Percutaneous transluminal pulmonary angioplasty (PTPA) is performed with balloon dilatation of the target lesions in the pulmonary arteries through a catheter (Online Figure 1A-Online Figure 1C, Moving image 1, Moving image 2). We routinely perform pulmonary angiography (PAG) using a rotational digital angiography system (Artis zeego multi-axis; Siemens AG, Forchheim, Germany) before the PTPA procedure (Moving image 3). A 360-degree three-dimensional (3D) PAG image is used for identifying the target lesions and estimating their perfusion area easily and rapidly, in addition to identifying the anatomical structures of the pulmonary arteries (Figure 1A, Moving image 4). A rotational 3D PAG image can help us develop therapeutic strategies during PTPA procedures, including guide catheter and balloon size selection. Furthermore, we can visualise the pulmonary artery anatomy in synchronisation with the real-time angiographic view during the procedure, resulting in safe and easy wiring. The rotational 3D PAG image after PTPA is shown in Figure 1B and Moving image 5. Accordingly, this rotational 3D PAG image contributes to the safe and easy performance of PTPA and reduces the amount of contrast agent, leading to a reduction in radiation exposure.
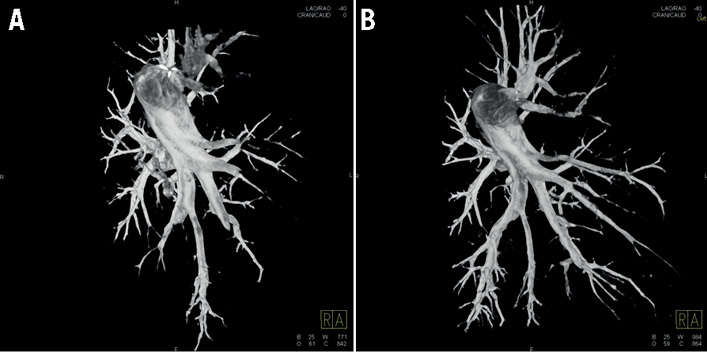
Figure 1. Rotational 360-degree three-dimensional pulmonary angiography image before PTPA (A) and after PTPA (B).
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
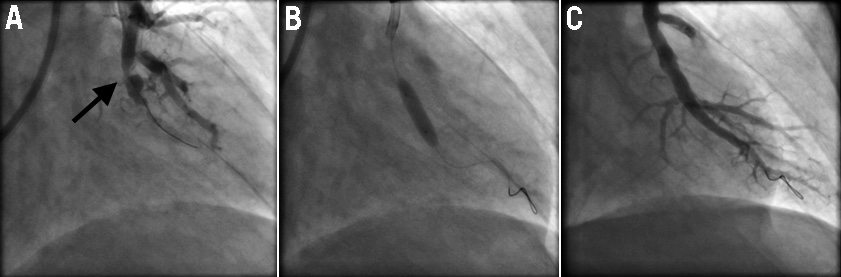
Online Figure 1. Representative angiography of percutaneous transluminal pulmonary angioplasty (PTPA). A) Angiography before PTPA. Angiography showed abrupt narrowing of the pulmonary artery. The target lesion is indicated by the arrow. B) Dilatation of the target lesions by balloon catheter. C) Angiography after PTPA. The target lesion was dilated, and the pulmonary artery was clearly visualised as far as the peripheral capillary vessels.
Moving image 1. Angiography before percutaneous transluminal pulmonary angioplasty (PTPA) demonstrating abrupt narrowing of the pulmonary artery and no visualised pulmonary veins.
Moving image 2. Angiography after PTPA demonstrating clearly visualised pulmonary artery as far as the peripheral capillary vessels and rapidly visualised pulmonary veins.
Moving image 3. Rotational pulmonary angiography (PAG).
Moving image 4. The 360-degree three-dimensional (3D) rotation PAG image before PTPA.
Moving image 5. Rotational 360-degree 3D PAG image after PTPA.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Angiography before percutaneous transluminal pulmonary angioplasty (PTPA) demonstrating abrupt narrowing of the pulmonary artery and no visualised pulmonary veins.
Moving image 2. Angiography after PTPA demonstrating clearly visualised pulmonary artery as far as the peripheral capillary vessels and rapidly visualised pulmonary veins.
Moving image 3. Angiography after PTPA demonstrating clearly visualised pulmonary artery as far as the peripheral capillary vessels and rapidly visualised pulmonary veins.
Moving image 4. The 360-degree three-dimensional (3D) rotation PAG image before PTPA.
Moving image 5. Rotational 360-degree 3D PAG image after PTPA.

