES-treated patients in the long term. The authors did not explore whether endothelial dysfunction was a predictor of long-term angina or cardiovascular events, most likely because the study population size would impede drawing solid conclusions.
Vascular restoration therapy, the Promethean promise of BVS, may still be an attractive concept but, in the post-ISCHEMIA trial era, the bar to demonstrate its clinical value will be even higher than before: resorbable stents or scaffolds should demonstrate either much higher safety (less stent thrombosis) or efficacy (better control of symptoms) than DES to gain widespread adoption in stable coronary disease. The latter prerequisite also seems more difficult to achieve now, as avoidance of unneeded interventions when angina has a non-obstructive origin, as an alternative to considering a different device, is emerging as a key aspect in preventing post-PCI angina12.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.