Abstract
Aims: The aim of this study was to assess the feasibility of unprotected non-ostial left main (LM) imaging by frequency domain optical coherence tomography (FD-OCT).
Methods and results: We conducted a retrospective analysis of OCT studies performed to image lesions located in the non-ostial LM. OCT studies were analysed to detect the number of artefact frames in the different LM/bifurcation segments. OCT cross-sectional images were used to assess area measures. OCT longitudinal reconstructions were used to obtain the LM length. Standard quantitative coronary angiography (QCA) was used as the reference methodology. A total of 54 patients with non-ostial LM disease entered the study. The mean number of LM artefact frames was 8±10, corresponding to 19% of the total number of LM frames analysed. The percentages of artefact frames differed significantly according to the segment analysed: 43.3% proximal LM, 11.4% mid LM and 2.1% distal LM, 1.9% ostial left anterior descending artery and 0% ostial left circumflex artery (p<0.0001). All LM OCT measurements were significantly correlated with QCA measurements.
Conclusions: The results of the present study show that FD-OCT assessment of non-ostial LM disease is feasible and may provide high-quality imaging. OCT assessment of the distal LM is more efficient than that of the proximal LM segment.
Introduction
Frequency domain optical coherence tomography (FD-OCT) is a high-resolution intracoronary imaging technique which may improve the assessment of complex coronary lesions1,2. Of note, OCT is associated with the need for full blood displacement by contrast injection so that large vessels with a proximal location (such as left main [LM]) are often considered unsuitable for this technique3.
In the present study, we sought to assess the feasibility and efficacy of FD-OCT imaging for non-ostial LM.
Methods
We retrospectively selected all patients who, between January 2010 and November 2012, underwent FD-OCT imaging in our institution for analysis of the LM and the ostia of its bifurcation branches (left anterior descending artery [LAD] and left circumflex artery [LCX]). FD-OCT images were acquired by a commercially available FD-OCT system and catheter (C7 System and C7 Dragonfly™; LightLab Imaging Inc., Westford, MA, USA, and St. Jude Medical, St. Paul, MN, USA), after coronary angiography. During image acquisition, continuous flushing of contrast medium was performed with a power injector (MEDRAD Avanta™; Siemens Healthcare, Erlangen, Germany) using a rate of 4 ml/s or (in the case of large-sized LM) 6 ml/s. FD-OCT analyses were performed off-line. The analysed regions included proximal LM, mid LM and distal LM and the ostia of its bifurcation branches (Figure 1). An example of LM FD-OCT imaging is shown in Appendix Figure 1.
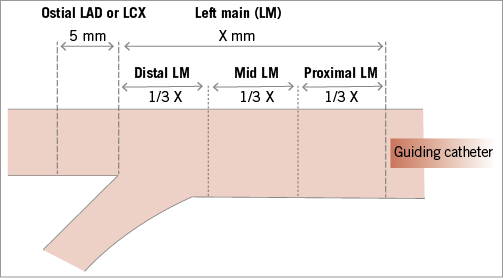
Figure 1. Schematic representation of left main (LM) coronary artery segments used for frequency domain optical coherence tomography (FD-OCT) analyses. LAD: left anterior descending artery; LCX: left circumflex artery
A detailed description of FD-OCT imaging acquisition and analysis is reported in the Appendix. Artefact frames were defined as frames where automatic minimal lumen area (MLA) calculation was not possible.
Quantitative coronary angiography (QCA) was performed off-line, using standard commercial software (CAAS QCA 5.9; Pie Medical Imaging BV, Maastricht, The Netherlands).
A detailed description of QCA and statistical analyses are reported in the Appendix.
Results
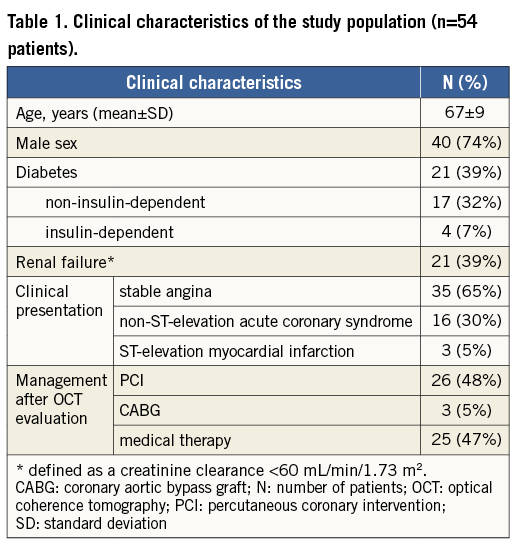
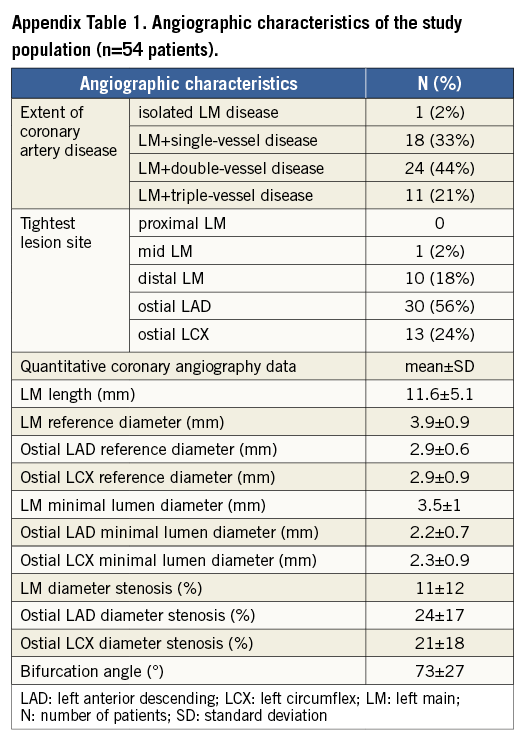
Fifty-four patients entered the study. Patient baseline characteristics are shown in Table 1 and angiographic characteristics are reported in Appendix Table 1.
A good inter-observer agreement for LM length, artefact frames, MLA and RLA was found (Appendix). The mean number of LM artefact frames was 8±10 (accounting for 19% of the total of LM frames). The number and the rate of artefact frames were significantly different across the considered LM segments (p<0.0001) (Table 2, Figure 2).


Figure 2. Percentage of artefact frames in different explored segments, p<0.0001. LAD: left anterior descending; LCX: left circumflex; LM: left main
The assessed LM FD-OCT and QCA parameters were significantly correlated (all p<0.001) (Appendix Figure 2). However, LM length as imaged by FD-OCT was significantly shorter compared with QCA (8.4±5.1 vs. 11.6±5.1 mm, p=0.001), reflecting a systematic missing of the LM ostium with FD-OCT.
Discussion
The main findings of the present study are:
– FD-OCT may be used effectively to assess non-ostial LM anatomy.
– artefacts hindering reliable LM lumen analysis by FD-OCT are substantially confined to the more proximal segments.
Quantitative analysis of the LM by coronary angiography is generally limited by vessel overlap, tortuosity and foreshortening4, although it can be improved by three-dimensional reconstructions5. OCT allows a superior lumen border detection and plaque characterisation compared to IVUS1,2, and OCT guidance for PCI is associated with favourable clinical outcomes6. With the first-generation OCT imaging system, the applicability of OCT to the specific setting of LM assessment was hindered by poor penetration and the need for proximal occlusion3. The introduction of the non-occlusive technique7 opened the way for LM assessment, but concerns about the need for guiding catheter coaxial engagement and appropriate flushing of the large LM lumen still exist. Parodi et al demonstrated that stented LM assessment by non-occlusive time domain OCT was safe and allowed for visualisation of about two-thirds of stent cross-sections8. More recently, a study comparing FD-OCT and IVUS in 35 unprotected LM patients found that the visualised lesion and/or stent length were shorter with FD-OCT9. Together with these studies, the present data collected in a larger population and using a stricter methodology (automatic MLA calculation for definition of artefact frames) support the feasibility of FD-OCT assessment of the distal LM (where artefacts are rare). On the contrary, the assessment of the proximal LM segment is limited because of systematic missing of the LM ostium and the increased rate of artefact occurrence.
| Impact on daily practice Frequency domain optical coherence tomography (FD-OCT), represents a high-resolution intracoronary imaging modality which may improve the invasive assessment of complex coronary lesions. The left main coronary artery (LM) is usually not considered suitable for FD-OCT assessment since it is a large vessel in which the complete blood displacement necessary for imaging may be challenging. In the present study, we have shown that FD-OCT imaging for non-ostial LM lesions is feasible using particular tricks like coaxial coronary intubation and appropriate contrast medium flow during scanning. Furthermore, since most artefact frames are detected in the proximal segment of LM scanning, the LM bifurcation (which is the more commonly diseased site, with complex management by stenting) is usually perfectly evaluated by FD-OCT. In conclusion, in expert centres, in clinical practice, FD-OCT may be used to evaluate non-ostial LM lesions. |
Acknowledgements
This study has been conducted by I. Dato as part of her PhD course.
Conflict of interest statement
I. Dato has received a research grant from St. Jude Medical. F. Burzotta, G. Niccoli, A.M. Leone and C. Trani received speaker’s fees from St. Jude. The other authors have no conflicts of interest to declare.
Methods
FREQUENCY DOMAIN OPTICAL COHERENCE TOMOGRAPHY IMAGING
Coronary angiography was performed via the transradial or transfemoral approach using 6 Fr sheaths and standard 6 Fr guiding catheters (XB 3 or 3.5, XB-LAD 3.5; Cordis Corporation, Johnson & Johnson, Warren, NJ, USA). Unfractionated heparin was administered during the procedure, with a target activated clotting time of >250 seconds. Intracoronary isosorbide dinitrate (2 mg) was administered before FD-OCT probe advancement into the coronary vessel. The entire length of the region of interest was scanned using the integrated automated pullback device at 20 mm/s, and FD-OCT images were acquired at 100 frames/s.
FD-OCT images were calibrated adjusting the Z-offset. This critical step was performed before image acquisition in order to obtain accurate measurements. The FD-OCT run was performed from the LAD and/or LCX, according to the operator’s preference. A double FD-OCT run from both the LAD and LCX was not routinely performed and was attempted only in selected cases, if judged necessary by the operator.
FREQUENCY DOMAIN OPTICAL COHERENCE TOMOGRAPHY IMAGING ANALYSES
FD-OCT image analysis was performed off-line by two independent investigators (I. Dato and G.L. De Maria) who were blinded to QCA data, according to the expert consensus statements10,11. For the present study, qualitative and quantitative FD-OCT analyses focused on the whole LM region. The analysed region included the whole LM (from the LM ostium or catheter tip) and the ostia of its bifurcation branches (defined as the first 5 mm of the LAD and/or LCX)12.
The LM segment was assessed for the presence of significant artefacts hindering the FD-OCT assessment. The LM segment cross-section was defined as “artefact frame” when automatic minimal lumen area (MLA) calculation was not possible. The number of artefact frames of LM segments was reported for each patient.
“LM length” was obtained from FD-OCT longitudinal reconstructions, and defined as the distance between the first distal frame of the LM at cross-sectional image and the last proximal LM frame before aorta or catheter visualisation. LM length was expressed in both mm and number of FD-OCT frames. The following parameters were obtained on cross-sectional images: the proximal and distal MLA (mm2) of the main vessel, the proximal and distal reference lumen area (RLA, mm2), and the proximal and distal main vessel percentage area stenosis (% AS=RLA–MLA/RLAx100).
QUANTITATIVE CORONARY ANGIOGRAPHY
Quantitative coronary angiography (QCA) was performed off-line by a skilled analyser (G. Pirozzolo) blinded to the results of the FD-OCT analysis, on a single, selected 2D end-diastolic image frame, according to standard protocols13,14. In particular, bifurcated vessel analysis3 was used, considering the LM as the proximal main vessel and its bifurcation branches as the distal main vessel or the side branch according to the vessel explored by FD-OCT.
Care was taken to select projections and frames with minimal foreshortening and vessel overlap, to obtain the best LM length assessment. Vessel diameters were calculated in absolute values (mm), after manual calibration with the outer diameter of the contrast-filled non-tapered part of the guiding catheter and comparison of the computed mean catheter diameter in pixels with the known catheter size in mm. For contour detection, the user indicated the vessel by choosing two centre positions proximal and distal to the stenosis. The vessel contours were automatically determined. Edge detection correction was performed if required. The reference vessel diameter was based on the computer estimation of the original arterial dimensions at the stenosis site. The following angiographic parameters were obtained for proximal and distal main vessel and for side branch: minimal lumen diameter (MLD, mm), reference diameter (RD, mm), percentage diameter stenosis (% DS) and bifurcation angle. Moreover, the length of the LM was measured and expressed in mm.
STATISTICAL ANALYSIS
Continuous variables were expressed as mean±standard deviation and compared with analysis of variance (Student’s t-test). Categorical variables were expressed as frequencies and compared using the χ2 test. Normality of data was determined using the D’Agostino-Pearson test. Correlations were calculated using Pearson’s correlation coefficient for parametric data and represented using scatter plot graphics. Inter-observer differences for FD-OCT analysis were investigated with Pearson’s correlation coefficient and Bland-Altman analysis. Statistical analyses were performed using SPSS version 17 (SPSS, Chicago, IL, USA). A two-sided p-value of 0.05 was considered significant.
Results
CHARACTERISTICS OF THE STUDY POPULATION
Overall, enrolled patients had mainly de novo lesions of unclear angiographic severity involving the LM bifurcation as testified by the visual location of tightest lesion (which, as shown in Table 1, was located mainly in the distal LM or ostial LAD/LCX). FD-OCT pullbacks for analysis of the LM and/or proximal tract of its bifurcation branches were performed through the LAD alone in 38 (70%) cases, through the LCX alone in 11 (21%) cases and through both vessels in five (9%) cases. In four cases (out of 58 attempted pullbacks, 7%), the FD-OCT pullback was repeated by the operators since the first LM imaging did not allow vessel wall and lumen assessment and was considered not acceptable for clinical purposes. These second acquisitions were used for the analyses of the present study. In STEMI patients, FD-OCT pullback was performed after thrombus aspiration which significantly reduced thrombus burden and enabled FD-OCT analysis.
FD-OCT INTER-OBSERVER AGREEMENT ANALYSES
Inter-observer agreement analysis was performed for LM length, artefact frames, MLA and RLA. Pearson correlation coefficients were: 0.99 for LM length (p<0.0001), 0.98 for artefact frames (p<0.0001), 0.90 for MLA (p<0.0001), 0.91 for RLA (p<0.0001). Bland-Altman analysis revealed that the absolute difference of number of artefact frames was 0.02 with –2.21 and 2.22 as lower and upper limits of inter-observer agreement.
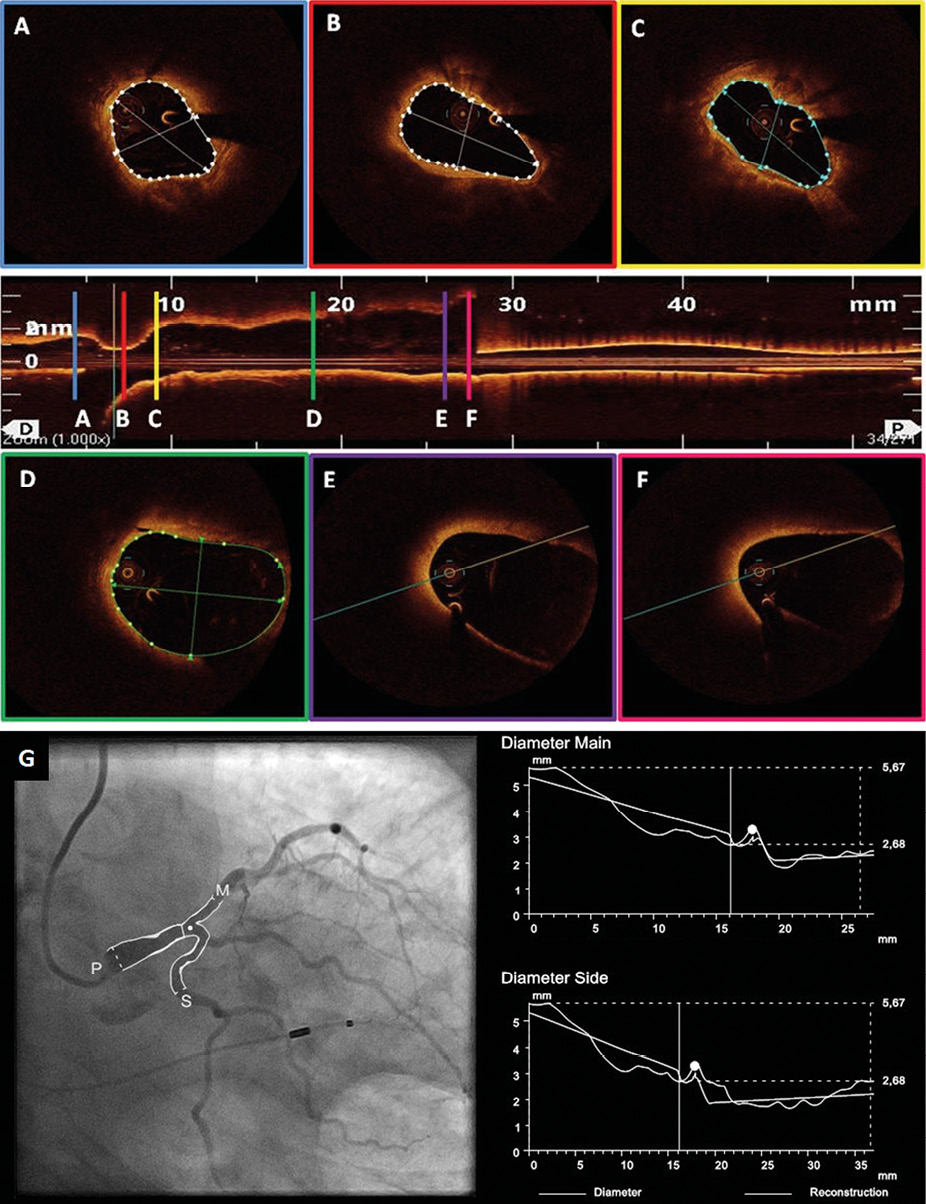
Appendix Figure 1. Frequency domain optical coherence tomography (FD-OCT) cross-sectional and longitudinal images and quantitative coronary angiography (QCA) images of left main coronary artery (LM) and ostial tract of left anterior descending (LAD) artery. In the central panel, a longitudinal FD-OCT view of the LM-LAD shows the presence of an atherosclerotic plaque of the distal LM and shows that FD-OCT analysis of the LM can sometimes not be limited by artefacts. In the upper panels, cross-sectional images of the LAD ostial tract (A), LM bifurcation (B) and distal LM (C) show a fibrolipidic plaque (minimal lumen area [MLA] 5.7 mm2, fibrous cap 50 µm) and automatic MLA measurements. In the lower panels, an FD-OCT cross-sectional image of the mid LM (D) shows a few artefacts not limiting vessel wall analysis and MLA measurement, while in the proximal LM (E, F) the “out-of-screen” phenomenon does not allow a complete qualitative and quantitative assessment of the vessel. In panel G the corresponding QCA image and analysis are shown.
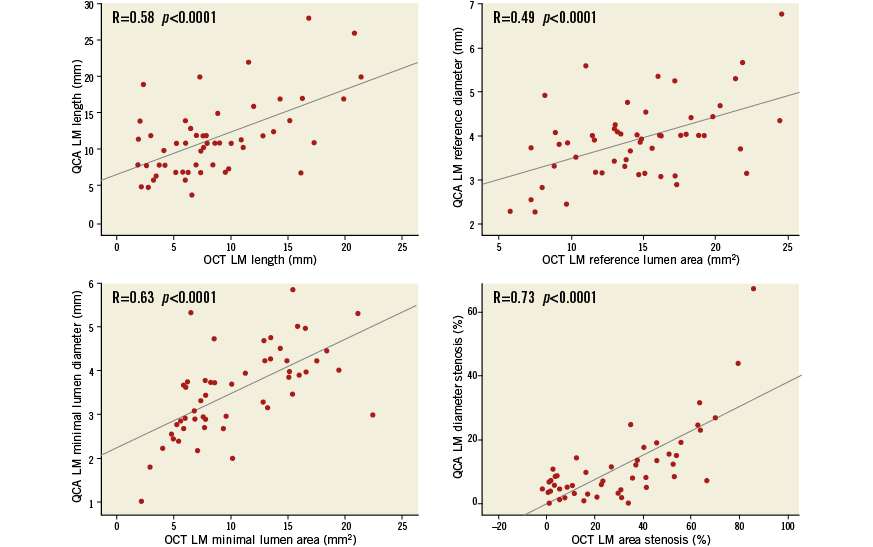
Appendix Figure 2. Scatter plots showing correlations between quantitative coronary analysis (QCA) and frequency domain optical coherence tomography (FD-OCT) left main (LM) coronary artery length (A), reference and minimal lumen measurements (B and C, respectively), and percentage of stenosis parameters (D).

