Abstract
Aims: The aim of this study was to investigate the association between early percutaneous coronary intervention (PCI) and pneumonia risk in patients with acute myocardial infarction (AMI) by using Taiwan’s National Health Insurance Research Database (NHIRD).
Methods and results: In total, 4,732 patients with non-ST-elevation myocardial infarction (NSTEMI) and 5,465 with ST-elevation myocardial infarction (STEMI) who had received PCI during AMI hospitalisation (early PCI) were evaluated. Patients who did not receive PCI during AMI hospitalisation (deferred PCI) were matched through propensity score matching. The incidence rates (per 100 person-months) of pneumonia hospitalisation, pneumonia-related respiratory failure, and pneumonia-related death associated with early PCI in patients with NSTEMI were 0.36 (95% confidence interval [CI]: 0.32-0.42), 0.12 (95% CI: 0.10-0.16), and 0.08 (95% CI: 0.06-0.11), respectively. In patients with STEMI, the incidence rates (per 100 person-months) of the aforementioned adverse events were 0.16 (95% CI: 0.13-0.20), 0.04 (95% CI: 0.03-0.06), and 0.02 (95% CI: 0.01-0.04), respectively. After adjustment for patients’ clinical variables, early PCI was associated with reduced risks of pneumonia hospitalisation (adjusted hazard ratio [aHR] 0.54, 95% CI: 0.43-0.68, p<0.001), pneumonia-related respiratory failure (aHR 0.54, 95% CI: 0.35-0.84, p=0.006), and pneumonia-related death (aHR 0.29, 95% CI: 0.17-0.52, p<0.001) in patients with NSTEMI. In patients with STEMI, early PCI was beneficial for pneumonia hospitalisation (aHR 0.62, 95% CI: 0.45-0.86, p=0.004).
Conclusions: Early PCI might reduce the risk of pneumonia hospitalisation in patients with AMI.
Abbreviations
ACEI: angiotensin-converting enzyme inhibitor
AMI: acute myocardial infarction
ARB: angiotensin II receptor blocker
CHADS2: congestive heart failure, hypertension, age >75 years, diabetes, previous stroke
CHF: congestive heart failure
CKD: chronic kidney disease
CLD: chronic liver disease
COPD: chronic obstructive pulmonary disease
CVD: cerebrovascular disease
DM: diabetes mellitus
HTN: hypertension
NSAID: non-steroidal anti-inflammatory drug
NSTEMI: non-ST-elevation myocardial infarction
PCI: percutaneous coronary intervention
PPI: proton pump inhibitor
PS: propensity score
PSM: propensity score matching
std: standard deviation
STEMI: ST-elevation myocardial infarction
Introduction
Acute myocardial infarction (AMI), including ST-elevation MI (STEMI) and non-STEMI (NSTEMI), remains the leading cause of morbidity and mortality worldwide1. The risk of incident infections, including bloodstream infections, pneumonia, and urinary tract infections, is 79% higher in patients with AMI than in those without AMI2-4. In particular, pneumonia is a major infection in patients with AMI and can cause serious complications2-4. Furthermore, patients with pneumonia and AMI have a significantly higher rate of all-cause mortality than do those without AMI5. Therefore, strategies for preventing adverse cardiovascular events and incident pneumonia in patients with AMI are crucial.
Early and successful percutaneous coronary intervention (PCI) for patients with AMI yields lower rates of adverse cardiovascular events than medical treatment6-8; early PCI is particularly beneficial for patients with AMI with high cardiovascular risks8. However, the association between early PCI and reduced risks of pneumonia and pneumonia-related adverse outcomes in patients with AMI remains unclear.
This study investigated the association between early PCI and pneumonia hospitalisation as well as pneumonia-related adverse outcomes in patients with AMI. A retrospective cohort study was conducted using data from Taiwan’s National Health Insurance Research Database (NHIRD).
Methods
INSTITUTIONAL REVIEW BOARD, STUDY DESIGN, AND DATA SET
This retrospective population-based cohort study was conducted using data collected from the NHIRD between 2000 and 2012. Approval for the study was received by the Joint Institutional Review Board of Taipei Medical University (TMU-JIRB No. 201603074). The study data were provided by the National Health Insurance Administration of Taiwan, which covers 99% of the residents in Taiwan. Notably, the NHIRD contains the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) disease diagnosis codes; treatment procedures; claims for prescribed drugs; service dates; reimbursement amounts; the demographic information of beneficiaries; and encrypted beneficiary and provider identifiers.
STUDY POPULATION
The cohort comprised patients first hospitalised for a primary diagnosis of AMI (ICD-9-CM 410) between 2001 and 2011. The date of AMI hospitalisation was considered the index date. Among all patients, we excluded those aged <20 years, those who were not residents in Taiwan, those with a history of pneumonia (ICD-9-CM 480-486) before the index date and concomitant pneumonia during AMI hospitalisation, and those who received a diagnosis of a malignant tumour or cancer during the study period. Furthermore, we excluded patients at a high risk for pneumonia, including those who had received mechanical ventilation therapy during AMI hospitalisation9 and coronary artery bypass grafting10, ventricular assist device support11,12, extracorporeal membrane oxygenation13, splenectomy, or heart transplantation14,15 within one year of follow-up. Figure 1 presents the patient selection process. Notably, patients who had and had not received PCI at their initial AMI hospitalisation comprised the early and deferred PCI groups, respectively.
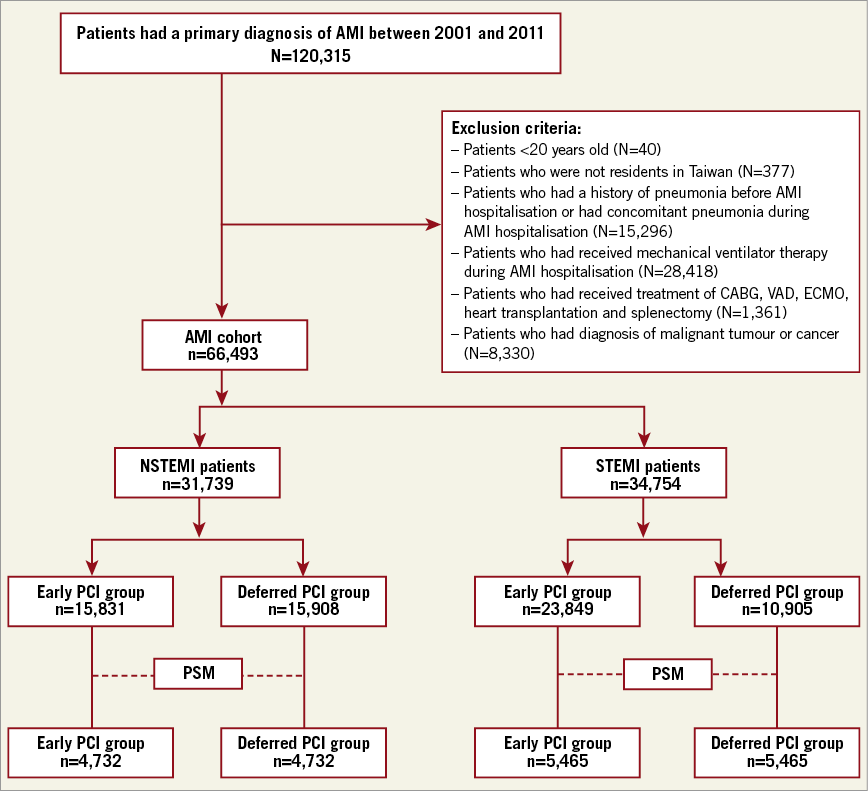
Figure 1. Flow chart of the patient selection process. AMI: acute myocardial infarction; CABG: coronary artery bypass grafting; ECMO: extracorporeal membrane oxygenation; NSTEMI: non-ST-elevation myocardial infarction; PCI: percutaneous coronary intervention; PSM: propensity score matching; STEMI: ST-elevation myocardial infarction; VAD: ventricular assist device
PROPENSITY SCORE MATCHING
To account for potential selection bias, propensity score matching (PSM) was used to select patients with AMI with early and deferred PCI who had similar baseline characteristics but a different PCI status16-19. The covariates used to calculate the score, namely age, sex, the index year, previous or present comorbidities, and drug prescriptions, are listed in Table 1.
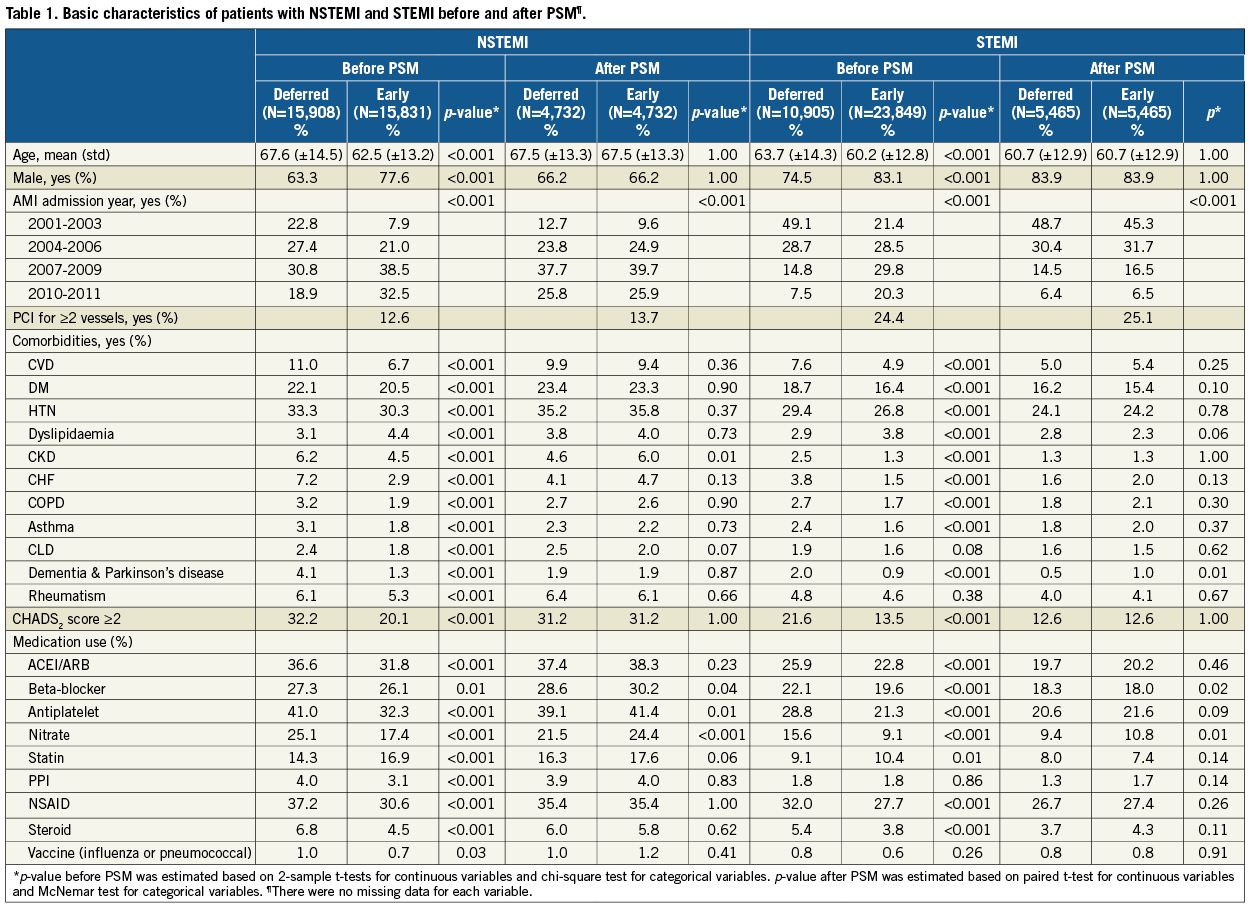
Previous or present comorbidities, namely cerebrovascular disease, diabetes mellitus (DM), hypertension (HTN), dyslipidaemia, chronic kidney disease, congestive heart failure (CHF), chronic obstructive pulmonary disease, asthma, chronic liver disease, dementia, Parkinson’s disease, and rheumatism, were recorded if the patients had ≥2 diagnostic claims in the year preceding the index date. Moreover, we calculated the CHADS2 score, which is the sum of the risk factors for CHF, HTN, DM, and stroke as well as age >75 years at MI diagnosis, and used it for patient matching20-22. The history of influenza and pneumonia vaccinations and prescribed medications, namely angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, beta-blockers, antiplatelets (including thienopyridines), nitrates, statins, proton pump inhibitors, nonsteroidal anti-inflammatory drugs, and steroids, were also considered. However, prescribed medications were only considered for matching if they were used for more than three months in the year preceding the index date.
MAIN OUTCOME MEASURES
The main outcomes were pneumonia hospitalisation (ICD-9-CM 480-486), pneumonia-related respiratory failure requiring mechanical ventilation therapy, and pneumonia-related death. Death-related data were obtained from Taiwan’s National Death Registry.
STATISTICAL ANALYSIS
A primary analysis was performed to determine the association between early PCI and the risk of main outcomes in the patients with STEMI and NSTEMI after PSM. We also performed a subgroup analysis of the patients with high cardiovascular risks (age ≥75 years and CHADS2 score ≥2). Stratified Cox proportional hazard regression was used to compare the risk of main outcomes between the early and deferred PCI groups after adjustment for the clinical variables noted in Table 1. All analyses were performed using SAS/STAT 9.2 (SAS Institute Inc., Cary, NC, USA) and Stata 12 (StataCorp LLC, College Station, TX, USA). Statistical significance was set at p<0.05.
Results
BASELINE CHARACTERISTICS
Among all of the patients with AMI, 52.3% had STEMI and 59.7% had received early PCI during AMI hospitalisation. The patients with STEMI were typically younger and had fewer comorbidities, lower CHADS2 scores, and a lower rate of medication use than did those with NSTEMI (Table 1).
Before PSM, the rate of receiving early PCI was higher in the patients with STEMI than in those with NSTEMI (68.6% vs. 49.9%). In both the STEMI and NSTEMI cohorts, the patients who had received early PCI were younger and had fewer comorbidities and a lower CHADS2 score than those who had received deferred PCI.
After PSM, 4,732 and 5,465 patient pairs were identified from the patients with NSTEMI and STEMI, respectively. The baseline characteristics were very similar in the early and deferred PCI groups (Table 1).
KAPLAN-MEIER ANALYSIS AND INCIDENCE RATES OF MAIN OUTCOMES IN THE NSTEMI AND STEMI COHORTS
In the NSTEMI cohort, the cumulative incidence rates of pneumonia hospitalisation and pneumonia-related death were lower in the early PCI group than in the deferred PCI group; similar results were found in the STEMI cohort (Figure 2). In the NSTEMI cohort, the incidence rates (per 100 person-months) of pneumonia hospitalisation, pneumonia-related respiratory failure, and pneumonia-related death were higher in the deferred PCI group (0.57, 95% confidence interval [CI]: 0.51-0.64; 0.17, 95% CI: 0.13-0.21; and 0.17, 95% CI: 0.13-0.20, respectively) than in the early PCI group (0.36, 95% CI: 0.32-0.42; 0.12, 95% CI: 0.10-0.16; and 0.08, 95% CI: 0.06-0.11, respectively). In the STEMI cohort, the incidence rates (per 100 person-months) of pneumonia hospitalisation were significantly higher in the deferred PCI group (0.22, 95% CI: 0.19-0.26) than in the early PCI group (0.16, 95% CI: 0.13-0.20) (Figure 3).
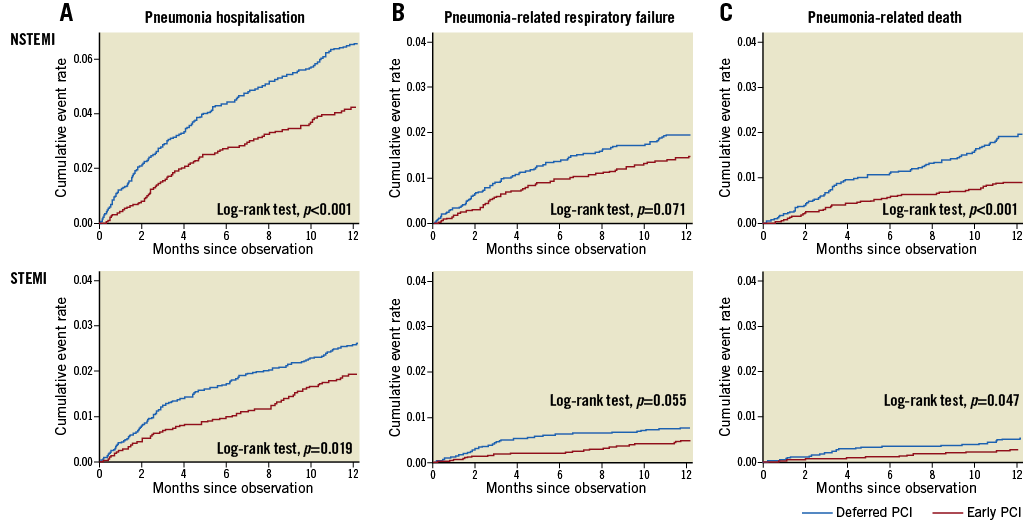
Figure 2. Kaplan-Meier curves and log-rank tests for pneumonia hospitalisation (A), pneumonia-related respiratory failure (B), and pneumonia-related death (C) in patients with NSTEMI and STEMI who had received deferred PCI versus early PCI after PSM.
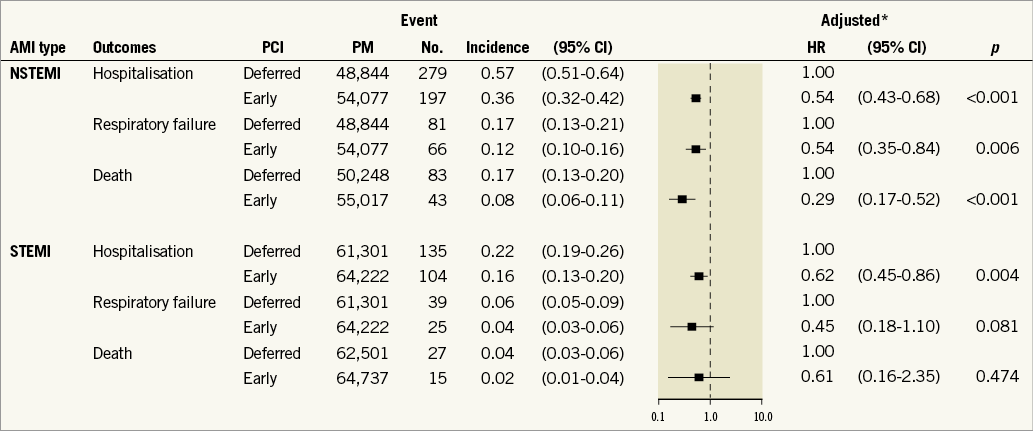
Figure 3. Incidence rates (per 100 person-months) and aHRs for pneumonia hospitalisation, pneumonia-related respiratory failure, and pneumonia-related death for patients with NSTEMI and STEMI who had received deferred PCI versus early PCI after PSM. *Results after adjustment for age, sex, the index date, previous or present comorbidities, and drug prescriptions are listed in Table 1.
EARLY PCI AND RISK OF MAIN OUTCOMES IN THE NSTEMI AND STEMI COHORTS
After adjustment for potential risk factors, we observed that, compared with deferred PCI, early PCI in the NSTEMI cohort was associated with reduced risks of pneumonia hospitalisation (adjusted hazard ratio [aHR] 0.54, 95% CI: 0.43-0.68, p<0.001), pneumonia-related respiratory failure (aHR 0.54, 95% CI: 0.35-0.84, p=0.006), and pneumonia-related death (aHR 0.29, 95% CI: 0.17-0.52, p<0.001). However, compared with deferred PCI, early PCI in the STEMI cohort was only associated with a reduced risk of pneumonia hospitalisation (aHR 0.62, 95% CI: 0.45-0.86, p=0.004) (Figure 3).
SUBGROUP ANALYSIS
Among the patients with a CHADS2 score of ≥2, the incidence rates of pneumonia hospitalisation (aHR 0.44, 95% CI: 0.30-0.63, p<0.001), pneumonia-related respiratory failure (aHR 0.35, 95% CI: 0.12-0.96, p=0.041), and pneumonia-related death (aHR 0.15, 95% CI: 0.05-0.45, p=0.001) were lower in the early PCI group than in the deferred PCI group in the NSTEMI cohort. In the STEMI cohort, early PCI was associated with a lower risk of pneumonia-related death than was deferred PCI, with an aHR of 0.31 (95% CI: 0.11-0.86, p=0.025). Similar results were obtained when the analysis was limited to the patients aged ≥75 years (Figure 4).
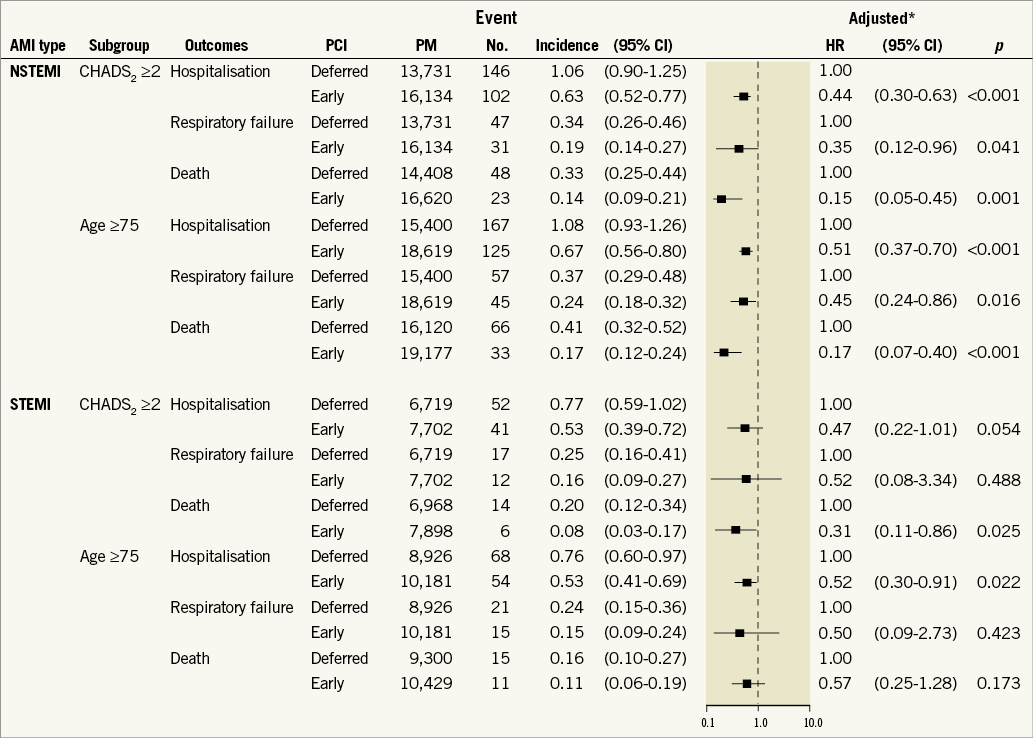
Figure 4. Subgroup analysis of incidence rates (per 100 person-months) and aHRs for pneumonia hospitalisation, pneumonia-related respiratory failure, and pneumonia-related death for patients with NSTEMI and STEMI who had received deferred PCI versus early PCI after PSM. *Results after adjustment for age, sex, the index date, previous or present comorbidities, and drug prescriptions are listed in Table 1.
Discussion
Our nationwide database comprised not only medical centres but also non-PCI-capable hospitals in Taiwan. Thus, our findings probably represent real-world data and indicate that many patients with AMI did not receive early PCI. Potential reasons for the delay between AMI and PCI include the lack of adherence to American College of Cardiology Foundation/American Heart Association guidelines, lack of implementation of quality improvement programmes, and suboptimal awareness of invasive cardiac procedures6,23.
Previous studies, as well as the present study, have reported the underutilisation of early PCI among patients with NSTEMI and high cardiovascular risks24-27. This may occur because the risk profiles of patients are perceived to increase the risks and complications associated with invasive procedures26-29. Moreover, patients with advanced age and comorbidities who develop AMI are more likely to present with atypical symptoms rather than typical chest pain6,7. Therefore, early PCI following the successful diagnosis of AMI in such patients is typically postponed6,7. Another possible reason is that STEMI is often recognised as a more concerning AMI type because it is associated with higher in-hospital mortality rates than NSTEMI, thus leading to substantial efforts to provide early PCI at presentation8,27.
Pneumonia places a considerable burden on healthcare resources and society, mainly because of hospitalisation and lost working days30,31. Studies have identified several risk factors for pneumonia and pneumonia-related adverse events, including advanced age, CHF, diabetes, and asthma30,31. These factors are particularly crucial for patients with NSTEMI because they typically develop the aforementioned comorbidities, as was also observed in the present study. Early PCI can be performed to reduce the risk of adverse cardiovascular events; it might also reduce the risks of pneumonia and pneumonia-related outcomes in patients with AMI, as noted herein.
Several mechanisms might explain our findings. CHF and physical limitations after AMI have been proposed to result in impaired inspiratory function; diaphragm neuromuscular alterations; intrinsic myocyte abnormalities32,33; and subsequent adverse events, including limited alveolar ventilation, impaired airway clearance, and sympathetic activation, which increase the risk of pneumonia, cardiac arrhythmias, and haemodynamic instabilities32. However, early PCI can reduce the risk of post-MI HF and improve the ability to engage in physical activities after AMI34,35, and it might have contributed to the benefits observed in the present study.
Patients with acute coronary syndrome(s) (ACS) with a CHADS2 score of ≥2 had significantly increased rates of 30-day and 10-year mortality21. In addition, the rates of hospital mortality attributable to an ACS were considerably higher in elderly patients than in younger patients36. Studies have suggested the following strategies to improve the utilisation of PCI in patients with AMI with high cardiovascular risks and to avoid the delay in PCI: 1) educating and improving the patient’s awareness of symptoms to shorten the delay between symptom onset and first medical contact, 2) establishing rapid assessment protocols to identify high-risk patients, 3) improving the patient’s understanding and acceptance of invasive coronary intervention, 4) enhancing the physician’s adherence to guidelines, and 5) increasing the availability of catheterisation laboratories and PCI-capable hospitals6,7,23.
Study limitations
First, the NHIRD does not have certain patient information, such as that on tobacco use and ambulatory status, which might be associated with the incidence of pneumonia. Second, the NHIRD does not contain some clinical information, such as the angiographic findings of PCI, extent of a patient’s coronary artery disease, and severity and pathogen of pneumonia. Consequently, we could not identify the most common pathogen in patients with pneumonia. Third, the PS only considered the observed variables; therefore, hidden bias was possible. Moreover, PSM must have reduced the external validity of our study because only a subset of the treated patients was analysed. However, despite its limitations, PSM was an acceptable approach because the findings of observational studies with PSM are moderately consistent with those of randomised clinical trials19,37,38. Fourth, we could not further define the patients with primary PCI based on the population-based health insurance claims. Finally, this study was conducted using a cohort of Taiwanese patients and therefore the results might not be generalisable to other populations. Future prospective, randomised studies on the effects of early PCI are warranted to confirm our findings.
Conclusions
In this population-based PSM cohort study, the patients with NSTEMI and STEMI with early PCI had a lower risk of pneumonia requiring hospitalisation than did those with deferred PCI; these results are consistent with those for high-risk patients. Our findings suggest that early PCI significantly prevents pneumonia requiring hospitalisation.
| Impact on daily practice Early PCI may reduce the risk of pneumonia requiring hospitalisation not only in patients with NSTEMI, but also in those with STEMI. |
Acknowledgements
This study was supported by the Health and Clinical Data Research Center of Taipei Medical University.
Conflict of interest statement
The authors have no conflicts of interest to declare.