Abstract
Aims: In patients undergoing percutaneous edge-to-edge mitral valve repair for mitral valve regurgitation (MR), our aim was to evaluate acute and follow-up differences with pre-existing sinus rhythm (SR) or atrial fibrillation (AF), as well as comparisons stratified by baseline heart rate.
Methods and results: Seven hundred and sixty patients who underwent a MitraClip procedure were prospectively enrolled in the TRAnscatheter Mitral valve Interventions (TRAMI) registry, and stratified according to baseline heart rhythm and heart rate with a cut-off value of 70 beats per minute. Technical success, procedural characteristics and MR reduction were similar throughout the subgroups. Overall, in-hospital adverse event rates were low in this high-risk patient collective. At 12 months, survival was higher in SR (83.5%) than AF patients (74.9%, p<0.05), while the cumulative major adverse cardio-cerebrovascular event rate did not differ, and a sustained improvement of NYHA functional class occurred in all subgroups.
Conclusions: These registry data, comprising the largest number of unselected “real-world” MitraClip patients, suggest that the intervention can be performed safely and effectively, and reduces MR in the majority of patients irrespective of baseline rhythm or heart rate. While 12-month survival was higher for patients with SR, overall MACCE and clinical improvement did not differ between the subgroups.
Abbreviations
AF: atrial fibrillation
bpm: beats per minute
CRT: cardiac resynchronisation therapy
ECG: electrocardiogram
HR: heart rate
ICD: implantable cardioverter-defibrillator
LVEDD: left ventricular end-diastolic diameter
LVEF: left ventricular ejection fraction
MACCE: major adverse cardiac and cerebrovascular events
MR: mitral valve regurgitation
NYHA: New York Heart Association
SR: sinus rhythm
TRAMI: TRAnscatheter Mitral valve Interventions registry
Introduction
A substantial number of patients with mitral regurgitation (MR) in need of mitral valve repair are currently considered at high or prohibitive risk for conventional surgery. MitraClip® (Abbott Vascular, Santa Clara, CA, USA) therapy has emerged as an interventional treatment option for these patients, and has been successfully applied in both degenerative and functional MR1-3.
Atrial fibrillation (AF) is frequently present in patients with MR. Pre-operative AF has been reported to be a marker of increased surgical risk for MR repair or replacement4,5, although other surgical studies reported similar outcomes for AF and non-AF patients6,7. Also, mitral surgery patients with AF were older, had more comorbidities, and a more advanced disease8,9. Increased heart rate has been shown to be associated with higher cardiovascular mortality and is a cardiovascular risk indicator10-13, and raised heart rate (≥70 beats per minute [bpm]) is a risk factor in patients with stable coronary artery disease, left ventricular dysfunction and heart failure12. In addition, both AF and increased heart rate could possibly affect the feasibility and the technical challenges of the MitraClip procedure.
We herein report baseline and procedural characteristics, as well as 30-day and 12-month follow-up in a large cohort of patients who underwent a MitraClip procedure, comparing patients with sinus rhythm (SR) to those with pre-existing atrial fibrillation (AF). Also, patients with a baseline heart rate equal to or below 70 bpm (HR ≤70) are compared to those with an increased baseline heart rate of more than 70 bpm (HR >70).
Methods
PATIENT COLLECTIVE
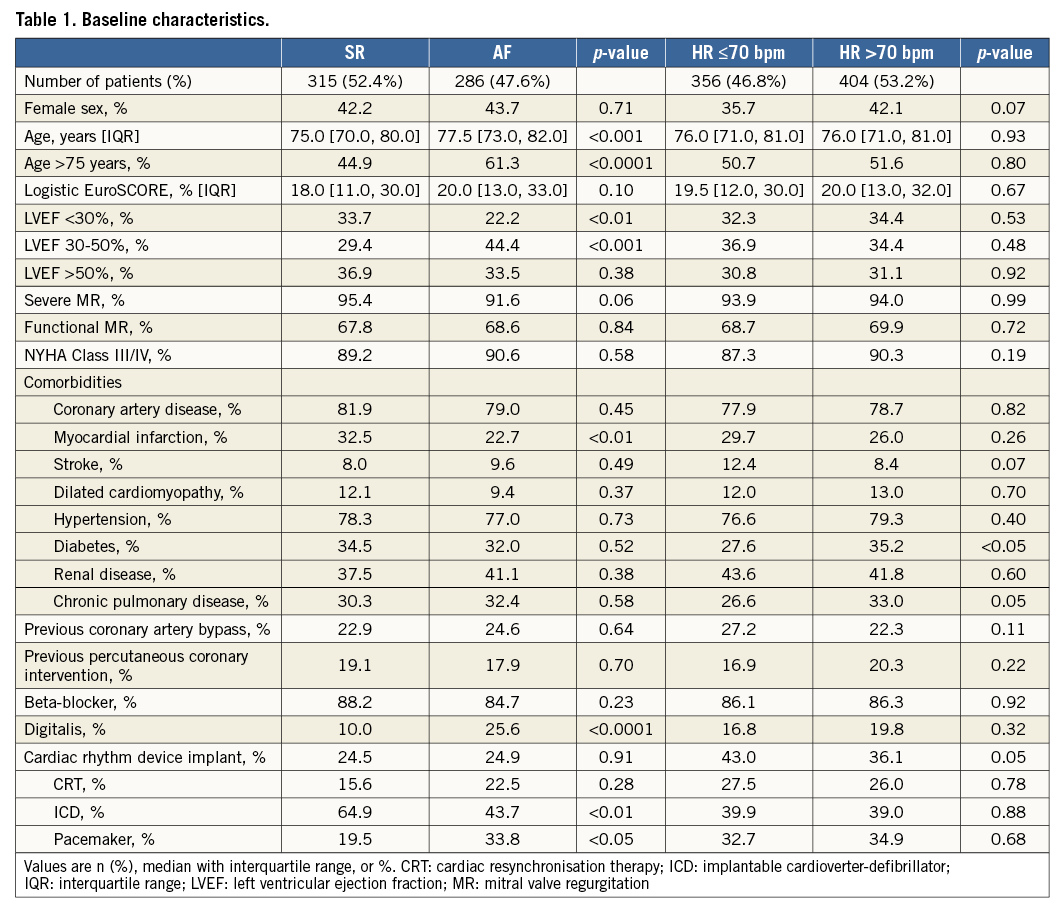
The prospective cohort of the non-randomised, investigator-initiated TRAnscatheter Mitral valve Interventions (TRAMI) registry comprises 760 patients treated with MitraClip who had been enrolled in 20 German sites. Detailed descriptions of the registry and follow-up schedule have recently been published14-16. Baseline demographics are shown in Table 1.
HEART RHYTHM AND RATE ASSESSMENT
Baseline electrocardiograms (ECGs) were analysed at each individual centre for heart rhythm and heart rate. In case of multiple ECGs on a single individual, only the first ECG recorded (baseline ECG, generally on the day of admission) was used. For all 760 (100%) prospectively enrolled patients, heart rate was known; heart rhythm was determined as AF or SR for 601 patients (79%) (Table 1), while ECGs reported as “paced” or “other rhythm” were not included in the present analysis.
MITRACLIP PROCEDURE AND MR ASSESSMENT
The MitraClip system (Abbott Vascular) received CE mark approval in March 2008, and has been commercially available in Europe since September 2008. Approval by the US Food and Drug Administration was granted in October 2013 for percutaneous reduction of degenerative MR. Device and procedural details have already been described in detail17,18. Based on current recommendations19, the severity of MR was graded as I (mild), II (moderate) and III (severe), as evaluated at each individual centre.
STATISTICAL ANALYSIS
Categorical variables are presented as absolute numbers and percentages and are compared by the chi-square test. Continuous variables are expressed as means with standard deviations or medians with interquartile ranges and are compared by the Mann-Whitney-Wilcoxon test. All tests were two-tailed, and p-values <0.05 were considered significant. SAS statistical package version 9.3 (SAS Inc., Cary, NC, USA) was used.
Results
BASELINE AND PROCEDURAL CHARACTERISTICS
A total of 760 patients who underwent a MitraClip procedure and who had been prospectively enrolled in the TRAMI registry between January 2009 and November 2013 were included in the present analysis. Patients were stratified according to i) the presence of SR or AF, and ii) heart rate with a threshold of 70 bpm. Heart rhythm was almost evenly distributed between SR and AF (52.4% and 47.6% of patients, respectively) (Table 1). While 46.8% of patients had a heart rate of ≤70 bpm (mean 62.8±6.0 bpm), an increased baseline heart rate of >70 bpm was found in 53.2% of patients (mean 84.7±13.0 bpm). Patients with pre-existing AF were older on average, more patients in SR had a history of myocardial infarction, and diabetes was more frequent in patients with increased heart rate. Approximately 2/3 of patients had a reduced left ventricular ejection fraction (LVEF). Of these, more SR patients had a severe reduction in LVEF (<30%), while more AF patients showed a moderately reduced LVEF. Accordingly, the mean baseline left ventricular end-diastolic diameter (LVEDD) was larger in SR patients (59.0 [52.0, 69.0] versus 55.0 [49.0, 61.0] mm [p<0.0001]), and 47.9% (SR) versus 35.2% (AF) of patients had an LVEDD ≥60 mm. As expected, mean left atrial diameter was larger in AF patients as compared to SR (51.0 [47.0, 58.0] versus 48.5 [44.0, 55.0] mm [p<0.001]), while echocardiographic measures of MR severity such as vena contracta width or MR jet area were similar throughout the subgroups. Baseline patient characteristics are shown in Table 1.
PROCEDURE
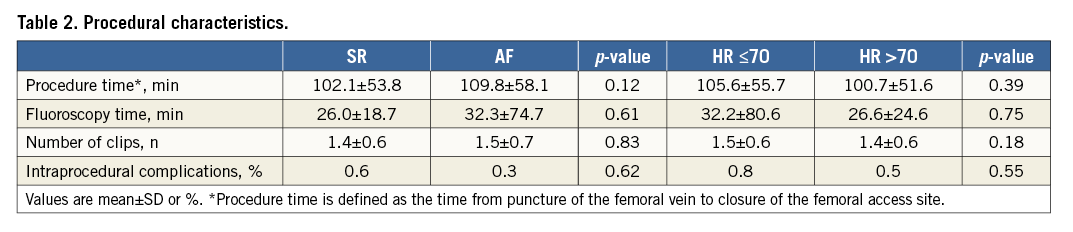
The procedural technical success rate, defined as non-severe MR after placement of the clip(s), was high (≥97.5%) for all subgroups (Figure 1A). Likewise, procedural time and the number of clips implanted were similar for all subgroups (Table 2).
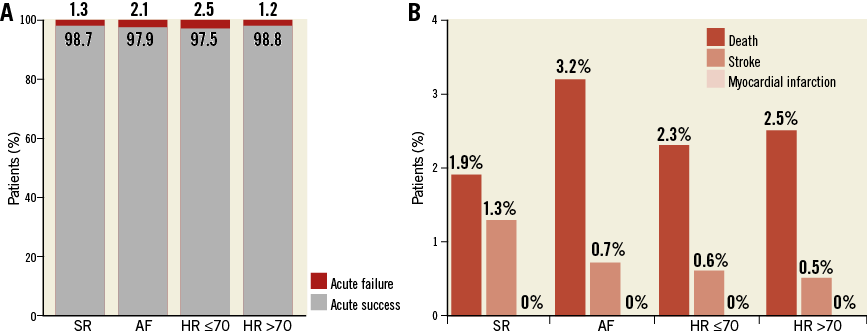
Figure 1. Procedural outcome and in-hospital major adverse cardiac and cerebrovascular events (MACCE). A) Technical success (grey) of the MitraClip procedure was high, achieved in >97% of all patients, and was independent of heart rhythm (sinus rhythm [SR], atrial fibrillation [AF]) or heart rate (stratified by a baseline heart rate threshold of 70 bpm). B) In-hospital MACCE rate (death [dark red bars], stroke [light red bars], myocardial infarction [pink bars]) was low overall and similar throughout the subgroups (p=n.s. for all comparisons).
CLINICAL AND ECHOCARDIOGRAPHIC PROCEDURAL OUTCOMES
In-hospital major adverse event rates were low overall (Figure 1B). While a comparison of the mean duration of in-hospital stay between SR and AF patients did not show any differences (9.0 [6.0, 15.0] days, p=0.77), it was shorter for HR ≤70 patients as compared to the HR >70 group (8.0 [6.0, 14.0] versus 9.0 [7.0, 15.0], p<0.05). At discharge, more than two out of three of all patients had an MR severity rating of mild or less, irrespective of initial rhythm or heart rate (Figure 2).
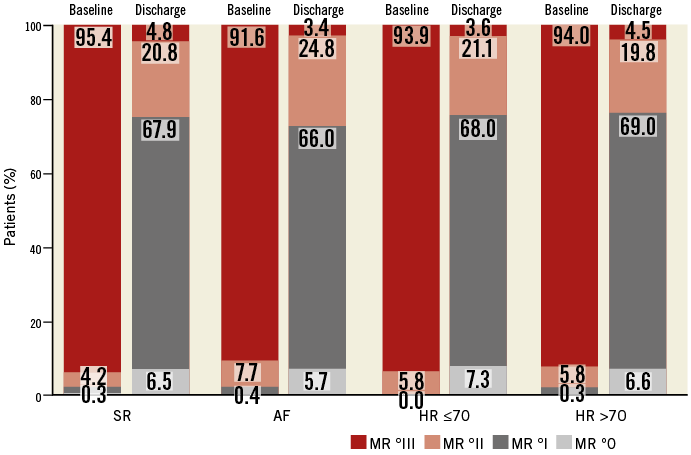
Figure 2. Mitral regurgitation (MR) severity, stratified by heart rhythm and heart rate. At baseline, as expected, the vast majority of patients were classified as having severe MR (°III, dark red bars). At discharge, MR grade in >70% of patients was equal to or less than °I, irrespective of heart rhythm or heart rate (p=n.s. for all comparisons).
FOLLOW-UP OUTCOMES
The follow-up rate was high (>95% for 30 days, >90% for 12 months), with a median follow-up time of 54 and 385 days, respectively. Cumulative mortality (in-hospital plus follow-up) was within the expected range in this high-risk patient collective: as shown in Figure 3A, cumulative 30-day mortality was 3.0 (SR), 5.8 (AF) (p=0.09), 4.3 (HR ≤70), and 4.5% (HR >70) (p=0.89), respectively (chi-square test). To address predictors of mortality in univariate and multivariate analyses, we ran Cox regression using the independent variables sex, age, baseline heart rate, left ventricular ejection fraction, diabetes and creatinine. Only creatinine >2.0 mg/dl was predictive of 30-day mortality (p=0.004; HR 2.11, 95% CI: 1.27-3.52). A second Cox analysis was run with the same parameters restricted to patients with known baseline heart rhythm; pre-existing AF did not reach statistical significance as a predictor of 30-day mortality (p=0.055; HR 1.74, 95% CI: 0.99-3.07). Figure 3B illustrates the cumulative adverse event rates for 12-month follow-up: cumulative mortality in AF patients was higher than in patients with SR at baseline (25.1 and 16.5%, p<0.05, chi-square test). Cox regression using the same independent variables as described above confirmed pre-existing AF (p=0.002; HR 1.83, 95% CI: 1.24-2.70) and creatinine >2.0 mg/dl (p=0.004; HR 1.83, 95% CI: 1.22-2.74) as predictors of 12-month mortality. The causes of post-hospital deaths are shown in Table 3. Figure 4 shows the Kaplan-Meier survival curves during 12-month follow-up. The cumulative rate of major adverse cardiac and cerebrovascular events (MACCE) (death, stroke, myocardial infarction) and re-hospitalisation rates were not different throughout the subgroups at both 30-day and 12-month follow-up (Figure 3, Table 4). As shown in Figure 3, the cumulative rate of severe bleeding events was rather high, mainly triggered by in-hospital bleeding rates of 6.5% (SR) and 8.0% (AF), respectively (p=0.48). Of note, 37.7% (SR) and 84.8% (AF, p<0.0001) of patients received anticoagulant therapy during follow-up, and antiplatelet therapy was given in 66.0% (SR) and 19.9% (AF, p<0.0001) of patients, respectively. Cumulative bleeding rates were not different in SR versus AF patients (p=0.62) (Figure 3). While severe heart failure symptoms (New York Heart Association [NYHA] Class ≥III) were frequently reported at baseline, the majority of patients had improved to an NYHA Class II or less at both 30-day and 12-month follow-up (Figure 5).
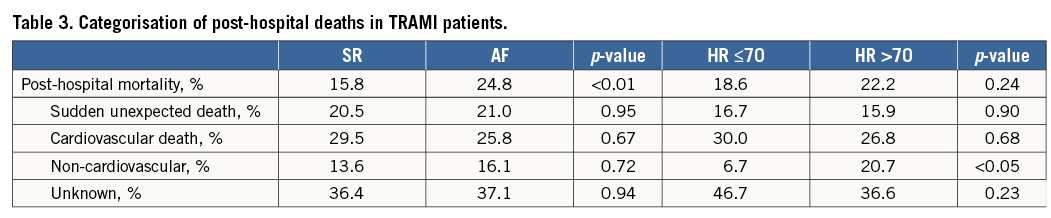
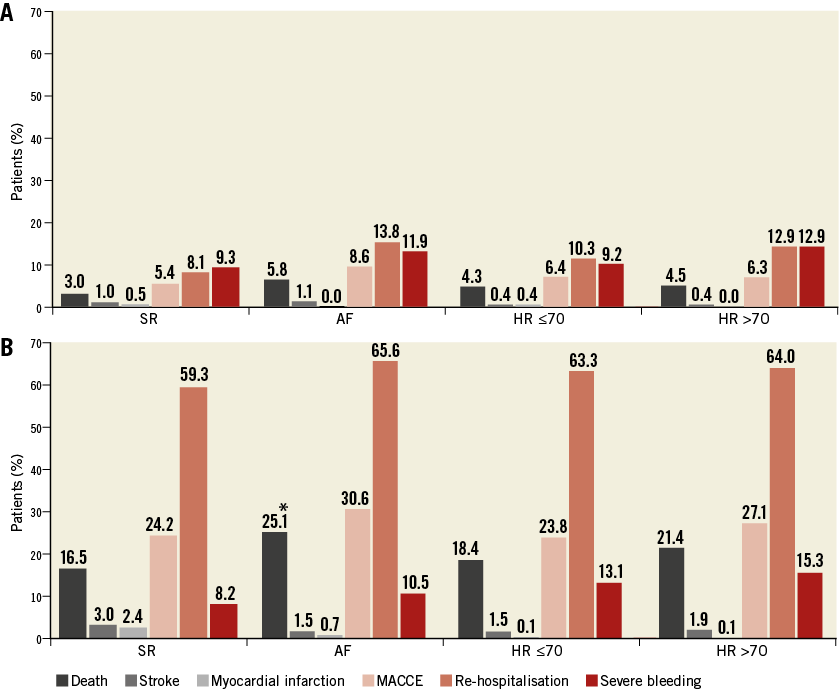
Figure 3. Cumulative MACCE, re-hospitalisation and bleeding. Cumulative incidence (in-hospital plus post-hospital) of MACCE (pink bars) at 30 days (A) and 12 months (B) as well as re-hospitalisation rates (light red bars) and severe bleeding events (dark red bars). *p<0.05 for SR versus AF; p=n.s. for all other comparisons.
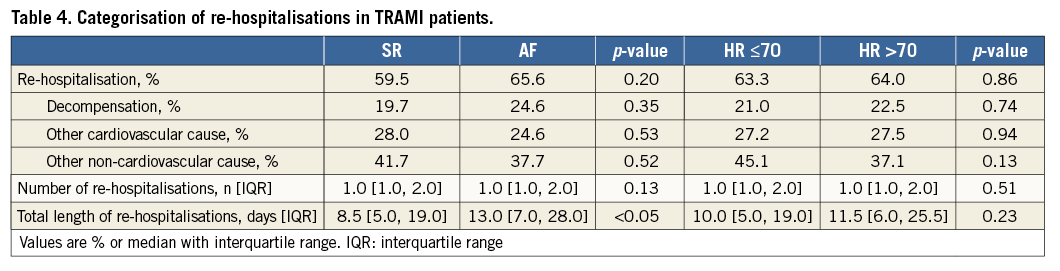
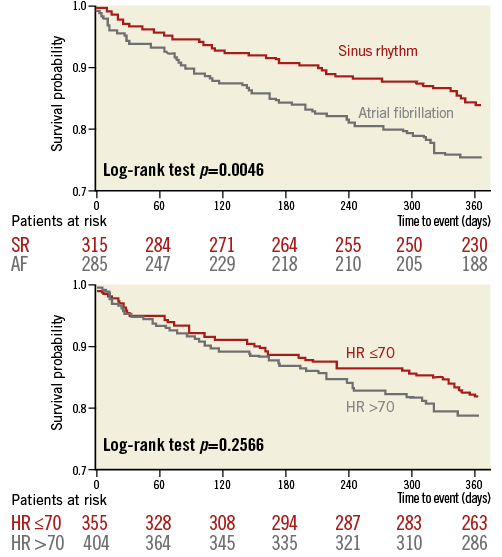
Figure 4. Kaplan-Meier curves for post-procedural survival after MitraClip implantation stratified by heart rhythm and heart rate subgroups.
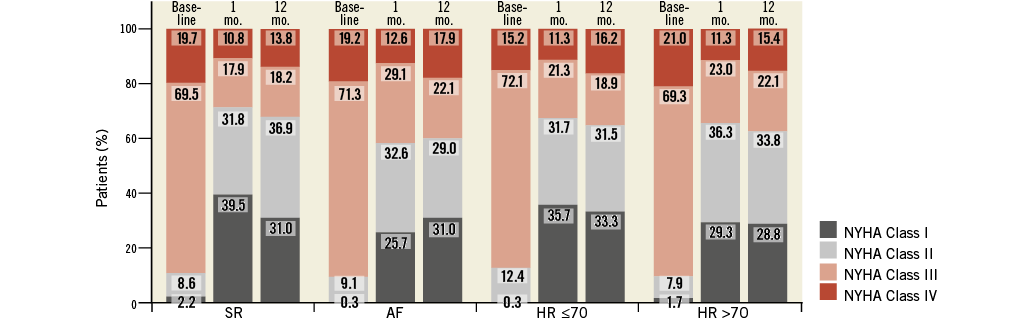
Figure 5. New York Heart Association (NYHA) functional class at baseline and follow-up. The majority of patients improved from NYHA Class III (pink bars) or IV (red bars) to NYHA Class II (light grey bars) or I (dark grey bars), independent of baseline heart rhythm or heart rate (p=n.s. for all follow-up comparisons).
Discussion
In the present analysis of the investigator-initiated TRAMI registry, we evaluated the potential effects of pre-existing atrial fibrillation on procedural, in-hospital and post-discharge outcomes of percutaneous mitral valve repair with the MitraClip system. In addition, we assessed the patient collective according to baseline heart rate.
As shown in Figure 1A, the procedural technical success rate was high, indicating the effective applicability independent of baseline rhythm or heart rate. Although the irregularity of mitral leaflet movements in AF and/or tachycardia could increase the technical difficulty for leaflet “grasping”, neither acute success rates nor procedure or fluoroscopy times (Table 2) were different within the subgroups. However, since intraprocedural heart rate and rhythm was not assessed in TRAMI, these data do not allow a definite statement regarding these putative technical challenges.
Pre-existing AF was more frequent in the patients included in TRAMI than in the EVEREST II trial, which has shown that MitraClip was associated with superior safety and similar improvements in clinical outcomes as compared to conventional surgery15-17. In contrast to EVEREST II patients20, AF in our patient collective was not associated with more advanced valvular disease or non-cardiac comorbidities (Table 1). As in EVEREST II patients20, acute procedural success, safety, and longer-term efficacy with MitraClip therapy was similar for patients regardless of the initial rhythm (Figure 1-Figure 5). Of note, patients in our TRAMI AF subgroup were on average 2.5 years older than SR patients (77.5 vs. 75.0 years, respectively), while the mean age in EVEREST II was 67.3 years. In some surgical series, pre-operative AF has even been reported to be a marker of increased surgical risk4,21. For MitraClip patients, both in-hospital and 30-day cumulative MACCE (death, stroke, myocardial infarction) rates were low throughout the subgroups (Figure 1B, Figure 3A), demonstrating the safety of the MitraClip procedure in both SR and AF patients. The mean duration of hospital stay was 9.0 days for both AF and SR patients, as well as for patients with increased baseline heart rates, while it was 8.0 days for patients with HR ≤70. In contrast, in the EVEREST II trial, patients with pre-existing AF required longer post-procedural in-hospital treatment, with AF adding 0.8 and 3.0 days to the length of stay for MitraClip and MV surgery patients, respectively20. Echocardiography at discharge demonstrated successful MR reduction to mild or less in more than 2/3 of patients (Figure 2). These results confirm findings from the EVEREST II trial, where MR reduction to ≤2 in AF patients (n=45) was similar to non-AF patients (n=130) at 83% and 75%, respectively19.
The relatively low cumulative 30-day MACCE rate in view of the high-risk patient collective (Figure 3A) again underlines the safety of the MitraClip procedure in “real-world” patients. Risk and outcomes of complications after MitraClip implantation in the TRAMI patient collective have recently been published15,16,22,23. In the present analysis, neither pre-existing AF nor baseline heart rate had an effect on overall MACCE at one- and 12-month follow-up. However, the observed 12-month cumulative mortality in AF patients was higher than in patients with SR at baseline (Figure 3B, Figure 4), which may point to effects of a generally more advanced cardiovascular disease (AF) as well as advanced age of the AF subgroup. Indeed, differences in survival rates were triggered by an increased post-hospital mortality in AF patients (Table 3).
Re-hospitalisation rates as well as severe bleeding events appeared rather high (Figure 3). Other than comorbidities (Table 1), bleeding may be in part explained by the need for antithrombotic and/or anticoagulant therapy in the majority of both SR and AF patients. However, neither bleeding nor stroke rates were statistically different in SR versus AF patients (Figure 3). Of note, the cumulative rate of severe bleeding depicted in Figure 3 comprises in-hospital and post-hospital bleeding events. By registry design, the definition of in-hospital severe bleeding comprised the need for transfusion, haemodynamic instability or intracranial bleeding22. The in-hospital rate of this bleeding endpoint was 6.5% (SR) and 8.0% (AF), respectively. Hence, pre-existing anaemia may have triggered intraprocedural or post-procedural transfusion, adding to the reported “bleeding” rate. Likewise, bleeding events represent the largest portion of MACCE in analyses of the TRAMI patient collective22,24, similar to EVEREST II patients20.
As for symptomatic improvement, the majority of patients were in NYHA functional Classes II or less at one- and 12-month follow-up (Figure 5), irrespective of rhythm or heart rate subgroup. Besides the direct haemodynamic improvements of MR reduction, this may in part also be due to a decrease in AF development. Sustained improvements of NYHA functional class were a consistent finding in TRAMI as well as other interventional mitral valve repair registries25,26.
Limitations
The registry data presented here are limited by the observational registry design. In particular, with regard to comparison of SR and AF patients, the stratification by heart rhythm in the admission ECG may be simplistic, since it cannot distinguish, for example, different types of AF and in particular may miss cases of paroxysmal AF. Also, heart rate variability in both SR and AF patients was not assessed. This may limit the conclusive interpretation of possible heart rhythm or rate effects on procedural challenges, since no intraprocedural rhythm or heart rate assessment was recorded. At this point, we do not have data on the duration of AF before enrolment or on the conversion rates to SR during follow-up. Also, success of the procedure was site-reported, without core lab echocardiographic assessment. In addition, site-reported assessment of neurological symptoms following cardiovascular interventions may well underestimate the actual rate of neurological events27. Longer-term follow-up data from the TRAMI registry will also have to assess, for example, changes in ventricular and atrial geometry and function, as well as possible effects on AF conversion. Indeed, as reported from EVEREST II, reductions in left ventricular and left atrial volumes can be expected during long-term follow-up, while the development of permanent or persistent AF after MitraClip was less common than after MV surgery20. However, in the evolving field of interventional heart valve therapy, large-scale registries that reflect “real-world” patients are of use to understand the current practice better, despite the inherent limitations of registry data acquisition.
Conclusions
In summary, these registry data, comprising the largest number of unselected “real-world” MitraClip patients, suggest that the intervention can be performed safely and effectively and reduces MR in the vast majority of patients, irrespective of baseline rhythm or heart rate. While the observed 12-month survival was higher for patients with SR at baseline, the overall MACCE rate and clinical improvement did not differ between the subgroups.
| Impact on daily practice In a “real-world” all-comers registry setting, patients who were considered as suitable candidates for interventional edge-to-edge MitraClip repair could be treated safely and effectively, with significant clinical improvement after 12 months, irrespective of baseline rhythm or heart rate. However, randomised studies to re-evaluate the possible outcome effects of atrial fibrillation and to verify the long-term efficacy of MitraClip therapy are still required. |
Acknowledgements
We thank Margot Neuser for expert graphical assistance.
Funding
The majority of funding for TRAMI is provided by proprietary means of the Stiftung Institut für Herzinfarktforschung (IHF), Ludwigshafen, Germany.
Conflict of interest statement
R. S. von Bardeleben, B. Plicht and U. Hink have received speakers’ honoraria and travel grants from Abbott Vascular. M. Puls has received travel grants from Abbott Vascular. E. Lubos has received lecture fees and grants from Abbott Vascular. H. Eggebrecht has received grant support from Abbott Vascular. The other authors have no conflicts of interest to declare.